Conventional treatment for small cell lung cancer (SCLC) is currently thoracic radiation and combination chemotherapy, and surgery has been traditionally stated to have little to no role in disease management. However, a growing body of literature suggests that early-stage SCLC may be more amenable to local control following resection, with surgery being an important component of multimodality therapy. This article attempts to summarize what is currently known about early-stage SCLC, and outlines the methods by which this controversy is actively being investigated.
Nomenclature
Small cell lung cancer (SCLC) is estimated to account for approximately 13% of newly diagnosed lung cancers. It is considered distinct from non–small cell lung cancer (NSCLC), due to different biological and clinical patterns. Specifically, SCLC is known to have a more aggressive biology with rapid growth and early spread, as well as a common association with paraneoplastic syndromes. Of all histologic types of lung cancer, SCLC is the most sensitive to chemotherapy and radiation, but prognosis remains poor, with an overall median survival following treatment of 10 months and a 5-year survival of 5%.
SCLC is seen almost exclusively in smokers and is characterized by a rapid tumor doubling time, high growth fraction, and early development of metastases. The majority of patients present with extrathoracic metastases, but more sensitive imaging and screening modalities have resulted in better detection of early disease. The first staging of SCLC by severity was introduced by the Veterans’ Administration Lung Study Group (VALSG) in the 1950s. In that classification, limited disease (LD) was characterized by tumor confined to the ipsilateral hemithorax that can be safely included in a single radiation port. More widespread cancer was termed extensive disease (ED). Approximately 40% of all new SCLC diagnoses are LD, which historically has improved survival compared with ED, with a median survival of 16 months and a 12% 5-year survival following chemoradiotherapy.
In 1989, after the introduction of TNM staging, the International Association for the Study of Lung Cancer (IASLC) described LD SCLC as consistent with TNM stages IA to IIIB, with ED describing patients with distant metastases. Additionally in the IASLC nomenclature at that time, supraclavicular, hilar, and mediastinal nodes were included in LD. These modifications have been found to be somewhat more prognostic than the original VALSG, and continue to be used to estimate prognosis and guide treatment.
For decades, clinicians and clinical trial investigators have consistently commented that LD SCLC comprises a heterogeneous patient population, with little similarity in survival rates between patients presenting with a peripheral nodule and those with main bronchus tumors and lymphadenopathy. Recognizing this, in 1993 the Toronto Lung Oncology Group suggested relying more heavily on TNM staging rather than grossly grouping LD and ED. Patient survival in their cohort with clinical stages I and II was significantly better than those with stage III including N2 or N3 involvement. The same article also proposed a “very limited disease” category defined by small tumors with a negative mediastinoscopy.
Despite these data and subsequent recognition that dichotomous LD/ED staging of SCLC may not be as predictive a framework as TNM, particularly for surgical intervention, the use of these terms has persisted in clinical practice, due to the fact that by not routinely offering resection for SCLC, it has been more difficult to validate staging accuracy. Because almost all patients with LD are candidates for chemotherapy and radiation, the two-group system has not been as problematic while investigating those modalities. Meanwhile, several reports in the surgical literature have found that TNM staging for SCLC is predictive of outcome, particularly for low-stage tumors. For the purposes of this article, the term early stage (ES) will include clinical or pathologic stage IA through IIB.
Conventional treatment for SCLC is combination thoracic radiation and platinum-based multiagent chemotherapy (most often etoposide and cisplatin), with surgery traditionally thought to have no role in disease management. However, ES SCLC may be more amenable to local control following resection, with a growing body of literature suggesting that surgery is an important component of multimodality therapy. Here the authors attempt to summarize what is currently known about ES SCLC, and outline the methods by which this controversy is actively being investigated.
History of surgical literature
Before 1970 surgical resection was often used to treat SCLC; however, surgery was supplanted by radiation following the British Medical Research Council (MRC) report that radiotherapy alone provided better survival than surgery alone as primary therapy for patients with SCLC. Of note, despite the statistically significant difference between surgery and radiation, the mean survival was less than 1 year in both groups. Furthermore, data were analyzed by intention to treat, and included 37 patients who underwent exploratory thoracotomy only or no surgery in the analysis of the 71 patients in the surgical arm.
The Veterans Administration Surgical Oncology Group in 1982 retrospectively reviewed their experience with 132 patients with SCLC who had undergone resection, and reported as high as 60% 5-year survival for T1N0 lesions status post surgery and adjuvant chemotherapy. This rate was higher than adjuvant survival rates for later-stage disease, and led the investigators to conclude that resection is definitely indicated in patients with T1N0M0 lesions and probably indicated in those with T1N1M0 or T2N0M0 lesions. This study was an early proponent of the concept of more precise staging to determine candidacy for surgery.
In 1994, the Lung Cancer Study Group published a prospective randomized trial of induction chemotherapy followed by either surgery or radiation. Of the 328 patients initially treated with 5 cycles of cyclophosphamide, doxorubicin, and vincristine, 146 responders were randomized to surgery or no surgery. All patients received radiation therapy to the chest and brain. There was no difference in survival between the two arms, with a median survival time of 16 months and a 2-year survival rate of 20%. However, patients with stage I were specifically excluded from this trial. This study has been the only randomized one to date comparing surgery and chemotherapy, and is often cited as the primary rationale to not offer resection for SCLC. There have been no published randomized trials conducted using a modern chemotherapy regimen (platinum-based) in ES disease.
History of surgical literature
Before 1970 surgical resection was often used to treat SCLC; however, surgery was supplanted by radiation following the British Medical Research Council (MRC) report that radiotherapy alone provided better survival than surgery alone as primary therapy for patients with SCLC. Of note, despite the statistically significant difference between surgery and radiation, the mean survival was less than 1 year in both groups. Furthermore, data were analyzed by intention to treat, and included 37 patients who underwent exploratory thoracotomy only or no surgery in the analysis of the 71 patients in the surgical arm.
The Veterans Administration Surgical Oncology Group in 1982 retrospectively reviewed their experience with 132 patients with SCLC who had undergone resection, and reported as high as 60% 5-year survival for T1N0 lesions status post surgery and adjuvant chemotherapy. This rate was higher than adjuvant survival rates for later-stage disease, and led the investigators to conclude that resection is definitely indicated in patients with T1N0M0 lesions and probably indicated in those with T1N1M0 or T2N0M0 lesions. This study was an early proponent of the concept of more precise staging to determine candidacy for surgery.
In 1994, the Lung Cancer Study Group published a prospective randomized trial of induction chemotherapy followed by either surgery or radiation. Of the 328 patients initially treated with 5 cycles of cyclophosphamide, doxorubicin, and vincristine, 146 responders were randomized to surgery or no surgery. All patients received radiation therapy to the chest and brain. There was no difference in survival between the two arms, with a median survival time of 16 months and a 2-year survival rate of 20%. However, patients with stage I were specifically excluded from this trial. This study has been the only randomized one to date comparing surgery and chemotherapy, and is often cited as the primary rationale to not offer resection for SCLC. There have been no published randomized trials conducted using a modern chemotherapy regimen (platinum-based) in ES disease.
Justification for surgery
The MRC trial effectively slowed the investigation of surgery for SCLC for 2 decades following its publication. However, there have been several strong criticisms of the conclusions. Most notably, there were few ES patients in the cohort, and subgroup analysis was not performed. In the 1994 Lung Cancer Study Group randomized trial, patients with T1N0 lesions were excluded and the study was performed before the advent of platinum-based modern chemotherapy. Despite these findings historically, for many practitioners there is strong intuitive rationale for the use of surgery in ES. Accordingly it continues to be investigated, and data are emerging to support the hypothesis that when staged appropriately, there is a benefit for resection in select cases. The arguments for surgery generally revolve around efficacy of local control and uncertainties in histologic diagnosis.
Local control
Local recurrence of SCLC after disease treatment can be at the primary tumor site as well as via lymphatic spread. Current chemoradiation regimens have a local failure rate approaching 50%. However, there are data to suggest that following surgical resection, local control may approach 85% to 90%, and when surgery has been directly compared with chemoradiation there has been a significantly lower rate of local recurrence after surgical resection.
Uncertainties in histologic diagnosis
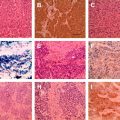
Small carcinoid tumors with no nodal involvement can occasionally be misdiagnosed as ES SCLC by needle biopsy. Furthermore, as many as one-quarter of resected SCLCs are found to be histologically mixed with other types (such as NSCLC). Because NSCLC tumors are less sensitive to current chemoradiotherapies, there is a risk of residual or refractory disease if treated without resection. Furthermore, after failure of chemotherapy, surgery has been shown to commonly reveal mixed histologies that are more amenable to surgery. In the event of survival for 2 years or more after SCLC diagnosis, new tumors should be considered as possibly NSCLC, although resection in that context has a lower median survival than resection for primary NSCLC (25 vs 58 months, respectively).
Studies in the modern era
Since the introduction of the TNM staging system, several retrospective and prospective nonrandomized reports have noted the benefits of surgical resection for patients with ES SCLC. A selection of these series is compared in Table 1 , with patient outcomes by stage as reported. Of note, there appears to be an effect of tumor stage on 5-year survival whenever surgery is offered as a primary treatment, and the survival rates for ES patients in these studies are higher than those reported for conventional treatment with modern platinum-based chemotherapy.
| Authors, Ref. Year | N | Study Design | Regimen | Overall 5-Year Survival, % by Stage (Pathologic When Available) | |||
|---|---|---|---|---|---|---|---|
| Stage I | Stage II | Stage III | Overall | ||||
| Fujimori et al, 1997 | 22 | Prospective | Induction PE ± D | 73 (I + II) a | 43 a | 67 a | |
| Rea et al, 1998 | 104 | Prospective | CAV or PEB, adjuvant for Stage I–II, induction for Stage III | 52 | 30 | 15 | 32 |
| Eberhardt and Korfee, 2003 | 46 | Prospective | Induction PE | 44 (IIB + IIIA) | 39 | ||
| Rostad et al, 2004 | 38 | Retrospective | 45 | 6 (IIIB) | |||
| Badzio et al, 2004 | 67 | Retrospective with case-matched control | Adjuvant PE or CAV | 27 | |||
| Brock et al, 2005 | 23 | Retrospective | 22% induction, 55% adjuvant, 22% surgery alone or unspecified | 86 | 68 | ||
| Tsuchiya et al, 2005 | 61 | Prospective | 70 | 38 | 39 | 57 | |
| Granetzny et al, 2006 | 95 | Retrospective | 43 (I + II) | ||||
| Bischof et al, 2007 | 39 | Retrospective | Adjuvant PE | 49 (I + II) | |||
| Lim et al, 2008 | 59 | Retrospective | 24% adjuvant, regimen unknown | 60 | 50 | 50 | 52 |
| Vallieres et al, 2009 | 349 | Retrospective (IASLC database) | Various | 48 | 39 | 12 | 30 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree