Sensory Impairment: Introduction
Because as many as 75% of older adults have significant visual or auditory dysfunction not reported to their physicians, adequate screening for these problems is important. These disorders may limit functional activity and lead to social isolation and depression. Correction of remediable conditions may improve ability to perform daily activities.
Vision
The visual system undergoes many changes with age (Table 13–1). Decreases in visual acuity in old age may be caused by morphological changes in the choroid, pigment epithelium, and retina, or by decreased function of the rods, cones, and other neural elements. Older patients frequently have difficulties turning their eyes upward or sustaining convergence. Intraocular pressure slowly increases with age.
Functional change | Physiological change |
|---|---|
Visual acuity | Morphological change in choroid, pigment epithelium, or retina Decreased function of rods, cones, or other neural elements |
Extraocular motion | Difficulty in gazing upward and maintaining convergence |
Intraocular pressure | Increased pressure |
Refractive power | Increased hyperopia and myopia Presbyopia Increased lens size Nuclear sclerosis (lens) Ciliary muscle atrophy |
Tear secretion | Decreased tearing Decreased lacrimal gland function Decreased goblet cell secretion |
Corneal function | Loss of endothelial integrity Posterior surface pigmentation |
The refractive error may become either more hyperopic or more myopic. In younger persons, hyperopia may be overcome by the accommodative power of the ciliary muscle on the young lens. However, with age, this latent hyperopia becomes manifest because of loss of accommodative reserve.
Other older patients may show an increase in myopia with age, caused by changes within the lens. The crystalline lens increases in size with age as old lens fibers accumulate in the lens nucleus. The nucleus becomes more compact and harder (nuclear sclerosis), increasing the refractive power of the lens and worsening the myopia.
Another definitive refractive change of aging is the development of presbyopia from nuclear sclerosis of the lens and atrophy of the ciliary muscle. As a result, the closest distance at which one can see clearly slowly recedes with age. At approximately age 45, the near point of accommodation is so far that comfortable reading and near work become cumbersome and difficult. Corrective lenses are then needed to enable the patient to move that point closer to the eyes.
Diminished tear secretion in many older patients, especially postmenopausal women, may lead to dryness of the eyes, which can cause irritation and discomfort. This condition may endanger the intactness of the corneal surface. The treatment consists mainly in substitution therapy, with artificial tears instilled at frequent intervals.
The corneal endothelium often undergoes degenerative changes with aging. Because these cells seldom proliferate during adult life, the cell population is decreased. This may leave an irregular surface on the anterior chamber side, where pigments may accumulate. This type of endothelial dystrophy is frequently seen in older patients, and dense pigment accumulation may slightly decrease visual acuity. In some patients, the endothelial dystrophy will spontaneously progress and lead to corneal edema. Such cases require corneal transplants.
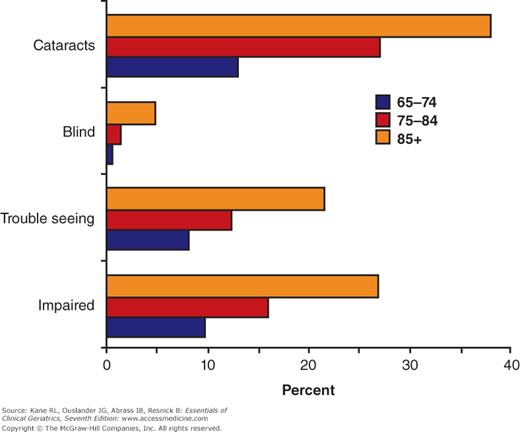
The prevalence of visual problems and blindness increases with age (Fig. 13-1). The most common causes of blindness are cataracts, glaucoma, macular degeneration, and diabetic retinopathy. Screening for these disorders should include testing visual acuity, performing an ophthalmoscopic evaluation, and checking intraocular pressure (Table 13–2).
Opacification of the crystalline lens is a frequent complication of aging. In the Framingham Eye Study, the prevalence of cataracts was associated with age and reached 46% at ages 75 to 85 (Kini et al., 1978). The development of age-related cataract is a painless, progressive, but variable, process. Cataract formation is typically bilateral and often asymmetrical. Patients usually complain of problems with night driving, reading road signs, and difficulty with fine print.
The cause of age-related cataracts is unknown, but the opacifications in the lens are associated with the breakdown of the g-crystalline proteins. Epidemiological data and basic research suggest that ultraviolet light may be a contributing factor in cataract development. The pathological process may occur in either the cortex or the nucleus of the lens. Cortical cataracts have various stages of development. Early in the process, opacities are in the periphery and do not decrease visual acuity. At the mature stage, opacifications are more widespread and involve the pupillary area, leading to a slow decrease in visual acuity. In the mature stage, the entire lens becomes opaque. The nuclear cataract does not have these stages of development, but is a slowly progressing central opacity, which frequently shows a yellowish discoloration, therefore preventing certain colors from reaching the retina.
Cataracts of mild degree may be managed by periodic examination and optimum eyeglasses for an extended period. Ultraviolet lenses may be of benefit. When a cataract progresses to the point where it interferes with activities, cataract surgery is generally indicated. The surgeon may use several methods to remove it, and the decision regarding the best method for each patient should be made by the ophthalmologist.
In intracapsular cataract extractions, the entire cataract and surrounding capsule are removed in a single piece. This removes the entire opacity. In extracapsular cataract extractions, the cataractous lens material and a portion of the capsule are removed. The posterior capsule is left in place to hold an intraocular lens implant.
The intraocular lens is surgically placed inside the iris and is expected to remain permanently in place. This lens corrects the focus of the eyes and permits central and peripheral vision; object size is increased by only 1%. It is appropriate for patients with cataracts in one or both eyes and is particularly useful for patients unable to wear a contact lens. Because the lens cannot change shape to accommodate, the lens can be chosen to provide good near or far vision and glasses prescribed to compensate for the other type of vision. (Table 13–3).
Intraocular lenses |
Correct central and peripheral vision Increase image size by 1% Can be used after surgery on one or both eyes Are useful for older adults unable to wear contact lenses Require bifocal eyeglasses Introduce added surgical and postsurgical complications |
Contact lenses correct the focus of the eye, permit both central and peripheral vision, and increase apparent object size by 6%. However, handling contact lenses is difficult for some individuals, and most lenses must be removed and inserted daily. Extended-wear contact lenses are available, and approximately 50% to 70% of elderly patients are able to wear them after surgery. Contacts are useful in patients who have had cataract surgery in one or both eyes. The lenses correct for distant vision, but eyeglasses are required for reading. Bifocal lenses are available but require some active adjustment.
Visual impairment is a known risk factor for falls and fractures, while patients who have had cataract surgery have a lower risk for hip fracture (Tseng et al., 2012).
The glaucomas are a group of eye disorders characterized by increased intraocular pressure, progressive excavation of the optic nerve head with damage to the nerve fibers, and a specific loss in the visual field. Visual field testing should be performed. Initial changes lead to peripheral vision loss, with loss of central vision as the disease progresses. Most cases of primary glaucoma occur in older patients. In the Framingham Eye Study, prevalence of open-angle glaucoma increased with age to 7.2% at ages 75 to 85, with men having much higher rates than women (Kini et al., 1978).
Angle-closure glaucoma is an acute and relatively infrequent type of glaucoma, characterized by a sudden painful attack of increased intraocular pressure accompanied by a marked loss in vision. The treatment consists of normalizing the intraocular pressure by the application of miotic eye drops or other medication (such as carbonic anhydrase inhibitors or osmotic agents). The definitive treatment, however, is surgical excision of a peripheral piece of iris or, more frequently now, by laser iridectomy, ensuring free flow of aqueous humor. Because the disease is usually bilateral, some physicians propose prophylactic iridectomy on the second eye.
Chronic open-angle glaucoma is the more frequent variety of primary glaucoma. (See Kwon et al., 2009, for a review.) It is the second leading cause of blindness in the United States and the leading cause of blindness among black Americans. The irido-corneal angle is open, but aqueous outflow is diminished. The neuroretinal rim of the optic nerve becomes progressively thinner, leading to optic-nerve cupping. Its cause is the loss of retinal ganglion cell axons. Primary open-angle glaucoma is characterized by an insidious onset, slow progression, and the appearance of typical defects of the visual fields. Early in the disease, intraocular pressure is only moderately elevated, and optic nerve head excavation progresses slowly and sometimes asymmetrically. While central visual acuity may remain normal for a long time, the defects in the peripheral visual field are characteristic and gradually progressive. Initially, there is a paracentral scotoma, which may coalesce. A nasal step of the visual field is another important sign. Finally, the entire field will constrict and eventually involve the visual centers.
The treatment is usually medical, with miotics of various kinds used first. β-Blocking agents may also be used and have the advantage of not changing the diameter of the pupil. However, care should be taken because these agents may be systemically absorbed and interact with other functions mediated by β agonists. In severe cases, combination drops may be used with systemic medications such as carbonic anhydrase inhibitors. Surgery or laser therapy is indicated only if disease progresses on maximal medical therapy.
The macular area of the retina lying at the posterior pole of the globe is the site of highest visual acuity. This area depends entirely on choriocapillaries for nutrition.
Any disturbance in the vessel wall of the choroidal capillaries, in the permeability or thickness of the Bruch membrane, or in the retinal pigment epithelium may interfere with the exchange of nutrients and oxygen from the choroidal blood to the central retina. Such disturbances occur frequently in older patients. Age-related degeneration of the macula is one of the most frequent causes of visual loss in older adults and is the commonest cause of legal blindness (20/200 or worse) (see Chakravarthy, Evans, and Rosenfeld, 2010, for a review). In the Framingham Eye Study, the prevalence was 28% at ages 75 to 85 years, with a higher rate in women than in men (Kini et al., 1978). In addition to older age, risk factors include family history of the disorder, cigarette smoking, low dietary intake or plasma concentrations of antioxidant vitamins and zinc, and white race for “wet” lesions (Fine et al., 2000). Age-related macular degeneration (AMD) is a common disease caused by the interplay of genetic predisposition and exposure to modifiable risk factors. Two susceptibility genes have been identified (CFH and LOC387715). Carrying the susceptibility alleles of either increases the risk between three-and eightfold, whereas having two copies of the susceptibility alleles in both genes increases the risk 50-fold (Schaumberg et al., 2007). The combined effect of these polymorphisms carries an attributable risk of 60% (Haines and Pericak-Vance, 2007). Cigarette smoking and obesity multiply the risks associated with these variants. High lifetime exposure to sunlight is also a risk factor.
Ophthalmoscopic findings vary and do not always parallel loss of vision. In the geographic atrophy form of degeneration, there are areas of depigmentation alternating with zones of hyperpigmentation caused mainly by changes in the retinal pigment epithelium. In another form, the degeneration involves the Bruch membrane, leading to the pigmentation of well-circumscribed, roundish yellow areas. As lesions coalesce and involve the central macula, there is progressive worsening of vision to legal blindness.
In the second type of degeneration, there is an acute exudative pathology as a consequence of neurovascularization. Here there is an elevated focus in the macular area, which at first contains serous fluid but later contains blood derived from blood vessels sprouting from the choroid to the subretinal space. The blood may become organized and form a plaque. Geographic atrophy AMD may produce a slow deterioration of central vision. Neurovascular AMD can cause a rapid distortion and loss of central vision.
In all these cases, central visual acuity will be markedly affected. Reading, driving, and recognizing faces become difficult. The atrophic type has no proven treatment or prevention. Verteporfin photodynamic (PTD) therapy has been shown to be beneficial in the treatment of advanced wet-type AMD (reviewed in Bourla and Young, 2006). PTD therapy combines the intravenous infusion of the light-sensitive dye verteporfin with low-intensity laser targeted to the neovascular tissue, causing occlusion of the abnormal choroidal vessels. However, recent therapy has been directed to vascular endothelial growth factor (VEGF) antagonism (reviewed in Chakravarthy, Evans, and Rosenfeld, 2010). VEGF may play a critical role in the pathogenesis of neovascularization. Several VEGF antagonists, both systemic and intraocular injections, are available, but ranibizumab given monthly by intravitreal injection is the first drug demonstrated to not only slow progression but to improve vision in patients with neovascular AMD. Total blindness does not occur, as patients retain peripheral vision and therefore are able to perform activities that do not necessitate acute central vision. In the United Kingdom guidance by the National Institute for Health and Clinical Excellence has resulted in ranibizumab being adopted as the treatment of choice. However, the high cost of ranibizumab, along with the much cheaper and positive clinical experience with bevacizumab (Martin et al., 2011), has resulted in the majority of patients in the United States and other countries being treated with the latter drug. Visual rehabilitation is an important part of therapy for AMD. Patients may benefit from reading glasses or magnification devices. Clinical depression may occur as a consequence of reductions in quality of life and should be treated.
In the geriatric population, a significant amount of visual loss is attributed to diabetic retinopathy. The Framingham Eye Study showed an age-associated increase in prevalence up to 7% at ages 75 to 85 years (Kini et al., 1978). In adult-onset diabetes with background changes, the visual loss is usually related to vascular changes in and around the macula leading to central visual loss. Leakage of serous fluid from vessels surrounding the macula leads to macular edema and deterioration of visual acuity. This may respond to laser photocoagulation.
Hemorrhages within the macula may lead to more permanent visual loss. A loss of retinal capillaries may lead to macular ischemia and poor prognosis of visual recovery.
Intensive blood glucose control and tight blood pressure control reduce the risk of microvascular disease, including retinopathy in type 2 diabetes (see Chapter 12). Panretinal and focal retinal laser photocoagulation reduces the risk of visual loss in patients with severe diabetic retinopathy and macular edema, respectively (reviewed in Mohamed, Gillies, and Wong, 2007). There is currently insufficient evidence for routine use of other treatments, such as VEGF antagonists.
Table 13–4 summarizes the general patterns of signs and symptoms associated with common visual problems of older adults. In addition to the specific treatment discussed earlier, some simple techniques, such as use of a magnifying device, large-print reading material, lighting intensifiers, and reduction of glare, can help maximize visual function (Table 13–5).
Signs and symptoms | Cataract | Open-angle glaucoma | Angle-closure glaucoma | Macular degeneration | Temporal arteritis | Diabetic Retinopathy |
|---|---|---|---|---|---|---|
Pain | x | x | ||||
Red eye | x | |||||
Fixed pupil | x | |||||
Retinal vessel changes | x | x | ||||
Retinal exudates | x | x | ||||
Optic disk changes | x | x |