Sinusitis, Nasal Polyps, and Otitis Media
Ricardo A. Tan
Jonathan Corren
I. SINUSITIS
A. Definitions and epidemiology
The paranasal sinuses are air-filled cavities that exist within the facial and skull bones that are lined with columnar epithelium and connect to the nasal passages via small openings called ostia. Sinusitis refers to inflammation in the paranasal sinuses, which is most commonly infectious in origin. The infectious etiology can be viral, bacterial, or, less frequently, fungal. Thirty-one million Americans have been estimated to suffer from chronic sinusitis, and patients lose an average of 4 days of work per episode.
Acute sinusitis usually lasts up to 4 weeks, while chronic sinusitis is defined as symptoms persisting beyond 12 weeks. Recurrent acute sinusitis is defined as three or more separate episodes of acute sinusitis per year.
Chronic rhinosinusitis (CRS) is a more recently coined term that reflects the concurrent involvement of both the paranasal sinuses and nasal passages, which is frequently present in many patients with sinus disease. CRS may occur with associated nasal polyps, without nasal polyps, or as a syndrome called “allergic fungal sinusitis.”
B. Pathogenesis
1. Acute sinusitis. When the ostia of any of the sinuses become obstructed, the environment within the cavity becomes anaerobic, leading to the development of a more acidic pH and retention of mucus. These changes may lead to bacterial growth and infection. Maxillary and ethmoid sinusitis are most common, while the sphenoid sinus is infrequently affected.
2. Chronic sinusitis. The sinus tissue and mucus from patients with CRS without nasal polyps usually contains a preponderance of eosinophils and neutrophils. The pathophysiology of this form of CRS is poorly understood but may involve some predisposing condition, such as chronic rhinitis (either allergic or nonallergic), an anatomic defect (e.g., septal deviation), or immunodeficiency. In addition, sensitization of Th2 lymphocytes to colonizing fungi (e.g., Alternaria) with subsequent eosinophil infiltration has been proposed to play a possible pathogenic role in CRS without nasal polyps.
In CRS with nasal polyposis, there is evidence for local production of specific IgE antibodies against staphylococcal enterotoxins, which act as superantigens and activate large numbers of lymphocytes. Patients with CRS without nasal polyps do not appear to produce these antistaphylococcal enterotoxin IgE antibodies. A role for Th2 fungal sensitization with eosinophilic tissue and mucus infiltration may also contribute to the pathogenesis of CRS with nasal polyps.
Allergic fungal sinusitis (AFS) represents allergic sinus inflammation caused by fungal colonization and is associated with “allergic mucin.” Allergic mucin ranges in color from light tan to brown to dark green and contains large numbers of degranulating eosinophils and microscopically identifiable fungal hyphae. Allergic mucin is usually not seen during routine physical examination and is most often identified during surgery. Over time, patients with AFS may develop sinus cavity opacification and sometimes local pressure effects on bone. Bony demineralization of the sinus wall may ensue, resulting in expansion of the sinus and possibly mucocele formation. Patients with AFS usually have nasal polyposis, are immunocompetent, and have evidence of fungal-specific IgE by skin tests or IgE immunoassays.
C. Clinical presentation
1. Acute sinusitis. Acute sinusitis most commonly presents as a persistent “cold” that lasts for more than 7 to 10 days. Nasal congestion, sore throat, cough, or postnasal drip may be present during the preceding viral infection but increase in severity as sinusitis develops. Purulent nasal discharge or postnasal drip, headache, facial pressure aggravated by bending over, teeth pain, or pain between the eyes signify that acute bacterial sinusitis may have developed. Low-grade fever and generalized malaise may occasionally be present.
On physical exam, tenderness over the sinuses or over the upper teeth may be noted. Anterior rhinoscopy may show purulent secretions, but their absence does not rule out sinusitis. Fiberoptic rhinoscopy can directly visualize the drainage of pus from the ostia of the sinuses, especially in the middle meatus. Topical decongestants may aid in diagnosis by shrinking the turbinates and allowing the ostia to be visualized.
2. Chronic sinusitis. Patients with chronic sinusitis commonly present with two or more of the following symptoms: nasal obstruction, facial pain or fullness, anterior or posterior drainage, or decreased sense of smell. Chronic sinusitis is less obvious by history and indeed is often missed as symptoms are attributed to other conditions. Occasional patients may also present with only a single long-standing and refractory symptom such as cough, purulent postnasal drip, headache, or halitosis with no other associated symptoms. Facial pain or fullness, if present, is not as intense as in acute sinusitis. Decreased or absent sense of smell is often associated with nasal polyps. In addition to the above symptoms, chronic sinusitis can also cause worsening of asthma.
Physical examination often shows turbinate swelling and erythema, whereas sinus tenderness is rarely found. Purulent discharge may be seen near the sinus ostia or nasal passages, but, as noted in the case of acute sinusitis, its absence does not exclude the diagnosis of chronic sinusitis. Nasal polyps may be present and appear as pale, blue-hued growths often emanating from the area medial to the middle turbinate. Fiberoptic rhinoscopy may be helpful in visualizing polyps or purulent discharge.
D. Diagnostic tests
1. Plain films. Acute sinusitis is usually treated based upon clinical suspicion. However, in occasional patients presenting with atypical symptoms, a Waters’ view plain film may be obtained to confirm maxillary or frontal sinusitis. Opacification, air-fluid levels, and moderate-to-severe
thickening have all been shown to correlate with positive bacterial cultures taken from the maxillary sinuses in patients with acute sinus symptoms; the most predictive finding is an air-fluid level. Waters’ view films may also be useful in young children with atypical chronic symptoms (e.g., chronic cough) to evaluate possible maxillary sinusitis. When ordering plain films in children, it should be kept in mind that the maxillary and ethmoid sinuses are present on x-rays from birth, while the frontal sinuses cannot be visualized until age 3 to 7 years and the sphenoid sinuses around age 9 years. In general, plain films are insensitive for detecting moderate amounts of mucosal thickening and are very ineffective at imaging the ethmoidal air cells, making it a poor study for patients with suspected chronic sinusitis.
thickening have all been shown to correlate with positive bacterial cultures taken from the maxillary sinuses in patients with acute sinus symptoms; the most predictive finding is an air-fluid level. Waters’ view films may also be useful in young children with atypical chronic symptoms (e.g., chronic cough) to evaluate possible maxillary sinusitis. When ordering plain films in children, it should be kept in mind that the maxillary and ethmoid sinuses are present on x-rays from birth, while the frontal sinuses cannot be visualized until age 3 to 7 years and the sphenoid sinuses around age 9 years. In general, plain films are insensitive for detecting moderate amounts of mucosal thickening and are very ineffective at imaging the ethmoidal air cells, making it a poor study for patients with suspected chronic sinusitis.
2. Computed tomography (CT) scan. The CT scan is considered the gold standard for diagnosing sinus disease. Sinus CTs are most appropriately performed in patients with suspected chronic sinusitis who are still symptomatic despite having received a prolonged trial of medical therapy. A limited-cut, four-slice CT scan of the sinuses is a very cost-effective and adequate alternative to a full CT scan. It can show the ethmoid sinuses in detail and provide some visualization of the osteimeatal complexes in the maxillary sinuses.
3. Magnetic resonance imaging (MRI). MRI is especially useful in differentiating inflammatory from neoplastic processes by the signal intensity of their T2-weighted images. Malignant tumors have an intermediate bright signal, while infectious inflammation shows a high signal intensity on T2-weighted images. The main disadvantage of MRI is its limited delineation of bone. Imaging of the ethmoid sinuses is also limited because normal cycles of mucosal swelling cannot be easily distinguished from pathologic swelling. Although the MRI is more sensitive than the CT scan for detecting soft tissue inflammation, the CT scan is sensitive enough for diagnosis in most cases.
4. Ultrasound. Sinus ultrasounds are rarely used because of false-positive rates of 39% to 45% and false-negative rates of 42% to 56%. Presently, ultrasound is not considered sensitive enough to substitute for radiographic imaging.
5. Sinus culture. Cultures of nasal secretions do not accurately reflect sinus microbiology because of frequent bacterial colonization of the nasal passages. Middle meatal aspiration uses a thin plastic tube to aspirate discharge from the ostium in the middle meatus and provides a meaningful culture result. Maxillary sinus punctures are more invasive and no longer commonly done. Sinus cultures are indicated only in complicated (e.g., sinus abscess) and refractory cases with significant systemic symptoms.
E. Microbiology
In acute bacterial sinusitis, the organisms most commonly responsible are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. In chronic sinusitis, Staphylococcus aureus, coagulase-negative staphylococci (S. epidermidis), Group A streptococcus, Pseudomonas aeruginosa, and anaerobic bacteria such as Fusobacterium and Bacteroides can also be involved. In cystic fibrosis, the most common organism is P. aeruginosa.
Invasive fungal sinusitis is most commonly, but not exclusively, seen in immunocompromised patients such as those with chronic diabetes or
malignancy or who are receiving chronic treatment with immunosuppressants. Aspergillus fumigatus is the most common organism seen regardless of an individual’s immune status. Candida, Sporothrix, Schizophyllum, Mucor, Bipolaris, Alternaria, and Curvularia can also be found. AFS has been shown to be caused by Aspergillus, Bipolaris, Dreschlera, and Curvularia species.
malignancy or who are receiving chronic treatment with immunosuppressants. Aspergillus fumigatus is the most common organism seen regardless of an individual’s immune status. Candida, Sporothrix, Schizophyllum, Mucor, Bipolaris, Alternaria, and Curvularia can also be found. AFS has been shown to be caused by Aspergillus, Bipolaris, Dreschlera, and Curvularia species.
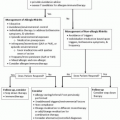
F. Medical therapy
1. Antibiotic therapy. Antibiotics are the mainstay of the treatment of acute sinusitis or recurrent acute sinusitis (Table 5-1), as well as infectious exacerbations of chronic sinusitis (Table 5-2). As S. pneumoniae, H. influenzae, and M. catarrhalis are the most common organisms cultured in all of the above conditions, amoxicillin remains a good first-line choice. Acute sinusitis should be treated for 10 to 14 days and for at least 7 days beyond the first day of marked improvement. For example, if a patient did not feel significantly better until the seventh day of antibiotics, they would receive a total of 14 days of therapy. For patients with significant penicillin allergy, sulfamethoxazole-trimethoprim is an efficacious and cost-effective alternative first-line treatment. In some geographic regions, at least 30% to 40% of H. influenzae and 75% to 95% of M. catarrhalis produce beta-lactamase. If this is a significant concern, amoxicillin-clavulanate or second-generation cephalosporins (e.g., cefuroxime) are cost-effective options. In patients with penicillin allergy, macrolides (e.g., clarithromycin) and fluoroquinolones (e.g., levofloxacin, moxifloxacin) are good alternatives.
Adult patients with chronic sinusitis and purulent nasal secretions should be treated with 3 to 6 weeks of antibiotics, depending upon the response to treatment, and a good first choice for these patients is amoxicillin-clavulanate or clarithromycin in penicillin-allergic patients. If first-line treatment with either of these medications is not effective, a trial of clindamycin or metronidazole may be useful.
If methicillin-resistant S. aureus is identified, the patient’s regimen should include clindamycin, trimethoprim-sulfamethoxazole, or linezolid.
If methicillin-resistant S. aureus is identified, the patient’s regimen should include clindamycin, trimethoprim-sulfamethoxazole, or linezolid.
Table 5-1 Conditions Associated with Sinusitis | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree