Patients with relapsed or refractory urothelial carcinoma (UC) face a poor prognosis and a dearth of available treatment options that improve their survival. End-organ function and performance status play a vital role in the choice of second-line therapies. Evidence supporting the use of cytotoxic chemotherapy, as single agents or in combination, arises from small phase 2 studies with modest responses. With the evolution of genomic testing in UC, several pathways amenable to available targeted therapies have emerged. Encouraging patient participation in clinical trials is critical to improve patient outcomes and to advance the current modest treatment armamentarium.
Key points
- •
There is no standard of care treatment that improves patient survival.
- •
Taxanes in the US and Vinflunine in Europe are the most commonly used agents.
- •
Participation in clinical trials is critical.
Introduction
Platinum-based chemotherapy regimens have shown significant clinical activity against urothelial carcinomas (UC) and are generally used in the first-line setting. These regimens include combinations such as gemcitabine and cisplatin (GC) and methotrexate, vinblastine adriamycin, cisplatin (MVAC). Although these regimens have initial high response rates (RRs), ranging from 40% to 70%, they are generally not curative, with median progression-free survival (PFS) of approximately 8 months and a 5-year overall survival (OS) of 15%. Most of these patients relapse and require additional therapy, but often, in the setting of decreased performance status and impaired renal function, precluding further administration of cisplatin.
Once patients progress or relapse after initial platinum-based chemotherapy, there is no standard of care treatment in the United States, despite scores of trials attempting to identify agents that improve patient survival. Further complicating matters, these patients tend to be older (median age, 70s), with multiple comorbidities. Selection of second-line or salvage treatment requires careful consideration of their prognosis, performance status, and organ function.
Introduction
Platinum-based chemotherapy regimens have shown significant clinical activity against urothelial carcinomas (UC) and are generally used in the first-line setting. These regimens include combinations such as gemcitabine and cisplatin (GC) and methotrexate, vinblastine adriamycin, cisplatin (MVAC). Although these regimens have initial high response rates (RRs), ranging from 40% to 70%, they are generally not curative, with median progression-free survival (PFS) of approximately 8 months and a 5-year overall survival (OS) of 15%. Most of these patients relapse and require additional therapy, but often, in the setting of decreased performance status and impaired renal function, precluding further administration of cisplatin.
Once patients progress or relapse after initial platinum-based chemotherapy, there is no standard of care treatment in the United States, despite scores of trials attempting to identify agents that improve patient survival. Further complicating matters, these patients tend to be older (median age, 70s), with multiple comorbidities. Selection of second-line or salvage treatment requires careful consideration of their prognosis, performance status, and organ function.
Clinical prognostic factors
Various clinical prognostic factors have been identified in patients with advanced UC. In a retrospective analysis of patients treated with first-line MVAC, Karnofsky Performance Score less than 80% and presence of visceral (lung, liver, or bone) were found to be 2 independent risk factors in predicting survival. When classified by the number of risk factors, 3 groups clearly emerged, with differential survival estimates. Patients with zero, 1, or 2 risk factors were found to have a median OS of 33, 13.4, and 9.3 months, respectively.
In the platinum-refractory second-line setting, performance status and liver metastasis continue to portend worse survival. In addition to these factors, Bellmunt and colleagues identified anemia, defined as a hemoglobin level less than 10 g/dL, as an additional prognostic factor in patients with platinum-refractory UC who were treated with vinflunine. Based on the presence of zero, 1, 2, or 3 prognostic factors; the median OS was 14.2, 7.3, 3.8, and 1.7 months ( P <.001), respectively. In a retrospective review of 7 prospective second-line phase 2 trials, shorter time from previous cisplatin therapy to start of subsequent therapy also portended worse survival. In the randomized phase 3 trial comparing vinflunine in combination with best supportive care (BSC) with BSC in patients relapsing after first-line platinum-based chemotherapy, patients who had received previous cisplatin had overall more favorable prognostic criteria (better performance status and absence of visceral metastasis or anemia) and improved OS.
Biology of advanced urothelial carcinoma
Until recently, the biology of progression in UC after response to previous therapy was poorly understood. Accumulating molecular data have now provided an improved understanding of the underlying tumor biology, and multiple candidate genes have been implicated in the pathogenesis and resistance mechanisms of UC. In advanced UC, alterations in various signaling pathways have been observed, involving angiogenesis (VEGFR [vascular endothelial growth factor receptor], FGFR [fibroblast growth factor receptor], angiopoietin receptor 1 and 2), survival (PI3K/AKT/mTOR [phosphatidylinositol 3-kinase/protein kinase B/mammalian target of rapamycin] pathway, phosphatase and tensin homolog [PTEN], tumor protein p53), and proliferation (MAPK/ERK [mitogen activated protein kinase/extracellular signal-regulated kinases], EGFR [epithelial growth factor receptor], HER2 [human epidermal growth factor receptor 2], JAK-STAT [Janus kinase and signal transducer and activator of transcription]), have been observed, and are frequently associated with poor outcomes.
Recently, a comprehensive profiling of muscle-invasive UCs by The Cancer Genome Atlas (TCGA) project showed 29 recurrently mutated genes, and several potential therapeutic targets in UC, including alterations in PIK3CA, HER2, FGFR3, TSC1 and HER3, as well as mutations in chromatin-regulating genes MLL, MLL2, MLL3, CREBBP, CHD7, SRCAP, ARID1A, KDM6A (UTX), and EP300. Several of the genomic alterations identified in this study, particularly those involving the PI(3) K/AKT/mTOR, , MAPK, HER2, HER3, FGFR3 and CCND1 (cyclin D1) are amenable in principle to therapeutic targeting.
Encouraging preclinical and clinical data have recently emerged in tumor immunology with therapies focused on enhancing T-cell responses against cancer. PD-L1 (programmed death ligand 1) is an extracellular protein that downregulates immune responses primarily in peripheral tissues by binding to its receptor, PD-1 (pro- grammed death 1). The interaction of PD-L1 with PD-1 inhibits T-cell proliferation, cytokine production, and cytolytic activity, leading to the functional inactivation or exhaustion of T cells.
Overexpression of PD-L1 on tumor cells is believed to impede antitumor immunity by inactivating the host cytotoxic T lymphocytes, resulting in immune evasion. PD-L1 expression is prevalent in many human tumors, and increased PD-L1 expression on tumor cells is associated with a poor prognosis in patients with UC. Therefore, interruption of the PD-L1/PD-1 pathway represents an attractive strategy to reinvigorate tumor-specific T-cell immunity.
Identification of these molecular drivers and escape mechanisms has paved the way for rational investigation and potential development of novel targeted therapeutics in bladder cancer. However, genomic testing of tumors still remains in its nascent stages and requires standardization, replication, and implementation in clinical trials to become standard of care for management of advanced UC.
Approach to patients
In the absence of definitive guidelines, treatment of patients requiring second-line or salvage chemotherapy has distinct challenges, and multiple host-related, disease-related, and therapy-related factors must be considered in formulating a treatment plan. Consideration of a patient’s prognosis forms the backbone of decision making in the salvage setting, in which options include available chemotherapies, enrollment in clinical trials, and BSC. Multiple clinical trials have implicated the patient’s performance status as a strong determinant of their OS. Age and end-organ function also influence the choice of second-line chemotherapy, along with patient eligibility for clinical trials.
Adequate cardiac and renal function, neurologic status, and hearing ability are important components when determining suitability for platinum-based regimens. Carboplatin-based combinations are feasible in patients unsuitable for cisplatin, but small randomized trials have suggested that they are suboptimal compared with cisplatin-based regimens. Previous cisplatin or taxane use can induce significant neuropathy, which may limit the use of these agents in the second-line setting. Retreatment with a previous regimen is a viable option, especially if it is offered after long duration of disease remission. Because platinum-based regimens are often applied in the first-line setting, it is important to define whether the patients are platinum sensitive or refractory. Although not uniformly defined for UC, a relapse-free interval greater or equal to 6 months after the last dose of platinum treatment, a rule generally applied in ovarian cancer, could be used to define platinum sensitivity in UC.
Given the absence of a second-line agent with meaningful improvement in survival, clinical trials should be considered in every patient who is amenable. With the advent of molecular testing and targeted therapies, clinical trials offer a unique opportunity for patient care and also enrich our knowledge of UC pathogenesis.
Results of second-line chemotherapy in advanced urothelial cancer
There is no standard second-line chemotherapy in the United States that is recommended for advanced UC. The evidence for the use of chemotherapy in the second-line setting comes from mostly small phase 2 trials evaluating single agents and combination regimens and 2 phase 3 trials.
Single agents
Several chemotherapeutics have been evaluated in the second-line setting, with modest responses between 8% and 30% ( Table 1 ).
| Drug | Type of Study | Number of Patients | RR (%) | Time to Progression (mo) | Overall Survival (mo) |
|---|---|---|---|---|---|
| Paclitaxel | Phase 2 | 31 | 10 | 2.2 | 7.2 |
| Nanoparticle albumin-bound paclitaxel | Phase 2 | 47 | 27.7 | 6 | 10.8 |
| Pemetrexed | Phase 2 | 13 | 8 | — | — |
| Pemetrexed | Phase 2 | 47 | 27.7 | 2.9 | 9.6 |
| Docetaxel | Phase 2 | 30 | 13.3 | — | 9 |
| Gemcitabine | Phase 2 | 28 | 11 | 4.9 | 8.7 |
| Gemcitabine | Phase 2 | 35 | 22.5 | — | 5 |
| Vinflunine | Phase 2 | 51 | 18 | 3 | 6.6 |
| Vinflunine | Phase 2 | 151 | 15 | 2.8 | 8.2 |
| Vinflunine | Phase 3 | 370 | 8.6 | 3 | — |
| Oxaliplatin | Phase 2 | 18 | 6 | 1.5 | 7 |
| Irinotecan | Phase 2 | 40 | 5 | 2.1 | 5.4 |
| Ixabepilone | Phase 2 | 42 | 11.9 | 2.7 | 8 |
| Bortezomib | Phase 2 | 25 | 0 | 1.4 | 5.7 |
| Ifosfamide | Phase 2 | 56 | 20 | 2.4 | 5.5 |
| Lapatinib | Phase 2 | 34 | 3 | 2 | 4.5 |
| Topotecan | Phase 2 | 44 | 9.1 | 1.5 | 6.3 |
Gemcitabine as a single agent, in varying doses, has shown good RRs, with a low toxicity profile in the second-line setting. In a phase 2 study of 30 patients who had received previous cisplatin-based chemotherapy, gemcitabine 1250 mg/m 2 administered on days 1 and 8 of a 21-day schedule for a maximum of 6 cycles was able to achieve an objective RR of 11%, a mean time to progression (TTP) of 4.9 months, and disease-specific survival of 8.7 months. Previous nonresponders to cisplatin had a significantly lower frequency of response to gemcitabine. Another phase 2 trial with a similar cohort of patients who received gemcitabine 1200 mg/m 2 on day 1, 8, and 15 of a 28-day cycle showed a promising overall response of 22.5%, with a median survival of 5 months.
Taxanes are also frequently implemented after previous use of cisplatin-based chemotherapy. In this setting, docetaxel can elicit an RR of 13.3% and a median survival of 9 months. Paclitaxel monotherapy has been evaluated in several phase 2 trials, with paltry RRs of 5% to 10%. In a phase 2 study evaluating weekly paclitaxel dosing, an RR of 10% with a PFS of 2.2 months and median survival of 7.2 months were noted. The nanoparticle albumin-bound paclitaxel was studied in a phase 2 trial involving 48 patients who had received previous cisplatin-based therapy. The agent elicited an encouraging overall RR of 27·7%, median PFS of 6 months, and a median OS of 10.8 months.
Vinflunine is a microtubule inhibitor that has been evaluated in phase 2 and 3 studies in patients with platinum-refractory advanced UC. In phase 2 studies, vinflunine produced an objective RR of 15% to 18%, a median PFS around 3 months, and a median OS of 6 to 9 months. The promising survival results prompted a phase 3 trial comparing vinflunine plus BSC with BSC alone in 370 patients progressing after first-line platinum-based chemotherapy. Although the median 2-month survival advantage (6.9 months for vinflunine + BSC vs 4.6 months for BSC) was not significant in the intent to treat population (hazard ratio [HR] = 0.88; 95% confidence interval [CI], 0.69–1.12) ( P = .287), in the eligible population (n = 357), the median OS was statistically significantly longer for vinflunine + BSC than BSC (6.9 vs 4.3 months, respectively, P = .04). The overall RR, disease control, and PFS all statistically favored the vinflunine plus BSC group (overall RR [ORR]: 8.6% vs 0%, respectively; P = .006; disease control rate: 41.1% vs 24.8%, respectively; P = .002; median PFS: 3.0 vs 1.5 months, respectively; P = .001; HR = 0.68; 95% CI, 0.54–0.86). Based on this study, vinflunine is approved in Europe as a second-line treatment option for patients with advanced UC who have failed a previous platinum-containing regimen.
Pemetrexed has also shown promise as a well-tolerated, single agent with an RR of 27.7%, PFS of 2.9 months, and a median survival of 9.6 months. Ifosfamide can induce considerable RRs, but at the expense of significant toxicity (RR, 20%; PFS, 2.4 months; OS, 5.5 months). Other agents with modest activity in the second-line setting include ixabepilone and oxaliplatin (see Table 1 ).
Combination regimens
Multiple second-line combination regimens have been evaluated in bladder cancer and frequently include platinums, taxanes, and gemcitabine as backbone agents ( Table 2 ). Although combination regimens have generally shown better RRs, they have not shown improved survival and are frequently associated with higher toxicity.
| Agents | Chemotherapy and Dosing | Study Type | N | RR (%) | OS (mo) |
|---|---|---|---|---|---|
| Gemcitabine/Paclitaxel | |||||
| Meluch et al, 2001 | Gemcitabine 1000 mg/m 2 (D 1, 8, 15) Paclitaxel 200 mg/m 2 (D 1) Every 3 wk | Phase 2 | 54 | 54 | 14.4 |
| Sternberg et al, 2001 | Gemcitabine 2500–3000 mg/m 2 Paclitaxel 150 mg/m 2 Every 2 wk | Phase 2 | 41 | 60 | 14.4 |
| Fechner et al, 2006 | Gemcitabine 1000 mg/m 2 (D 1, 8) Paclitaxel 175 mg/m 2 (D 1) Every 3 wk or Gemcitabine 1250 mg/m 2 (D 1) Paclitaxel 120 mg/m 2 (D 2) Every 2 wk | Randomized Phase 2 | 30 | 44 | — |
| Takahashi et al, 2006 | Gemcitabine 2500 mg/m 2 Paclitaxel 150 mg/m 2 Every 2 wk | Phase 2 | 23 | 30 | 12.1 |
| Kanai et al, 2008 | Gemcitabine 2500 mg/m 2 Paclitaxel 150 mg/m 2 Every 2 wk | Phase 2 | 20 | 30 | 11.5 |
| Suyama et al, 2009 | Gemcitabine 1000 mg/m 2 (D 1, 8, 15) Paclitaxel 180 mg/m 2 Every 4 wk | Phase 2 | 30 | 33.3 | 11.3 |
| 5-Fluorouracil/α-Interferon/Cisplatin | — | — | — | — | — |
| Logothetis et al, 1992 | — | Phase 2 | 28 | 61 | — |
| De Mulder et al, 2000 | — | Phase 2 | 40 | 12.5 | — |
| Paclitaxel/methotrexate/cisplatin | Paclitaxel 200 mg/m 2 , methotrexate 30 mg/m 2 , cisplatin 70 mg/m 2 Every 3 wk | Phase 2 | 25 | 40 | — |
| Paclitaxel/ifosfamide | Ifosfamide 1.0 gm/m 2 D 1–4 Paclitaxel 135 mg/m 2 (24-h infusion, D 4) Every 3 wk | Phase 2 | 26 | 15 | 8 |
| Docetaxel/ifosfamide | Docetaxel 60 mg/m 2 Ifosfamide 2.5 g/m 2 (24-h infusion) Every 3 wk | Phase 2 | 20 | 25 | 4 |
| Methotrexate/paclitaxel | Methotrexate 30 mg/m 2 and paclitaxel 175 mg/m 2 Every 3 wk | Phase 2 | 19 | 32 | 5 |
| Cisplatin/gemcitabine/ifosfamide | Cisplatin 30 mg/m 2 , gemcitabine 800 mg/m 2 , ifosfamide 1 g/m 2 (D 1, 8, 15) Every 4 wk | Phase 2 | 49 | 41 | 9.5 |
| Docetaxel/gemcitabine/carboplatin | Docetaxel 50 mg/m 2 (D 1) Carboplatin AUC = 5 (D 1) Gemcitabine 800 mg/m 2 (D 1, 8) Every 21 d or Docetaxel 50 mg/m 2 (D 1) Carboplatin AUC = 5 (D 1) Gemcitabine 800 mg/m 2 (D 2, 8, or 15) Every 21 d | Phase 1/2 | 20 | 45 | — |
| Carboplatin/paclitaxel | Carboplatin AUC 5 Paclitaxel 200 mg/m 2 Every 3 wk | Phase 2 | 44 | 16 | 6 |
| Gemcitabine/Ifosfamide | — | — | — | — | — |
| Pectasides et al, 2001 | Gemcitabine 800 mg/m 2 Ifosfamide 2 g/m 2 (D 1, 8) Every 3 wk | Phase 2 | 34 | 21 | 9 |
| Lin et al, 2007 | Gemcitabine 800 mg/m 2 (D 1, 8, 15) Ifosfamide 1500 mg/m 2 (24-h infusion D 8–10) Every 4 wk | Phase 2 | 23 | 22 | 4.8 |
The combination of gemcitabine and paclitaxel has been the most extensively evaluated regimen in the second-line setting in advanced UC. Although the phase 2 studies have all used different dosing and treatment schedules, this combination can elicit objective responses ranging from 30% to 60% and a median OS of 11 to 14 months (see Table 2 ). A German phase 3 trial randomized patients to receive 6 cycles of gemcitabine and paclitaxel (group A) versus an additional maintenance therapy for gemcitabine and paclitaxel every 3 weeks until progression (group B). No significant difference in OS (group A, 7.5 months; group B, 6.8 months, P = .8) or overall RRs (group A, 34.5%; group B, 50.0%) was observed with the added maintenance dosing. It was also noted in the study that patients who had a previous major response to first-line chemotherapy had a trend toward a higher chance of response to second-line treatment ( P = .06), and patients with a median duration of response greater than 7.1 months to first-line therapy also had a significantly better response to second-line treatment.
In contrast, the combination of carboplatin and paclitaxel has modest efficacy, with RRs of only 16%, median PFS of 4 months, and median OS of 6 months. The triplet combination of carboplatin, docetaxel, and gemcitabine produced a high RR of 45% but was limited by significant dose-limiting neutropenia.
Studies have also evaluated the use of GC or methotrexate, vinblastine, adriamycin, and cisplatin (MVAC) as second-line regimens. In a study that enrolled 30 patients, who had progressed or relapsed after treatment with GC, the use of second-line MVAC produced an RR of 30% with a median PFS of 5.3 months and OS of 10.9 months, with grade 3 to 4 neutropenia, thrombocytopenia, and anemia occurring in 63.3%, 30%, and 16.7% of the patients, respectively. Similarly, GC after first-line MVAC produced an objective RR of 39.4% in 33 patients with a median survival of 10.5 months with similar rates of neutropenia (66.7%) and thrombocytopenia (30.3%).
Evaluation of targeted therapies in urothelial cancer
In recent years, genomic studies have shown the heterogeneous nature of UC. Many somatic mutations are expressed that may provide rational targets for novel targeted therapies. Multiple candidate genes with potential diagnostic and prognostic relevance from oncogenic signaling, cell cycle, tumor suppressor, and stromal angiogenesis pathways have been identified for both non–muscle-invasive and muscle-invasive bladder cancers.
For example, profiling of muscle-invasive UCs by TCGA identified the FGFR3, PI3-kinase/mTOR/AKT/TSC1, and ERBB2 (or HER2) pathways as potential targets for novel therapeutics based on the frequency of these alterations ( Fig. 1 ).
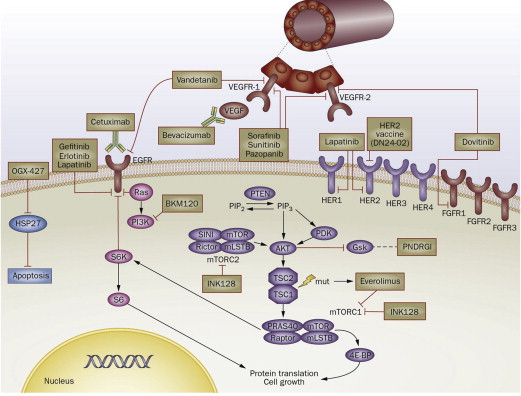
UCs that progress after cisplatin-based chemotherapy regimens are frequently resistant to other available chemotherapies, and, therefore, addition of targeted agents alone or in combination is a rational treatment strategy. Clinical trials have evaluated several novel agents, including those targeting angiogenesis (VEGF), growth factor receptors (EGFR, HER2, FGFR), and immunomodulatory agents in UC with variable levels of success. Table 3 lists the recently concluded trials evaluating targeted therapies in UC.
| Target | Agent | Type of Study | Chemotherapy | Number of Patients | RR (%) | OS (mo) |
|---|---|---|---|---|---|---|
| EGFR | Cetuximab | Randomized phase 2 | Paclitaxel and cetuximab vs | 39 | 25 | 10.5 |
| Cetuximab alone | 0 | 1.3 | ||||
| Lapatinib | Phase 2 | None | 59 | 3 | 4.5 | |
| Gefitinib | Phase 2 | None | 31 | 3 | 3 | |
| VEGF | Sorafenib | Phase 2 | None | 27 | 0 | 6.8 |
| Sunitinib | Phase 2 | None | 45 | 7 | 6.9 | |
| Aflibercept | Phase 2 | None | 22 | 4.5 | NR | |
| Pazopanib | Phase 2 | None | 19 | 0 | NR | |
| Pazopanib | Phase 2 | None | 41 | 17 | 4.7 | |
| VEGFR, EGFR | Vandetanib | Randomized phase 2 | Docetaxel and vandetanib vs | 142 | 7 | 5.56 |
| Docetaxel and placebo | 11 | 7.39 | ||||
| FGFR3 | Dovitinib | Phase 2 | None | 44 | 0 | NR |
| PI3k/Akt/mTOR | Everolimus | Phase 2 | None | 45 | 5 | 10.5 |
| SAHA: histone deacetylase | Vorinostat | Phase 2 | None | 14 | 0 | 4.3 |
| Pololike kinase 1 | Volasertib | Phase 2 | None | 31 | 19 | NR |
| Farnesyl transferase | Lonafarnib | Phase 2 | Gemcitabine | 31 | 32 | NR |
| Proteasome inhibitor | Bortezomib | Phase 2 | None | 20 | 0 | NR |
| Bortezomib | Phase 2 | None | 25 | 0 | 5.7 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




