St Bartholomew’s Hospital trial
The Boston study
Ref.
[9]
[10]
Published
1996
2003
Design
Single arm prospective study
Single arm prospective study.
Subjects
The low-risk asymptomatic women > or = 45 years of age. 22,000 volunteers
33,621 CA125 results from 9233 low-risk women older than 45 years for whom two or more serial samples were available
Recruitment
Between June 1, 1986 and May 1, 1990, London
Between June 1, 1986, and May 1, 1990
Strategy
CA125 measured annually for 1–4 years and a positive CA125 was recalled for ultrasound
CA125 II levels
Interpretation
A CA125 concentration > or = 30 U/mL
Calculation based on serial CA125 II levels
Results
The relative risk of developing ovarian and fallopian cancers within 5 years was increased 14.3-fold (8.5–24.3) after a CA125 cut-off > or = 30 U/mL and 74.5-fold (31.1–178.3) after a cut-off > or = 100 U/mL
The risk calculation significantly improved the area under the curve from 84 to 93% compared with a fixed cutoff for CA125. CA125 achieved a sensitivity of 62%
Mortality
Serial CA125 elevation is associated with an increase in risk of an index cancer in asymptomatic women older than 45 years. The mortality effect has not been reported as yet
Serial CA125 elevation improved the ovarian cancer detection rate in asymptomatic women. The mortality effect has not been reported as yet
4.3.2.2 Transvaginal Sonography
Transvaginal sonography (TVS) has been considered a primary imaging modality for diagnosing and evaluating adnexal masses. TVS has high specificity and sensitivity for detecting an adnexal mass based on a pattern recognition approach and morphological feature through gray-scale ultrasound. Table 4.2 is a summary of the findings of the four major ovarian cancer screening trials using TVS. These studies used gray-scale TVS as a primary screening modality [13, 14, 16, 17]. The percentage of the total number of stage I cases increased after the induction of screening (stage shift). It was not effective in detecting ovarian cancers in women who had normal ovarian volume. The use and role of Doppler ultrasonography as a screening technique are controversial. Color flow imaging for detection of ovarian cancer greatly improves specificity but at the expense of potential sensitivity in the triage of adnexal masses. Dr. van Nagell and his colleagues have reported some encouraging evidence of not only stage shift but also survival benefit by a single-arm prospective study, not a RCT [18]. A large-scale RCT is required for answering this question. Further, stringent quality control and quality assurance are necessary for TVS screening of asymptomatic postmenopausal women.
Table 4.2
A summary of the findings of the four major ovarian cancer screening trials using TVS
The London study | The First Kentucky study | The Hirosaki, Japan study | The Second Kentucky study | The Third Kentucky study | |
|---|---|---|---|---|---|
Ref. | [13] | [16] | |||
Published | 1993 | 2000 | 2000 | 2007 | 2011 |
Design | Single arm prospective study | Single arm prospective study | Single arm prospective study | Single arm prospective study | Single arm prospective study, not a RCT |
Subjects | 1601 self referred asymptomatic women aged 17 to 79 (mean 47) years, with a family history of ovarian cancer, aged 17 to 79 (mean 47) years. 60% were premenopausal | 14,469 asymptomatic women; women >/= 50 years of age in the general populations and women >/= 25 years of age with a family history of ovarian cancer | 51,550 low-risk asymptomatic women who participated in annual uterine cervical carcinoma screening. | 25,327 asymptomatic women aged > or = 50 years in the general populations and women aged > or = 25 years who had a family history of ovarian cancer | 37,293 asymptomatic women aged > or = 50 years in the general populations and women aged > or = 25 years who had a family history of ovarian cancer |
Recruitment | Between 1987 and 1999 | Between 1989 and 1999 | Between 1987 and 2005 | Between 1987 and 2011 | |
Strategy | Transvaginal ultrasonography with color blood flow imaging | Annual transvaginal sonography (TVS) | Annual transvaginal sonography (TVS) | Annual transvaginal sonography (TVS) | Annual transvaginal sonography (TVS). Women with abnormal screens underwent tumor morphology indexing, serum biomarker analysis, and surgery |
Interpretation | Morphological score > or = 5 and pulsatility index <1.0 | An abnormal sonogram | An abnormal sonogram (a mass > 30 mm in greatest dimension or a mass with a mixed pattern) | An abnormal sonogram | An abnormal sonogram |
Results | 61 women had a positive screening result (3.8%, 95% confidence interval 2.9 to 4.9%), six of whom had primary ovarian cancer detected at surgery (five stage Ia, one stage III) | 180 patients with persisting TVS abnormalities underwent exploratory laparoscopy or laparotomy. 17 ovarian cancers were detected: 11 Stage I, 3 Stage II, and 3 Stage III. Four and four patients developed ovarian cancer within 12 months of a negative scan and more than 12 months following a normal screen, respectively. Statistical variables: sensitivity, 81%; specificity, 98.9%; positive predictive value, 9.4%; and negative predictive value, 99.97% | Secondary screening was required for 5309 participants (10.3%). Surgery was performed on 324 participants. Twenty-two primary tumors and 2 metastatic tumors were detected for a diagnostic rate of 0.047%. 77.3% were classified as Stage I carcinoma. | Among 364 patients (1.4%) with a persisting ovarian tumor, 35 primary invasive ovarian cancers, 9 serous ovarian tumors of low malignant potential, and 7 cancers metastatic to the ovary were detected. Nine women developed ovarian cancer within 12 months of a negative screen. A sensitivity of 85.0%, specificity of 98.7%, positive predictive value of 14.0%, and negative predictive value of 99.9% | Forty-seven invasive epithelial ovarian cancers and 15 epithelial ovarian tumors of low malignant potential were detected. Stage distribution: stage I, 47%; stage II, 23%; stage III, 30%, and stage IV, 0%. The 5-year survival rate for all women with invasive index cancer detected by screening as well as interval cancers was 74.8% compared with 53.7% for unscreened women with ovarian cancer (P < 0.001) |
Mortality | TVU with color flow imaging can effectively detect early ovarian cancer in women with a family history of the disease. The mortality effect has not been reported as yet | A decrease in stage at detection (stage shift) and a possible decrease in case-specific ovarian cancer mortality | Stage shift may decrease the mortality of the disease. The mortality effect in comparison with the non-screening group has not been reported as yet | Stage shift. Although a significantly higher fraction of early-stage cancer was detected, they also had nine patients who developed ovarian cancer within 12 months of a normal scan. The mortality effect in comparison with the non-screening group has not been reported as yet. Although a significantly higher fraction of early-stage cancer was detected, they also had nine patients who developed ovarian cancer within 12 months of a normal scan | Some encouraging evidence of stage shift and survival benefit |
4.3.2.3 Two-Stage Strategies
Several studies have assessed the diagnostic value of combinations of CA125 and imaging concurrently or sequentially to augment the specificity and sensitivity for screening. Clinicians and public health informants were in consensus that the key issue is to reduce mortality. Table 4.3 is a summary of the key conclusions from the five major ovarian cancer screening trials using CA125 and TVS.
Table 4.3
A summary of the key conclusions from the five major ovarian cancer screening trials using CA125 and TVS
The First London study | The Second London study | Japanese Shizuoka Cohort Study of Ovarian Cancer Screening (SCSOCS) | Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial in the United States of America (USA) | United Kingdom Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) | |
|---|---|---|---|---|---|
Ref. | [19] | [20] | |||
Published | 1988 | 1999 | 2008 | 2016 | 2016 |
Design | Single arm prospective study | A pilot randomized controlled trial | RCT with 1 screening strategy in study group | RCT with 1 screening strategy in study group | RCT with 2 screening strategies in study group |
Subjects | 1010 low-risk asymptomatic postmenopausal women | The low-risk postmenopausal women aged 45 years or older. Randomized to a screened group (n = 10,958) or control group (n = 10,977) | 41,688 low-risk asymptomatic postmenopausal women. Either an intervention group (n = 41,688) or a control group (n = 40,799), with follow-up of mean 9.2 years | 78,216 low risk asymptomatic women aged 55 to 74 of whom 39,105 underwent screening | An RCT of 202,638 low risk asymptomatic women aged 50–74 years from the general population randomized in 2001–2005 to no intervention (control: 101,359) or annual screening using either TVS alone (50,639) or serum CA125 interpreted by a ‘Risk of Ovarian Cancer’ algorithm (ROCA) with TVS as a second line test (multimodal screening, MMS; 50,640) |
Recruitment | For an ovarian cancer screening programme | Between 1989 and 1998 | Between 1985 and 1999 | Between 1993 and 2007, at a median follow-up of 12.4 years (25th–75th centile 10.9–13.0) | Randomized in 2001–2005 |
Strategy | CA125 measurement and vaginal examination as initial tests and real-time ultrasonography as a secondary procedure in selected cases | Multimodal screening with sequential CA 125 and TVS to detect invasive epithelial cancers of the ovary or fallopian tube (index cancers). In the screened group, CA125 was measured annually for 3 years | Physical exam, ultrasound and CA125 concurrently | Ultrasound and CA125. The women were screened using serum CA125 and TVS for 4 years followed by CA125 alone for a further 2 years. The patients with pelvic lesions or an elevated CA125 level were referred to their local physicians for further management | Two screening arms (TVS) and CA125 followed by ultrasound (MMS) |
Interpretation | The normal range for serum CA125 in postmenopausal women was established | CA 125 was 30 U/mL or more | CA125 using a 35 U/mL cutoff | CA125 using a 35 U/mL cutoff and/or an abnormal sonogram | CA125 interpreted using the Risk of Ovarian Cancer algorithm (ROCA). The ROCA is a statistical tool that considers current and past CA125 values to determine ovarian cancer risk |
Results | The combinations of serum CA125 measurement with ultrasound and vaginal examination with ultrasound achieved specificities of 99.8% and 99.0%, respectively. 100% specificity was achieved by serum CA125 measurement with vaginal examination and by the combination of all three tests | Of 468 women in the screened group with a raised CA125, 29 were referred for a gynecological opinion; screening detected an index cancer in six and 23 had false-positive screening results. The positive predictive value was 20.7%. Median survival of women with index cancers in the screened group was 72.9 months and in the control group was 41.8 months (p = 0.0112). The number of deaths from an index cancer did not differ significantly between the control and screened groups (18 of 10,977 vs. nine of 10,958, relative risk 2.0 [95% CI 0.78–5.13]) | Encouraging sensitivity (77.1%) for primary ovarian cancer. Stage shift: more Stage I ovarian cancers in the screened group (63%) compared to the control (38%), which did not reach statistical significance. The Japanese screening trial enables diagnosis of EAOC at an early stage of the disease. | Lower sensitivity (69.5%); only 28% were Stage I/II. Abnormal TVS and elevated CA125 were found in 4.7%, and 1.4% of the participants, respectively. The positive predictive value for detection of ovarian cancer for CA125 alone and for TVS alone was 3.7% was 1.0%, respectively. The PPV for both tests combined was 23.5%, but 60% of early-stage disease would have been missed [5]. 118 and 100 deaths were reported in the screening and control arm, respectively, with a mortality rate ratio of 1.18 (95%CI 0.91–1.54) | Encouraging sensitivity (89.4% MMS/84.9% TVS) for primary index cancer; 84.9% MMS/75.0% TVS for primary invasive index cancer (47% MMS/50% TVS were Stage I/II). Superior sensitivity (88.6% vs 65.8%) and PPV (21.7% vs 5.8%) of MMS compared to the TVS arm for detection of primary invasive index cancers during incidence screening, with 40.3% in the MMS and 51.5% in the TVS arm detected at early stage |
Mortality | The combination of CA125 with ultrasound achieved acceptable specificity. The mortality effect has not been reported as yet | A larger randomized trial to see whether screening affects mortality | The mortality effect has not been reported as yet | No mortality benefit. Screening with concurrent CA 125 and TVS has no evidence of a mortality benefit | The stages at detection were relatively earlier (stage I/II: 44%) in the screening cohort. Although the mortality reduction was not significant in the primary analysis, researchers noted a significant mortality reduction with MMS when prevalent cases were excluded. MMS significantly reduced ovarian cancer mortality after excluding either deaths in the first 7 years after randomization or prevalent cancers. The large number of false positive surgeries (roughly 2100 surgeries) would be needed in order to prevent the small cancer deaths (about 40 deaths in each screening group) |
First, Jacobs and coworkers studied a group of 1010 asymptomatic postmenopausal women, comparing the specificities of individual evaluation or a combination of CA125, TVS, and pelvic examination (the first London study) [19]. Their study showed a specificity of 99.8% and 99.0% for CA125 plus TVS and CA125 plus pelvic examination, respectively, indicating that the combination of CA125 with TVS achieved acceptable specificity.
In the second study (a pilot randomized controlled trial in the second London study) conducted in the UK by Jacobs and coworkers, the specificity of CA125 alone or in combination with abdominal ultrasound was evaluated in postmenopausal women 45 years of age or above [20]. The subjects were divided into a control group (10,977) and a screened group (10,985). A total of 16 and 21 cancers were detected in the screened and control group, respectively, during the same interval. Median survival in the screened group (72.9 months) was significantly greater than in the control group (41.8 months) [20].
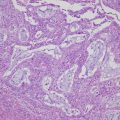
Third, the original intention in the Shizuoka study (RCT with one screening strategy in study group) conducted in Japan by Kobayashi and coworkers was to offer women in the intervention group annual screens by gynecological examination (sequential TVS and serum CA125 test) [21]. Women with abnormal TVS findings and/or elevated CA125 values were referred for surgical investigation by a gynecological oncologist. Twenty-seven index cancers were detected in the 41,688 screened women. Eight cancers were diagnosed outside the screening program. Among the 40,779 control women, 32 women developed ovarian cancer. The detection rate of early-stage ovarian cancer was elevated in the screened group compared with the controls, which did not reach statistical significance (63% vs 38%, p = 0.2285). Interestingly, sub-analysis assessment identified that the Shizuoka screening favorably detected certain histotypes such as clear cell and endometrioid types that are more common, low-grade, and less aggressive tumors in Japan. Since the progression of endometriosis to cancer is usually slow, recognition of patients at early stages may improve survival.
Fourth, the prostate, lung, colon, and ovary (PLCO) screening trial in the USA aimed to conduct concurrent testing of CA125 and TVS in the low-risk asymptomatic women between 55 and 74 years of age to determine if screening could reduce mortality in these cancers [22]. This RCT of screening versus usual care was initiated in 1993 and has studied 78,216 women. Data from the PLCO trial has not shown mortality benefit [15, 22, 23].
Finally, the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) used the risk of ovarian cancer algorithm (ROCA) to interpret the impact of CA125, which has shown an encouraging sensitivity and specificity [15]. The mortality reduction was not significant in the primary analysis, but this trial may have the potential to make an impact on survival benefit when prevalent cases were excluded [24]. The survival data from the UKCTOCS study provide a modest degree of hope.
Given the paucity of randomized controlled trial data, at present there is no effective screening test for ovarian cancer. The previous RCT results are unable to provide the impact on clinical survival benefit. This allowed us to explore the impact of growing insights into disease etiology and biomarker discovery on future screening strategies. In an era of promising advances in ovarian cancer screening, researchers have to focus on detecting low-volume disease using cancer-specific markers and targeted imaging. More cost-effective approaches might utilize novel biomarkers alone or in combination with imaging modalities in a more limited number of women.
4.3.3 Ovarian Cancer Screening in the High-Risk Population
Hereditary breast and ovarian cancer (HBOC) syndrome accounts for 5%–10% of breast cancers and 15% of invasive ovarian cancers [26]. Mutations in two genes, BRCA1 and BRCA2, are associated with HBOC. The average lifetime risk of EOC in the general populations is 1.3%, but the risk is markedly increased in women who carry mutations of the BRCA1 or BRCA2 (40% and 18% risk, respectively, by age 70 years) or the mismatch repair genes of hereditary nonpolyposis colorectal cancer (Lynch) syndrome (12% lifetime risk) [27–29]. Women with BRCA mutations have a markedly increased risk of early-onset breast, ovarian, pancreatic, and other cancers when compared to the risks in the general population. EOC is a spectrum of several subtypes, with different clinicopathological characteristics, possibly separate pathways of progression, and different sets of genetic and epigenetic characteristic of familial versus sporadic tumors. Since the molecular biology of the known hereditary disease may differ from that of sporadic cancer, separate trials and screening strategies may be required to detect hereditary and sporadic ovarian cancer. The overall occult gynecological carcinoma has been detected in 9.1% of BRCA mutation carriers [30]. Clinical guidelines are available for HBOC, such as those published by the National Comprehensive Cancer Network (NCCN), which include breast and ovarian cancer screening (surveillance) and risk-reducing interventions (risk-reducing surgical and medical options) [30, 31]. Published guidelines adopt standardized surveillance strategies that limit medication side effects, medical/surgical exposure without compromising cancer control and unnecessary cost, as well as enhance overall clinical and economic outcomes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree