FIGURE 4.1
4.2.1 HyperTG HyperapoB: Increased VLDL and LDL Lipoprotein Particles
Pathophysiology of Increased VLDL and LDL Particle Number
The most frequently observed atherogenic dyslipoproteinemia in overweight or obese patients with DM2 or metabolic syndrome is the HyperTG HyperapoB phenotype, which is defined as an increased number of VLDL and LDL particles. HDL-C is often low as well (Figure 4.2 ). In Figure 4.3 a general overview of the different mechanisms contributing to dyslipidemia are indicated. Increased flux of free fatty acids from adipocytes to hepatocytes results in increased synthesis and secretion of triglycerides and cholesterol ester with the result that increased numbers of VLDL particles are secreted resulting in increased formation of LDL particles — thus the increased apoB. Hyperinsulinemia, due to insulin resistance in obesity, promotes fatty acid and cholesterol synthesis in the liver, which adds to the tendency to increased VLDL production and secretion of VLDL particles. VLDL catabolism may be impaired due to decreased LPL activity, which can be associated with insulin resistance. Increased apoCIII may contribute both to increased synthesis and decreased clearance of triglyceride (see Figure 1.15 ). ApoCIII may also increase the conversion of VLDL particles to LDL particles.7 Increased CETP activity also contributes to the atherogenic lipoprotein phenotype characterized by high apoB, low HDL-C, small, cholesterol depleted LDL, high triglycerides with relatively cholesterol-rich VLDL particles (see Figure 1.12 ).
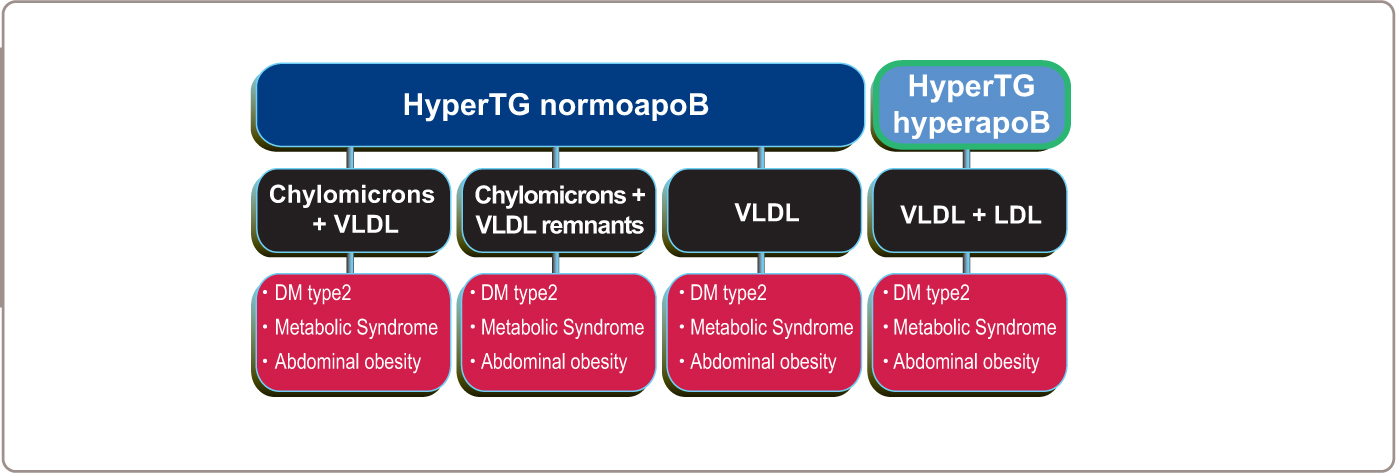
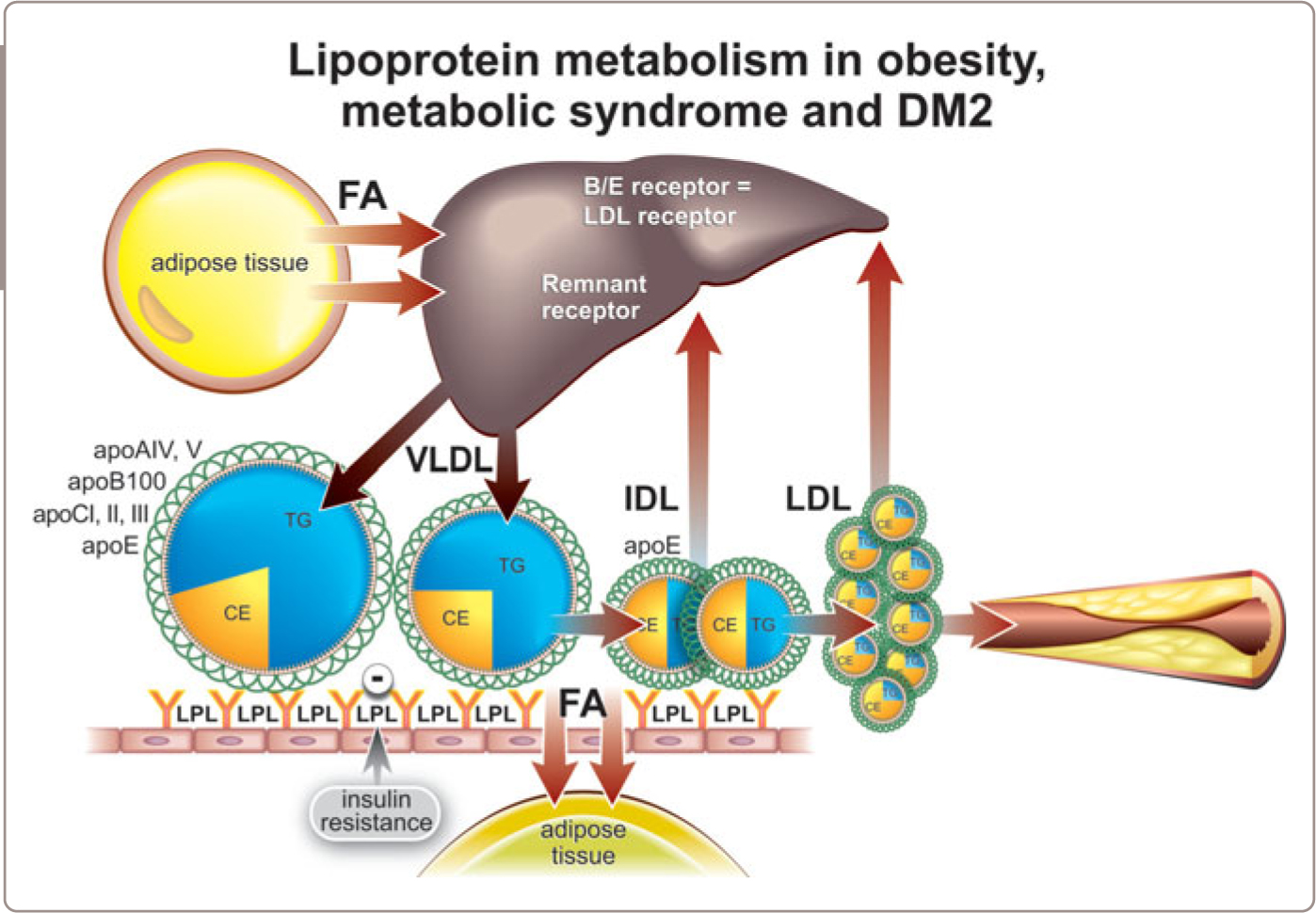
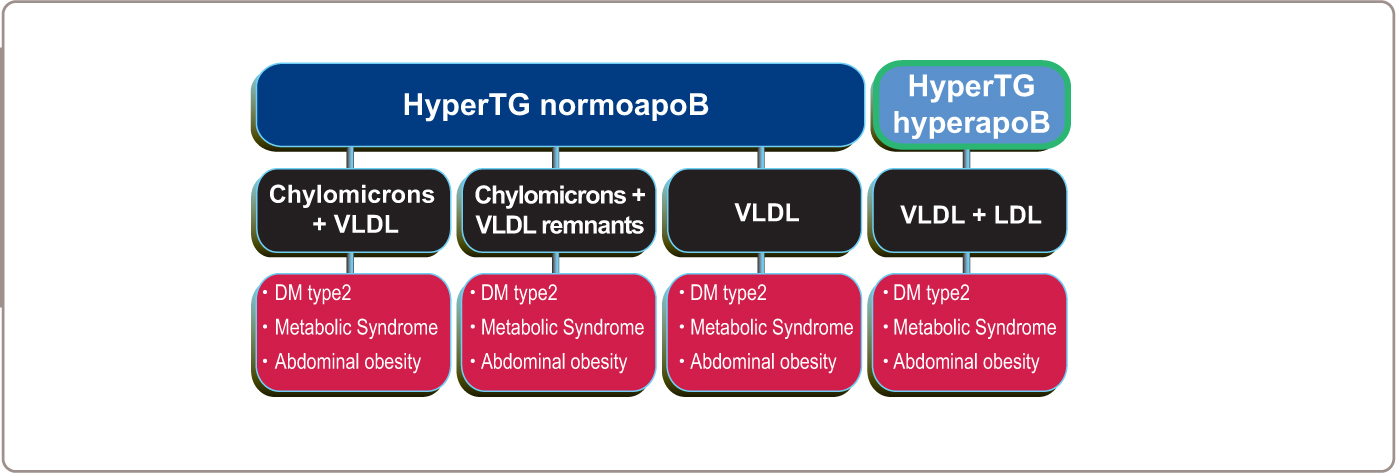
FIGURE 4.2
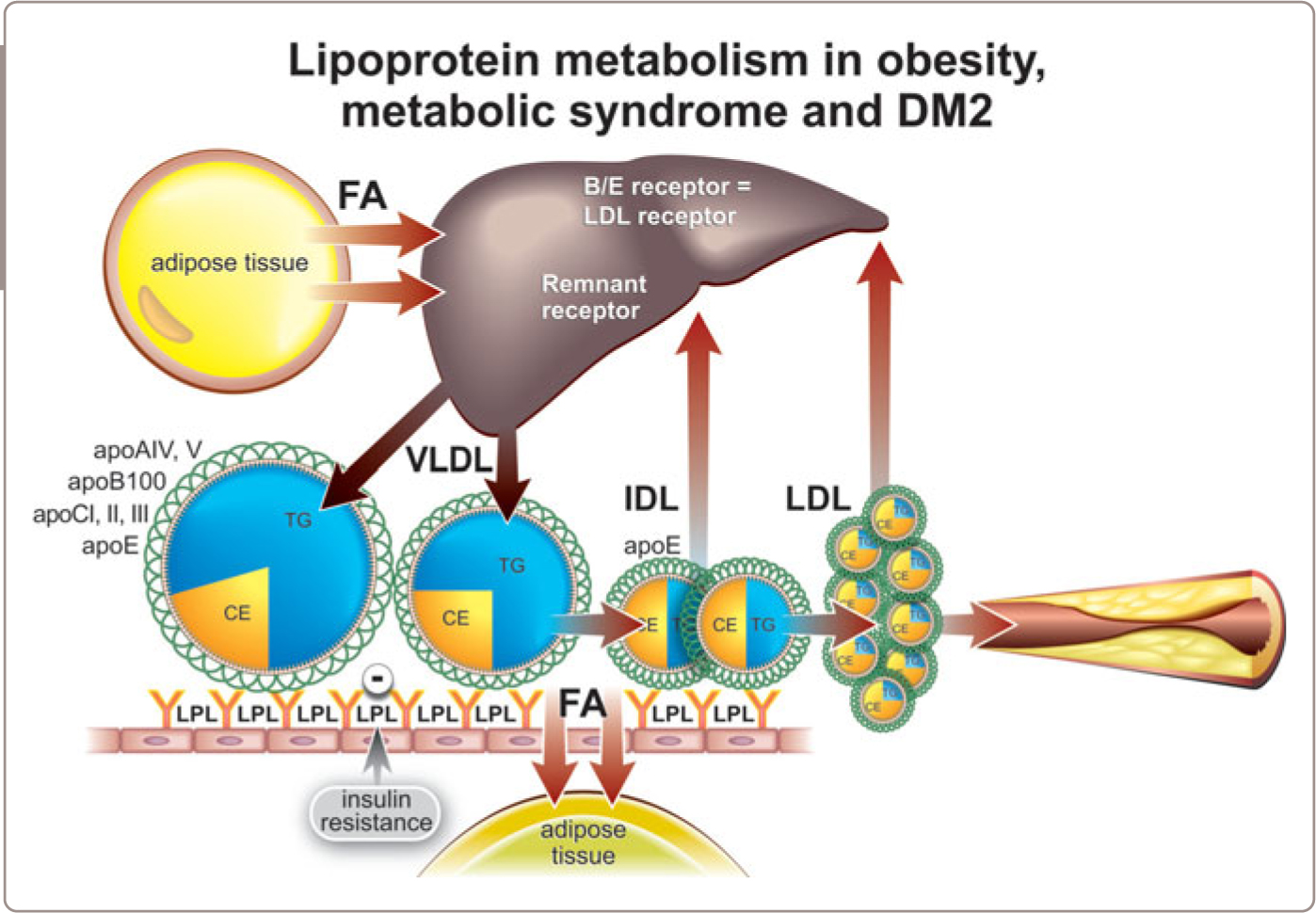
FIGURE 4.3
Clinical Diagnosis
No diagnostic stigmata of high VLDL and LDL are present on physical examination. Treatment Individuals with obesity, metabolic syndrome, DM2 and increased VLDL and LDL (HyperTG HyperapoB) should be treated aggressively due to their significantly increased risk of premature CVD (Table 4.1 ). Weight loss is a difficult but necessary objective and weight loss and aerobic exercise can have beneficial effects on the lipid profile. However, the great majority will require lipid-lowering drug therapy to reduce atherogenic apoB lipoprotein levels to the recommended range (< 0.75 g/l for high-risk and < 0.65 g/l for very high-risk patients) necessary to reduce the high risk of CVD. Note apoB, not triglycerides, are the primary target of therapy. Statins are effective in this condition, but many patients will need a second drug such as a cholesterol absorption inhibitor (ezetimibe) for optimal control of apoB levels. Such agents are also necessary for statin-intolerant patients. The IMPROVE-IT study demonstrated additional clinical benefit with ezetimibe plus statin and this result supports its use in the appropriate clinical settings. Pharmacological therapy with fibrates added to statins has been suggested to reduce triglycerides and increase HDL-C in very high-risk patients. However, clinical trial results have not supported this combination, albeit the subjects were not selected for this phenotype.
Table 4.1
Steps in treatment | HyperTG HyperapoB (increased VLDL and LDL particles) | ||
|---|---|---|---|
General measures including lifestyle intervention and check for / treat other secondary or primary causes | Weight loss, exercise, stop smoking, stop alcohol, decrease saturated fat and simple carbohydrates intake | ||
Risk of CVD | ++[+] | ||
Treatment to prevent CVD | 1. statins 2. ezetimibe | ||
Targets to prevent CVD | apoB < 0.75 g/l in moderate and high risk apoB < 0.65 g/l in very high risk | ||
Risk of pancreatitis | – |
4.2.2 HyperTG NormoapoB: Increased VLDL Lipoprotein Particles
Pathophysiology of High VLDL
If triglyceride synthesis and secretion are increased but VLDL apoB secretion is normal, the number of LDL particles will be normal and therefore total plasma apoB will be ‘normal’ (that is < 1.20 g/l) in the face of an elevated plasma triglyceride (≥ 1.5 mmol/l). If so, the VLDL particles are likely to be triglyceride enriched. Alternatively, this phenotype may be due to a decreased clearance rate of VLDL particles coupled to a normal production rate, as could occur with primary or secondary impairment of LPL activity (Chapter 3 , section 3.1.4 ).
Clinical Diagnosis
No diagnostic stigmata attributable to high VLDL are present on physical examination.
Treatment
Because the number of atherogenic particles is not markedly increased (apoB < 1.20 g/l), the atherogenic risk of this dyslipoproteinemia is not markedly increased (Table 4.2 ). But there is nothing magic in the dividing line of 1.20 g/l. Cardiovascular risk rises exponentially as the level of apoB increases and therefore the higher the apoB, the higher the risk. Just as importantly, it is the apoB that is the issue, not the triglycerides since there is no evidence that lowering triglycerides improves clinical outcome. In patients with other high-risk abnormalities, such as DM2, pharmacological therapy would be indicated to lower apoB. If so, statins should be the primary therapy to reduce apoB to the appropriate target level with ezetimibe added if necessary to reach the appropriate apoB target level (apoB < 0.75 g/l in high-risk and < 0.65 g/l in very highrisk patients).
Table 4.2
Steps in treatment | HyperTG NormoapoB [increased VLDL particles] |
|---|---|
General measures including lifestyle intervention and check for / treat other secondary or primary causes | Weight loss, exercise, stop smoking, stop alcohol, decrease saturated fat and simple carbohydrates intake |
Risk of CVD | +/- depending on associated high-risk conditions ie DM2 etc |
Treatment to prevent CVD | 1. statins 2. ezetimibe |
Targets to prevent CVD | apoB < 0.75 g/l in moderate and high risk apoB < 0.65 g/l in very high risk |
Risk of pancreatitis | – |
Ezetimibe can be used in patients who do not tolerate statins. As increased triglyceride levels are the main lipid presentation of this phenotype, clinicians might consider fibrates. However, while fibrates lower triglyceride levels, they only modestly lower the number of atherogenic apoB particles and there is insufficient randomized clinical trial evidence to justify their use in this phenotype.
4.2.3 HyperTG NormoapoB: Increased Chylomicron and VLDL Lipoprotein Particles
Pathophysiology of Excess Chylomicron and VLDL
In some patients with obesity, especially those with an associated genetic defect in lipid metabolism (see Chapter 3 , section 3.1.2 ), serum triglycerides can be extremely elevated. Obesity, particularly abdominal obesity, can lead to increased production of VLDL due to increased flux of fatty acids to the liver. If partial LPL deficiency were also present, the combination might result in the phenotype of an increased number of triglyceride-rich VLDL and chylomicron particles.
Clinical Consequences
Patients with severe hypertriglyceridemia due to chylomicrons and VLDL particles may present with eruptive xanthomata (Figure 3.6 ) and their plasma may appear milky (Figure 3.9 ). If chylomicron and VLDL particle numbers are increased sufficiently, pancreatitis may occur. In such patients, plasma triglycerides will generally be > 10 mmol/l. Plasma apoB is only occasionally elevated above the 75th percentile (i.e. > 1.20 g/l); in these patients, lowering of apoB is indicated. For those with intermediate apoB levels (0.75-1.20 g/l), the decision to institute apoB-lowering therapy should be based on the associated clinical characteristics of the patient.
Treatment
In those with severe hypertriglyceridemia who are at risk of pancreatitis, dietary total fat intake should be reduced, acutely and profoundly (Table 4.3 ). Other secondary or primary causes should be identified and, if present, treated. Treatment with fibrates may be helpful in these patients as partial LPL activity is likely present. Nicotinic acid or long-chain n-3 polyunsaturated fatty acids (PUFAs) remain an option but the clinical trial evidence is lacking. Whether apoB-lowering therapy with statins is indicated depends on the level of apoB and the clinical circumstances. Thus, patients with increased cardiovascular risk because of the presence of DM2 or a history of CVD will require apoB-lowering therapy to target apoB levels < 0.65 g/l.
Table 4.3
Steps in treatment | HyperTG NormoapoB (increased chylomicron and VLDL particles) |
|---|---|
General measures including lifestyle intervention and check for / treat other secondary or primary causes | – fasting for > 24 hours – IV fluids if necessary – insulin drip – dietary fat restriction 15 g/d – followed by low fat diet – no alcohol, weight loss, treat diabetes |
Risk of CVD | Depends on apoB and associated high risk conditions |
Treatment to prevent CVD | statins |
Targets to prevent CVD | apoB < 0.75 g/l in moderate and high risk apoB < 0.65 g/l in very high risk |
Risk of pancreatitis | + + |
Treatment to prevent pancreatitis | 1. fibrates 2. long chain n-3 PUFA 3. nicotinic acid |
Target to prevent pancreatitis | TG < 5 mmol/l |
4.2.4 HyperTG NormoapoB: Increased Chylomicron and VLDL Remnant Lipoprotein particles
Pathophysiology of Chylomicron and VLDL Remnants — Remnant Lipoprotein Disorder
Familial dysbetalipoproteinemia (FDBL) or remnant lipoprotein disorder may become evident in patients with obesity, metabolic syndrome or DM2. FDBL is characterized by markedly increased numbers of chylomicron and VLDL remnants (Chapter 3 , section 3.1.3 ). However, homozygosity of apoE2/E2 alleles is not sufficient to produce the full clinical syndrome. Only 1 in 50 to 1 in 100 of apoE2 homozygotes have the clinical profile of FDBL. There is also evidence that most patients with FDBL are not apoE2/E2. Given that FDBL is only present in a small minority of apoE2 homozygotes, some additional provoking factor must be present to produce the full clinical syndrome. This second abnormality is generally one that increases fatty acid flux to the liver with the result that VLDL apoB production increases. The most common precipitating factors are a high-fat diet, DM2, obesity and the metabolic syndrome. Furthermore, hypothyroidism, renal disease, estrogen deficiency, alcohol use, or certain drugs may be involved.
Clinical Diagnosis
Chylomicron and VLDL remnants are extremely atherogenic lipoprotein particles and peripheral vascular disease is a major clinical feature in these patients as well as CAD. Think of remnant lipoprotein disorder when tubero-eruptive and palmar xanthomas (Figure 3.15 and 3.17 ), premature CAD and peripheral vascular disease are found in obese patients with or without metabolic syndrome or DM2 (FDBL, Chapter 3 , section 3.1.3 ).
4.2.5 Treatment
Since remnants are associated with markedly increased risk of premature CVD, this atherogenic apoB phenotype should be treated aggressively (Table 4.4 ). The first step is to treat the conditions that precipitate the expression of the phenotype, such as obesity, DM2, metabolic syndrome, significant alcohol intake and hypothyroidism. Weight reduction is recommended. Alcohol intake should be curtailed and estrogen treatment stopped. Pharmacological treatment is aimed at decreasing the number of atherogenic remnant particles. In this instance, risk would be severely underestimated if total plasma apoB were relied on. Treatment should aim at normal levels of cholesterol (< 5 mmol/l) and triglyceride (< 2 mmol/l) and apoB levels < 0.65 g/l. Patients with remnant lipoprotein disorder may respond well to fibrates as well as statins or even nicotinic acid. Occasionally, combination drug therapy is required.
Table 4.4
Steps in treatment | HyperTG NormoapoB (increased chylomicron and VLDL remnant particles) |
|---|---|
General measures including lifestyle intervention and check for / treat other secondary or primary causes | Stop smoking, exercise, diet, stop alcohol, check medication ie stop estrogens, check for hypothyroidism, treat DM etc. |
Risk of CVD | + + + |
Treatment to prevent CVD | 1. statins
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|