SJS/TEN (Stevens-Johnson syndrome/toxic epidermal necrolysis)
SJS/TEN-like hypersensitivity reaction or SJS/TEN mimics
DRESS (drug reaction with eosinophilia and systemic symptoms)
AGEP (acute generalized exanthematous pustulosis)
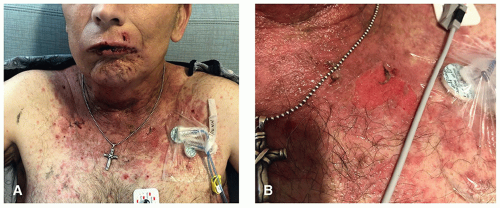 Figure 21.1. PD-L1-induced Stevens-Johnson syndrome-like reaction with mucosal sloughing (A). Epidermal detachment from ECG lead demonstrating positive Nikolsky sign (B). |
the reaction was due to oncologic therapy or a supportive medication. Traditional nononcologic medications most commonly associated with SJS/TEN are as follows:
Antibiotics—most commonly sulfamethoxazole/trimethoprim
Allopurinol
Anticonvulsants
Paraneoplastic Pemphigus (PNP): A paraneoplastic autoimmune bullous disease with skin and mucosal involvement. May be clinically identical to SJS/TEN; however, a skin biopsy for H&E and direct immunofluorescence will help distinguish between the two. Moreover, PNP would be characterized by a chronic course with relapses and a culprit medication is often difficult to identify. Most commonly associated malignancies are non-Hodgkin lymphomas, chronic lymphocytic leukemia, and Castleman disease; however, many diverse malignancies have been reported.
Toxic Medication Accumulation: Seen with cytotoxic chemotherapies when supratherapeutic medication accumulation occurs through lack of excretion due to renal or hepatic insufficiency, genetic enzyme deficiency resulting in decreased metabolism of the medication, or iatrogenic overdose. Skin blistering and mucositis may occur due to direct toxic effects from the medication rather than an immune-mediated process as is seen in true SJS/TEN. Specific examples of these include the following:
□ Methotrexate-induced epidermal necrolysis: Toxic accumulation of methotrexate (MTX) results in diffuse skin sloughing and mucositis. Risk factors are absence of folate supplementation, impaired kidney function, and older age.2
Leukopenia and pancytopenia are rare findings in SJS/TEN and point toward MTX-induced bone marrow suppression
Skin biopsy may help to differentiate the two, however, imperfectly as significant histological overlap exists
First-line therapy includes prompt leucovorin rescue.
□ 5-fluorouracil (5-FU)-toxicity due to dihydropyrimidine dehydrogenase (DPD) deficiency: Prevalent in 3% to 5% of the population. Presents with fevers, severe erythematous rashes, oral mucositis, diarrhea, neurological abnormalities, leucopenia, and thrombocytopenia often within ˜1 week of treatment onset. Management includes 5-FU discontinuation, evaluation of DPD levels via reverse transcription quantitative polymerase chain reaction, supportive care, and potentially hemodialysis.3
Severe Intertriginous Eruptions: Cytotoxic therapy may cause local erosions due to excreted drug in intertriginous areas, which may be due to direct toxic effects or local allergic contact dermatitis. These drug classes may also induce mucositis as a direct toxic effect. The clinical presentation of both skin and mucosal lesions is most helpful in clarifying this diagnosis.
Erythema Multiforme: Presents with true target lesions (three zones of color). The center of these lesions may develop small vesicles or bullae, but extensive skin sloughing
is not seen and overall body surface area is <10%. Mucosal involvement is common. Common triggers include prior mycoplasma infection or herpes simplex virus.
TABLE 21.1 • Reported Oncologic Medication Culprits Associated With SJS/TEN and SJS/TEN Mimics
Traditional chemotherapeutics*
Targeted anticancer therapy
Anticancer immunotherapy
Docetaxel (Plant alkaloid)
Imatinib (BCR-ABL inhibitor)
Pembrolizumab (PD1 inhibitor)**
Etoposide (Plant alkaloid)
Rituximab (Anti-CD20 antibody)
Nivolumab (PD1 inhibitor)**
Paclitaxel (Plant alkaloid)
Vemurafenib (BRAF inhibitor)
Ipilimumab (CTLA4 inhibitor)**
Bleomycin (Antitumor antibiotic)
Afatinib (EGFR inhibitor)
Aldesleukin (Recombinant IL2)
Mithramycin (Antitumor antibiotic)
Cetuximab (EGFR inhibitor)
Denileukin (Rec.IL2 + Diph. Toxin)
Mechlorethamine (Alkylating agent)
Erlotinib (EGFR inhibitor)
Temozolomide (Alkylating agent)
Gefitinib (EGFR inhibitor)
Procarbazine (Alkylating agent)
Panitumumab (EGFR inhibitor)
Immunomodulatory Therapy:
Chlorambucil (Alkylating agent)
Vandetanib (EGFR inhibitor)
Lenalidomide
Treosulfan (Alkylating agent)
Bortezomib (Proteasome inhibitor)
Thalidomide
Pemetrexed (Antimetabolite)
Brentuximab (Anti-CD30 antibody)
Cytarabine (Antimetabolite)
Regorafenib (Antiangiogenic agent)
Fludarabine (Antimetabolite)
Sorafenib (Antiangiogenic agent)
Gemcitabine (Antimetabolite)
Sunitinib (Antiangiogenic agent)
Capecitabine (Antimetabolite)
Cladribine (Antimetabolite)
6-Mercaptopurine (Antimetabolite)
Pemetrexed (Antimetabolite)
Doxorubicin (Anthracycline)
Asparaginase
* Important to distinguish from toxic medication accumulation vs. true SJS/TEN.
** Important to distinguish from lichenoid and autoimmune mucocutaneous reactions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree