Neuroendocrine tumors (NETs) are rare epithelial neoplasms with neuroendocrine differentiation originating most commonly in the lungs and gastroenteropancreatic. Treatment includes surgery and other local therapies; treatment of inoperable disease centers around symptom management and control of tumor growth. Somatostatin analogues (SSAs) have been a mainstay of managing hormone-related symptoms. Emerging evidence suggests that they are effective therapies for tumor control also. Peptide receptor radionuclide therapy with radiolabeled SSAs is a new, promising treatment for inoperable or metastatic NETs. This article reviews the role of SSAs in the treatment of NETs.
Key points
- •
Functional neuroendocrine tumors (NETs) cause various clinical symptoms depending on the activity of the hormone secreted.
- •
Carcinoid syndrome, the classic example of a functional NET, is caused by serotonin overproduction and leads to flushing, diarrhea, edema, telangiectasia, bronchospasm, and hypotension.
- •
Somatostatin receptors (SSTRs) are expressed in NETs, with SSTR-2 expression being predominant in gastroenteropancreatic NETs.
- •
Somatostatin analogues (SSAs) control clinical symptoms arising from hormone excess in SSTR-expressing NETs.
- •
Recently published data from have established the antiproliferative effects of SSAs and their role in control of tumor growth.
Introduction
Neuroendocrine tumors (NETs) are epithelial neoplasms with neuroendocrine differentiation that arise in various anatomic locations throughout the body. The annual incidence of NETs in the United States is about 3.65 per 100, 000 and recent analyses have indicated a rise in the incidence of carcinoid tumors in the United States and elsewhere, owing in part to improvements in diagnostics and increased awareness.
The clinical presentation of carcinoid tumors can be variable, depending on their anatomic site of origin. Whereas patients with indolent disease can remain asymptomatic for years, some patients may present with symptoms related to tumor bulk or from secretion of various peptides or amines from these tumors. Such secretory tumors, also called “functional tumors,” cause various clinical symptoms depending on the activity of the hormone secreted. The minority of NETs are truly functional; approximately 10% of patients with small bowel NETs and 40% of patients with pancreatic NETs meet this definition. Carcinoid syndrome, caused by serotonin overproduction, is the classic example of a functional NET and is associated with symptoms such as flushing, diarrhea, edema, telangiectasia, bronchospasm, and hypotension. These symptoms occur when the secretory products from the NETs bypass metabolism in the liver and enter the systemic circulation directly. This usually occurs in the presence of liver metastases, bulky retroperitoneal disease, or primary sites of disease outside the gastrointestinal tract. Hindgut tumors (ie, transverse, descending, and sigmoid colon; rectum; and genitourinary) are rarely functional and almost never associated with classic carcinoid syndrome. Table 1 lists examples of various clinical syndromes arising from hormone secretion in gastroenteropancreatic (ETs).
| Syndrome | Secreted Hormone(s) | Symptom(s) |
|---|---|---|
| Intestinal neuroendocrine tumors | ||
| Carcinoid syndrome | 5-hydroxytryptamine (5-HT) Prostaglandin Substance P Gastrin Vasoactive intestinal polypeptide Prostaglandin Serotonin Bradykinin Kallikrein Histamine | Abdominal pain Secretory diarrhea Flushing Heart disease Telangiectasias (face) Bronchospasm Arthropathy Hypotension Pellagra |
| Pancreatic neuroendocrine tumors | ||
| Calcitoninoma | Calcitonin | Diarrhea, facial flushing |
| CRHoma | Corticotropin release hormone | Cushing’s syndrome |
| Gastrinoma | Gastrin | Zollinger Ellison syndrome (peptic ulcers) |
| GHRHoma | Growth hormone releasing hormone | Acromegaly |
| Glucagonoma | Glucagon | Necrolytic migratory erythema Cheilitis Diabetes mellitus Anemia Weight loss Diarrhea Venous thrombosis Neuropsychiatric symptoms |
| Insulinoma | Insulin | Hypoglycemia |
| PPoma | Pancreatic polypeptide | Considered nonfunctioning |
| Somatostatinoma | Somatostatin | Diabetes mellitus Cholelithiasis Diarrhea with steatorrhea |
| VIPoma | Vasoactive intestinal polypeptide | Watery diarrhea Hypokalemia Hypochlorhydria Dehydration Weight loss Flushing Hypercalcemia Hyperglycemia |
The management of NETs is multidisciplinary. For patients with unresectable and metastatic disease the intent is 2-fold: controlling tumor growth and alleviating symptoms arising from peptide hormone secretion. The treatment options for tumor control include observation (stable disease and mild tumor burden), systemic therapy with somatostatin (SST) analogues (SSAs), molecularly targeted agents and cytotoxic chemotherapies, cytoreductive surgery, and regional therapies (hepatic arterial embolization and ablative procedures). SSAs are the mainstay for control of hormone secretion. Recently, SSAs have also been recognized as antiproliferative agents in well-differentiated metastatic disease. This article reviews the application and role of SSAs in the treatment of well-differentiated NETs.
Introduction
Neuroendocrine tumors (NETs) are epithelial neoplasms with neuroendocrine differentiation that arise in various anatomic locations throughout the body. The annual incidence of NETs in the United States is about 3.65 per 100, 000 and recent analyses have indicated a rise in the incidence of carcinoid tumors in the United States and elsewhere, owing in part to improvements in diagnostics and increased awareness.
The clinical presentation of carcinoid tumors can be variable, depending on their anatomic site of origin. Whereas patients with indolent disease can remain asymptomatic for years, some patients may present with symptoms related to tumor bulk or from secretion of various peptides or amines from these tumors. Such secretory tumors, also called “functional tumors,” cause various clinical symptoms depending on the activity of the hormone secreted. The minority of NETs are truly functional; approximately 10% of patients with small bowel NETs and 40% of patients with pancreatic NETs meet this definition. Carcinoid syndrome, caused by serotonin overproduction, is the classic example of a functional NET and is associated with symptoms such as flushing, diarrhea, edema, telangiectasia, bronchospasm, and hypotension. These symptoms occur when the secretory products from the NETs bypass metabolism in the liver and enter the systemic circulation directly. This usually occurs in the presence of liver metastases, bulky retroperitoneal disease, or primary sites of disease outside the gastrointestinal tract. Hindgut tumors (ie, transverse, descending, and sigmoid colon; rectum; and genitourinary) are rarely functional and almost never associated with classic carcinoid syndrome. Table 1 lists examples of various clinical syndromes arising from hormone secretion in gastroenteropancreatic (ETs).
| Syndrome | Secreted Hormone(s) | Symptom(s) |
|---|---|---|
| Intestinal neuroendocrine tumors | ||
| Carcinoid syndrome | 5-hydroxytryptamine (5-HT) Prostaglandin Substance P Gastrin Vasoactive intestinal polypeptide Prostaglandin Serotonin Bradykinin Kallikrein Histamine | Abdominal pain Secretory diarrhea Flushing Heart disease Telangiectasias (face) Bronchospasm Arthropathy Hypotension Pellagra |
| Pancreatic neuroendocrine tumors | ||
| Calcitoninoma | Calcitonin | Diarrhea, facial flushing |
| CRHoma | Corticotropin release hormone | Cushing’s syndrome |
| Gastrinoma | Gastrin | Zollinger Ellison syndrome (peptic ulcers) |
| GHRHoma | Growth hormone releasing hormone | Acromegaly |
| Glucagonoma | Glucagon | Necrolytic migratory erythema Cheilitis Diabetes mellitus Anemia Weight loss Diarrhea Venous thrombosis Neuropsychiatric symptoms |
| Insulinoma | Insulin | Hypoglycemia |
| PPoma | Pancreatic polypeptide | Considered nonfunctioning |
| Somatostatinoma | Somatostatin | Diabetes mellitus Cholelithiasis Diarrhea with steatorrhea |
| VIPoma | Vasoactive intestinal polypeptide | Watery diarrhea Hypokalemia Hypochlorhydria Dehydration Weight loss Flushing Hypercalcemia Hyperglycemia |
The management of NETs is multidisciplinary. For patients with unresectable and metastatic disease the intent is 2-fold: controlling tumor growth and alleviating symptoms arising from peptide hormone secretion. The treatment options for tumor control include observation (stable disease and mild tumor burden), systemic therapy with somatostatin (SST) analogues (SSAs), molecularly targeted agents and cytotoxic chemotherapies, cytoreductive surgery, and regional therapies (hepatic arterial embolization and ablative procedures). SSAs are the mainstay for control of hormone secretion. Recently, SSAs have also been recognized as antiproliferative agents in well-differentiated metastatic disease. This article reviews the application and role of SSAs in the treatment of well-differentiated NETs.
Somatostatin and somatostatin receptor physiology
SST is a peptide hormone that was initially discovered as an inhibitor of growth hormone release in the hypothalamus of rats. Subsequent studies found that SST was secreted by paracrine cells scattered throughout the gastrointestinal tract, and also found in various locations in the nervous system. The physiologic effects of SST are largely inhibitory, and it has been known to reduce gastrointestinal motility and gallbladder contraction; inhibit secretion of most gastrointestinal hormones, including insulin, glucagon, and gastrin; reduce blood flow in the gastrointestinal tract; and inhibit growth hormone release from the pituitary and neurotransmission in the brain.
SST mediates its primarily inhibitory effects by binding to at least 5 high-affinity G-protein-coupled membrane receptors (SSTR1–5). The antiproliferative actions of SST result from cell cycle arrest and/or apoptosis downstream from tumor SSTR activation, and SSTR-induced inhibition of tumor angiogenesis and the production of factors that support tumor growth. The SSTRs share about 40% to 60% homology, but mediate different biological actions upon activation. All 5 SSTRs have been identified throughout the central nervous system, the gastrointestinal tract, and endocrine and exocrine glands, as well as on inflammatory and immune cells. Tumors arising from SST target tissues, such as the pancreas and small intestine, express a high density of SSTRs. The expression of SSTR2 has been noted to be predominant in most gastroenteropancreatic NETs. Well-differentiated tumors express SSTRs more often, and at higher density, than do poorly differentiated tumors.
Clinical application of somatostatin and synthetic analogues
The inhibitory effects of SST were initially recognized in the 1970s. However, given its short half-life requiring a cumbersome continuous infusion and rebound hypersecretion of hormones, its routine clinical application was limited. Given the limitations of native SST, synthetic analogues were developed from the early 1980s to present time and these include octreotide, lanreotide, and pasireotide. These peptides are more resistant to degradation and their half-lives and hence their biological activities are substantially longer than native SST (1.5–2 h vs 1–2 min). They vary in their affinity toward different SSTR subtypes, and bind mainly to SSTR2, and much less to SSTR5. The newly developed SSA pasireotide is a new ‘universal’ or ‘pan-receptor’ SSA, having a high affinity for SSTR 1, 2, 3, and 5 subtypes. Although initially approved for the treatment of acromegaly, the clinical application of SSAs now extends to multiple indications, such as the treatment of secretory diarrhea, gastrointestinal bleeding, inhibition of tumor growth, treatment of functional NET, and for the imaging of NETs.
Somatostatin analogues in the treatment of neuroendocrine tumors
In patients with NETs, indications for the use of an SSA include the treatment of symptoms arising from clinical syndromes caused by hormone excess, and for control of tumor growth. The SSAs are also used perioperatively for the prevention of carcinoid crisis.
Controlling Symptoms Arising From Hormone Excess
SSAs can control hypersecretion in NETs that express SST receptors. These include functional NETs such as glucagonomas, VIPomas, gastrinomas, and metastatic insulinomas. Octreotide was the first SSA developed for this clinical indication, and has a half-life of 2 hours and high affinity toward SSTR 2 and 5. This short-acting formulation of octreotide requires administration by continuous infusion or as a subcutaneous injection 2 to 3 times per day, and is not associated with the side effect of rebound hormonal hypersecretion. Octreotide long-acting release (LAR), a longer acting formulation, was developed in the 1990s to provide more sustained drug levels and is administered at 20 to 30 mg as a monthly intramuscular (IM) injection. Studies comparing the shorter acting and longer acting forms of octreotide have demonstrated equal efficacy in terms of symptom control, with symptomatic response rates of 60% to 72% across groups. For adequate symptom control during the initial administration of octreotide LAR, coverage with short acting octreotide for the initial 2 to 3 weeks is recommended until steady-state levels of octreotide LAR are achieved.
Lanreotide is another SSA with similar SSTR binding affinity as octreotide. Lanreotide has 2 formulations that are currently available, lanreotide sustained release (LA), given as an IM injection every 2 weeks and lanreotide prolonged release (Somatuline Autogel), given as a deep subcutaneous injections every 4 weeks. Lanreotide is approved both in Europe and the United States for the treatment of acromegaly. In a number of small prospective and retrospective studies, lanreotide has led to improvement of symptoms associated with carcinoid syndrome. Short-acting octreotide and lanreotide LA have also demonstrated equal efficacy in controlling carcinoid syndrome. Additionally, in a recent phase III study (A Double-blind, Randomized Placebo-controlled Clinical Trial Investigating the Efficacy and Safety of Somatuline Depot (Lanreotide) Injection in the Treatment of Carcinoid Syndrome [ELECT]) of lanreotide versus placebo in SSA-naïve patients or those responsive to conventional doses of octreotide, lanreotide reduced the need for short-acting octreotide (49% vs 34%, absolute difference 15%; P = .02). A large cross-sectional observation study evaluated patient-reported satisfaction with lanreotide use for carcinoid syndrome, and found that patients achieved good and sustained control of symptoms arising from carcinoid syndrome.
Pasireotide was developed as an agent with a broader SSTR profile similar to that of natural SST. It binds with high affinity to SSTR subtypes SSTR 1, 2, 3, and 5 and displays a 30- to 40-fold higher affinity for SSTR1 and SSTR5 than octreotide or lanreotide. Given its greater binding affinity, it has been hypothesized that it may have a greater inhibitory effect than octreotide on hormones secreted by carcinoid tumors. A multicenter, randomized, blinded phase III study of pasireotide LAR versus octreotide LAR in patients with symptomatic metastatic NET demonstrated equal efficacy of both these drugs in controlling symptoms of hormone secretion. The safety profile was similar with the exception of hyperglycemia, which was higher in the pasireotide arm (11% vs 0%).
Dosing of Somatostatin Analogues for Hormone-Related Symptoms
When SSAs are used for symptom control, it is recommended to start short-acting SSA immediately in an effort to provide immediate symptom relief and then overlap with long-acting SSA until steady-state levels are reached (approximately 2 weeks). The suggested starting dose of octreotide acetate ranges from 100 to 600 μg/d in 2 to 4 divided doses; test doses are not required routinely. Doses are initiated usually at the lower dose range and can be individually titrated to control symptoms; some patients may require significantly higher doses (≤1.5 mg/d). The recommended dose of octreotide LAR is 20 to 30 mg by deep IM injection repeated every 4 weeks. Correct IM injection can be challenging. One report noted that only 52% of injections were delivered successfully and correct IM injection was associated with improved control of flushing among patients with carcinoid syndrome. Some patients also require “rescue” doses of short-acting octreotide for control of breakthrough symptoms even after initiation of the long-acting formulation; this commonly occurs in the days preceding a scheduled octreotide injection. Dose and frequency of both short- and long-acting SSAs may be increased further for symptoms control as needed. The duration of treatment with SSAs is usually lifelong, unless there is loss of symptom control or occurrence of unmanageable side effects. The risk of tachyphylaxis after long-term use of SSAs has been postulated, although the mechanism of tachyphylaxis is poorly understood and rigorous prospective data are lacking.
The dosing of SSAs in elderly patients with carcinoid syndrome requires special mention, particularly given that the majority of NET patients are diagnosed in their 70s. In a recent study of the Surveillance, Epidemiology, and End Results–Medicare databases, Yao and colleagues showed that only 50% of elderly patients with US Food and Drug Administration–approved indications (carcinoid syndrome or metastatic disease) started Octreotide LAR within 6 months of diagnosis. Octreotide LAR use was lowest among patients aged 80 years and older. Also, the use of octreotide LAR within 6 months of diagnosis of carcinoid syndrome was associated with better survival for patients with metastatic disease. This study suggests that SSA use in elderly patients with functional NETs may be underused and should be evaluated in future studies.
Control of Tumor Growth
SSAs have also demonstrated antiproliferative properties in NETs with varying effect depending on primary site and SSTR subtype. For example, SSTRs 2 and 5 have been shown to mediate the antimitotic activity leading to cell cycle arrest. SSAs may also exert an indirect antiproliferative effect by inhibiting the release of growth factors and various trophic hormones such as growth hormone, insulin-like growth factor-1, insulin, gastrin, and epidermal growth factor, both from the neoplastic cell and from the surrounding tumor matrix. SSAs have also been postulated to reduce the vascularization of the neoplastic tissue in experimental models via inhibition of vascular endothelial growth factor.
The first clinical trial to demonstrate the antiproliferative effect of SSAs in NETs was the PROMID (Placebo controlled, double-blind, prospective, Randomized study on the effect of Octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors) study. In this phase III randomized, double-blind, placebo-controlled, multiinstitutional German study 85 patients with well-differentiated metastatic midgut NETs were randomized to receive 30 mg octreotide LAR monthly via IM injection versus placebo. In 85 enrolled patients, octreotide significantly improved time to progression when compared with placebo (14.3 vs 6 months in the placebo arm; hazard ratio, 0.34; 95% CI, 0.20–0.59; P = .000072); median overall survival (OS) could not be calculated at the time of initial analysis. The study also found that functionally active and inactive tumors responded similarly and the most favorable effect was observed in patients with low hepatic tumor volume and resected primary tumors. Updated OS data were presented in 2013; median OS was not reached in the octreotide LAR arm versus 84 months in the placebo arm (hazard ratio, 0.85; 95% CI, 0.46–1.56; P = .59). Although this study did not formally impact the US Food and Drug Administration label for octreotide LAR, octreotide was adopted widely for controlling tumor growth in patients with metastatic midgut NETs.
The CLARINET (Controlled study of Lanreotide Antiproliferative Response In NeuroEndocrine Tumors) study was a phase III randomized, double-blind, placebo-controlled, multinational study of lanreotide in patients with advanced, well-differentiated or moderately differentiated, nonfunctioning, SST receptor–positive NETs of grade 1 or 2 (with a Ki-67 antigen of <10%). Patients were randomized to receive lanreotide 120 mg via a deep subcutaneous injection every 28 days versus placebo. In 205 enrolled patients, lanreotide significantly improved progression-free survival when compared with placebo (median not reached vs 18.0 months; hazard ratio, 0.47; 95% CI, 0.30–0.73, P <.001); there was no difference in median OS. In an open-label extension study, 88 patients from the CLARINET core study continued on lanreotide (41 from the lanreotide arm and 47 from the placebo arm.) Of the subset of patients who had progressive disease while on placebo in the core study, median time to further progression was 14 months.
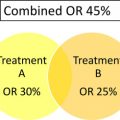
The PROMID and CLARINET studies demonstrate the antiproliferative effect of SSAs in the treatment of NETs. However, there are key differences between these studies worth highlighting ( Table 2 ). Most notably, PROMID included patients with small bowel NETs, grade 1 tumors, low hepatic tumor volume, and a relative short interval from diagnosis. CLARINET included a broader patient population with a predominance of pancreas and small bowel primary sites, both grade 1 and 2 tumors (Ki67 <10%), greater hepatic tumor volume, a majority of patients with stable disease during a 3 to 6 months before the study observation period, and a longer median time from diagnosis. CLARINET contributes new information to the field because it demonstrates activity of SSAs in pancreas, hindgut, and unknown primary NETs with higher grade and higher hepatic tumor volume. This study raises an important question, as to whether we should be using SSAs in patients with stable disease. Notably, the 18-month median progression-free survival in the placebo arm is encouraging and may provide evidence that active surveillance in select patients is reasonable. The CLARINET study has not demonstrated an OS difference, which could be attributed to crossover, need for longer follow-up, and perhaps a more indolent disease as evidenced by a longer time from diagnosis as compared with PROMID. Other completed and ongoing clinical trials evaluating SSAs for control of tumor growth in NETs are summarized in Tables 3 and 4 .