Fig. 1
Range of surgical approaches to recurrent oropharyngeal squamous cell carcinoma (OPSCC). TLM Transoral laser microsurgery. TORS Transoral robotic surgery
Patient selection is critical to the successful application of surgery for recurrent OPSCC. Patient selection goes beyond simply identifying which patients may benefit from surgery. Rather, in the context of recurrent OPSCC, it also involves selecting which surgical approach is best suited for the disease. The broad surgical options for recurrent OPSCC include transmandibular, transcervical and transoral approaches.
3.1 Transmandibular Approaches
The mandible can represent a barrier to exposure for resection of recurrent OPSCC. Mandibulotomy or mandibulectomy may need to be considered depending on the extent of disease. A common scenario requiring mandibulectomy is direct tumor involvement of the pterygoid musculature with resulting severe trismus. Resection of the ascending ramus of the mandible may be necessary in such cases to afford exposure and an adequate lateral margin. For deeply invasive lateral pharyngeal cancers, the mandible may even be directly involved (Fig. 2). In other cases, a mandibulotomy may be useful for facilitating resection and reconstruction. This approach is most applicable to bulky recurrent OPSCC involving the base of tongue. Utilizing either a visor flap or a lip-splitting approach, the mandible may be divided and retracted laterally to allow broad access to the oropharynx (Fig. 3). Internal fixation is utilized to restore the mandibular arch at completion of the procedure. While these approaches greatly expand the scope of tumors that may be resected and reconstructed, they also entail significant additional morbidity. Complications from mandibulotomy or mandibulectomy include difficulty with speech, swallowing, malocclusion, temporomandibular joint pain and cosmetic deformity (Babin and Calcaterra 1976; Sessions 1983).
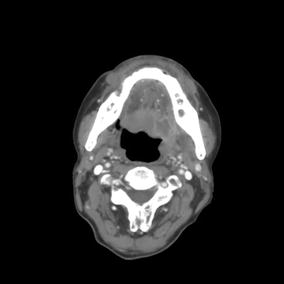

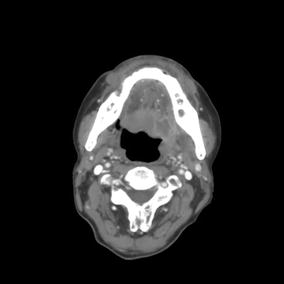
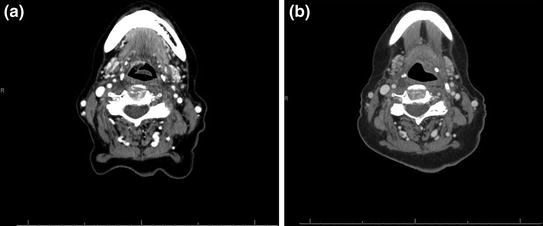
Fig. 2
Computed tomography (CT) neck with contrast demonstrating direct involvement of the mandible from recurrent left base of tongue oropharyngeal squamous cell carcinoma (OPSCC)

Fig. 3
Transmandibular approach for resection of recurrent right base of tongue oropharyngeal squamous cell carcinoma (OPSCC)
3.2 Transcervical Approaches
As an alternative to mandibulotomy or mandibulectomy, recurrent OPSCC of the tongue base, inferior tonsillar fossae or pharyngeal wall may be approached via a transcervical approach. Depending on the location of the cancer and the extent of exposure needed, a lateral pharyngotomy, transhyoid pharyngotomy and or suprahyoid pharyngotomy can be utilized. Acceptable oncologic outcomes have been reported using each of these approaches (Nasri et al. 1996; Zeitels et al. 1991). While transcervical approaches avoid many of the complications inherent in transmandibular surgery, the access afforded is substantially more limited. In addition, patients undergoing pharyngotomy are at increased risk of pharyngocutaneous fistula formation and long-term dysphagia.
Trancervical approaches to recurrent OPSCC also require considerable skill for proper execution. This is because a transcervical approach requires an “inside-out” understanding of the anatomy whereby at least some of the mucosal cuts are completed last. A transcervical approach is made even more challenging in the recurrent setting given fibrosis, induration and potential changes to the anatomy from prior therapies. For these reasons, transcervical approaches to recurrent OPSCC are infrequently reported.
3.3 Transoral Approaches
A transoral approach offers the quickest and most direct route to the oropharynx with the least potential for morbidity. The primary disadvantage of a transoral approach can be related to exposure. While the tonsil can often be adequately visualized directly, OPSCC involving the inferior tonsil, glossotonsillar sulcus or base of tongue may be difficult or impossible to reach through the mouth without specialized techniques and or instrumentation. Patient factors (trismus, kyphosis and dental obstruction) and tumor characteristics (tumor size and location) can limit direct visualization of the oropharynx, thereby preventing a direct transoral approach from being used.
Advancements in endoscopic surgery have led to the development of minimally invasive techniques that enable transoral surgery as an alternative to transmandibular and or transcervical approaches. TLM was the first minimally invasive technique to be applied to OPSCC (Moore and Hinni 2013). High-volume TLM surgeons have reported favorable oncologic outcomes using TLM for OPSCC. However, the technical challenges of this method have limited widespread adoption outside of select large academic centers. More recently, TORS has been applied to the management of OPSCC (Weinstein et al. 2012). Unlike TLM, TORS allows for en bloc resection of pathology and is not limited by line-of-site access. So the learning curve for TORS appears shorter than for TLM (White et al. 2013a). TORS using the da Vinci Surgical System (Intuitive Surgical, Inc. Sunnyvale, CA) was cleared by the Food and Drug Administration (FDA) in the United States in 2009. Since then, there has been a rapid rise in the use of TORS to treat OPSCC. In 2015, another robotic platform, the Flex Robotic System (MedRobotics Corp., Raynham, MA), was also approved for transoral surgery by the FDA. TORS has also been investigated for recurrent OPSCC.
In previously untreated patients with OPSCC, transoral approaches are most appropriate for addressing small-volume disease. In these cases, TLM or TORS is often being used with the intent of treatment de-intensification. For example, patients with early stage HPV-associated OPSCC (T1-2, N0-1) treated with TORS have the potential of single-modality therapy and avoiding radiation therapy (Brickman and Gross 2014). More advanced stage OPSCC can also be managed with TORS and de-intensified adjuvant therapies with the goal of potentially avoiding chemotherapy and limiting potential late toxicities (Weinstein et al. 2010). However, the utility of a transoral approach diminishes in patients with large volume or high tumor (T) classification primaries due to the challenges of obtaining negative surgical margins and the expected increased functional morbidity, without obviating the need for intensive adjuvant therapies.
The goal of a transoral approach is different in patients with recurrent OPSCC. In these cases, surgery may be the only available means of treatment or a method for treatment intensification. Small-volume recurrent OPSCC can be amenable to a transoral approach without reconstruction (Fig. 4). However, given the impact of prior radiation on wound healing and the risk of life threatening complications (e.g., bleeding) after transoral surgery, large-volume recurrent OPSCC may require simultaneous microvascular reconstruction. This is particularly important if re-irradiation is contemplated.