Fig. 2.1
(Left) X-ray of left femur showing subtrochanteric fracture and lytic lesion. (Right) X-ray of left distal femur showing lucent lesions (arrows)
Her hypercalcemia was treated with aggressive intravenous fluid administration, subcutaneous calcitonin, and zoledronic acid 4 mg. Her calcium level normalized. An ultrasound of the neck showed a solid mass encompassing the left lobe of the thyroid with sonographic features of malignancy. Parathyroid hormone (PTH) was 1510 pg/mL (15–65 pg/mL), and 25-hydroxyvitamin D was undetectable. The thyroid-stimulating hormone (TSH) level was 3.5 mIU/L (0.3–5.0 mIU/L). Fine-needle aspiration (FNA) of the neck mass was positive for neoplastic cells with Hürthle cell features.
Assessment and Diagnosis
The most likely diagnosis for a patient presenting with a pathologic fracture, lytic bone lesions, and severe hypercalcemia is widespread malignancy. The presence of a neck mass would also be consistent with a malignancy. The cytology of FNA does not prove or disprove malignancy. Although thyroid cancers such as follicular, medullary, or anaplastic thyroid carcinoma can metastasize to the bone, they are not generally associated with hypercalcemia. The profound elevation of PTH indicates a PTH-mediated hypercalcemia. The findings of severe hypercalcemia, significant elevation of PTH, and a neck mass are highly suspicious for parathyroid carcinoma [1–3]. Cytologic features alone on FNA cannot distinguish thyroid and parathyroid tissue nor parathyroid carcinoma from benign parathyroid tissue.
Lytic bone lesions are a common finding when widespread malignancy metastasizes to the bone and also in multiple myeloma which can also result in severe hypercalcemia. Osteitis fibrosa cystica is a skeletal disorder with lytic bone lesions related to hyperparathyroidism. Although rarely seen in the USA today, it occurs in severe long-standing primary hyperparathyroidism and parathyroid carcinoma. The proliferation and activity of osteoclasts in response to PTH leads to cystic defects that can produce pain and be locally aggressive, resulting in pathologic fractures. This is often initially mistaken for widespread malignancy [4]. However, the lesions are composed of numerous multinucleated giant cells admixed with fibroblasts and associated with interstitial hemorrhage marked by hemosiderin deposition, resulting in a brown appearance (“brown tumors”). The imaging and histology in isolation may not be diagnostic for osteitis fibrosa cystica due to overlapping features with other conditions but in addition to the biochemical and clinical picture, can lead to the correct diagnosis.
When parathyroid carcinoma is a concern, as in this setting, the surgical team should be alerted to this possibility so that the appropriate en bloc surgical resection can be performed (see Chap. 10). Also when parathyroid carcinoma is a concern, FNA is not diagnostic and has the potential for tumor seeding [5].
Management
The subtrochanteric femur fracture required resection and endoprosthetic replacement. The pathology from the operation revealed a brown tumor of hyperparathyroidism (Fig. 2.2). The patient then underwent neck surgery with excision of a 5.3 × 3.5 × 2.2 cm left superior parathyroid adenoma that was adherent to the left lobe of the thyroid but did not show invasion to suggest carcinoma. Postoperatively, hypocalcemia and hypophosphatemia developed, and she was treated with calcium, initially intravenous via central line, and calcitriol.
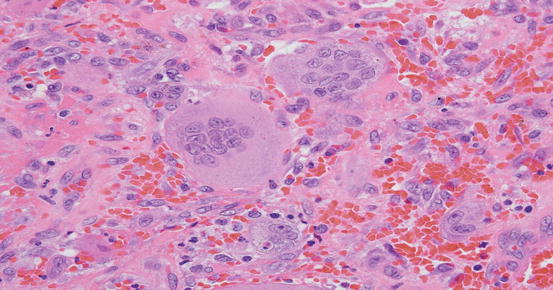
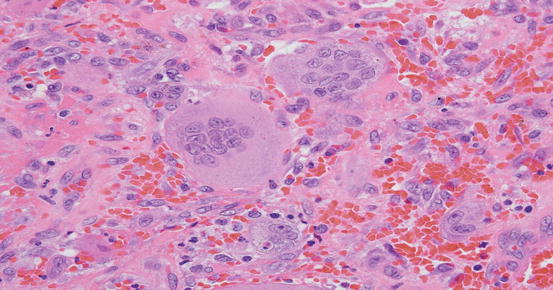
Fig. 2.2
Histology of tumor-resected femur showing the presence of multinucleated giant cells admixed with fibroblasts and associated with interstitial hemorrhage consistent with a brown tumor from hyperparathyroidism
Hypocalcemia following parathyroidectomy is common but usually transient and not symptomatic. Hungry bone syndrome is the term used to describe prolonged, severe, symptomatic hypocalcemia, often with hypophosphatemia, accompanied by normal or elevated PTH levels [6]. This distinguishes it from postoperative hypoparathyroidism in which the PTH is low and the phosphorus is increased. Depending on the severity of hypercalcemia at the time of surgery, the development of hypocalcemia due to hypoparathyroidism may be delayed up to 48 h postoperatively. Postoperative hypoparathyroidism is often also accompanied by significant hypercalciuria, due to the loss of PTH-stimulated renal tubular reabsorption of calcium, and is not seen in hungry bone syndrome. The hypophosphatemia of hungry bone syndrome does not usually require replacement (unless <1.0 mg/dL), and intravenous phosphorus should be avoided due to the further lowering of calcium seen with it. In this case, hypocalcemia developed rapidly following parathyroidectomy, as her calcium was normalized preoperatively. Her coexistent vitamin D deficiency may also have contributed to hungry bone syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree