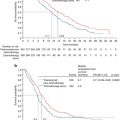
Fig. 18.1
OR setup. The patient is in left lateral position. The robot is docked from the dorsocranial side
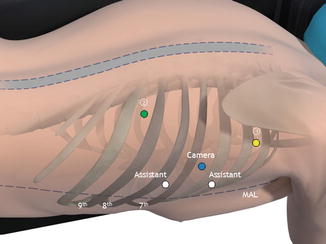
Fig. 18.2
Port position. Robotic arms 1 (yellow), 2 (green) and camera (blue). Two assisting ports (white)
Operative Steps
After division of any pulmonary adhesions and a proper overview of the operating field is achieved, the right pulmonary ligament is divided. The parietal pleura is dissected at the anterior side of the esophagus from the diaphragm up to the azygos arch. The azygos arch is carefully ligated with robotic hemoloc clips (Fig. 18.3a, b). Then dissection of the parietal pleura is continued above the aortic arch for a right paratracheal lymph node dissection. The right vagal nerve is dissected below the level of the carina. Subsequently, the parietal pleura is dissected at the posterior side of the esophagus cranially to caudally along the azygos vein, including the thoracic duct. Paratracheally left, the left recurrent nerve is identified and carefully protected. At the level of the diaphragm, the thoracic duct is clipped with a 10-mm endoscopic clipping device (Endo ClipTM II; Covidien, Mansfield, Massachusetts, USA) to prevent postoperative chylous leakage (Fig. 18.4a, b).
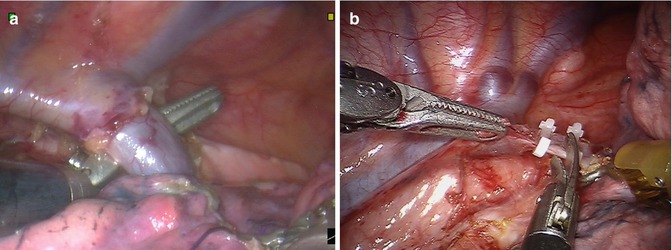
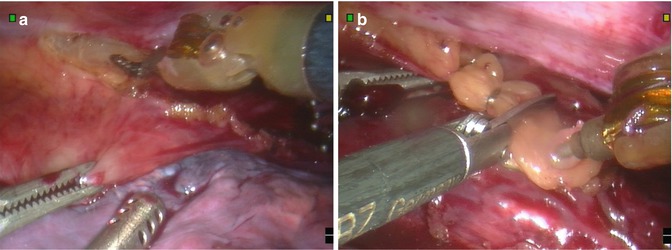
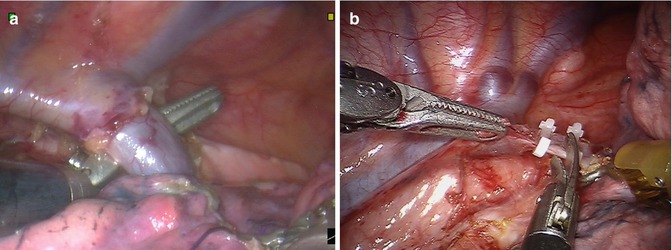
Fig. 18.3
(a) Identification of the azygos vein (AV). (b) Division of the azygos vein over the esophagus
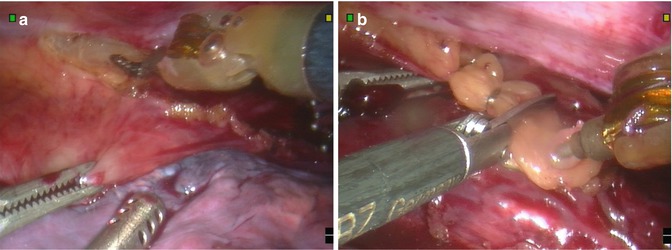
Fig. 18.4
(a) The thoracic duct (TD) is identified. (b) The thoracic duct (TD) is identified, clipped at the level of the diaphragm, and divided
At the level of the diaphragm, a Penrose drain is placed around the esophagus to provide traction, which facilitates esophageal mobilization (Fig. 18.5). The esophagus is then resected en bloc with the surrounding mediastinal lymph nodes and the thoracic duct from the diaphragm up to the thoracic inlet. Aortoesophageal vessels are identified and clipped by the assisting surgeon. The extensive lymphadenectomy includes the right- and left-sided paratracheal (lymph node station 2R, 2L), tracheobronchial (lymph node station 4), aortopulmonary window (station 5), carinal (station 7), and periesophageal (station 8) lymph nodes. A 24-Fr chest tube is placed, and the lung is insufflated under direct vision.
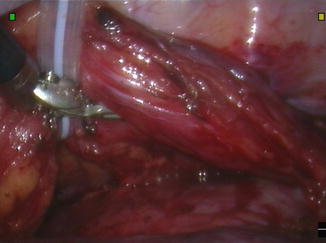
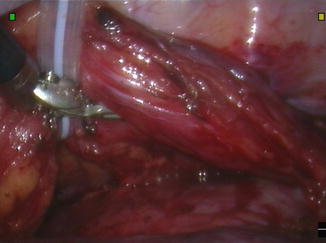
Fig. 18.5
A Penrose drain (PD) is placed around the esophagus (E) at the level of the pericardium to retract the esophagus anteriorly
Laparoscopic Dissection (Video 18.1)
Instruments
Harmonic scalpel
2× fenestrated bowel clamps
Endopaddle
Clipper
Hem-o-lok® Ligation clips
Positioning
After completion of the robot-assisted thoracoscopic esophageal mobilization, the patient is put in supine position. An 11-mm camera port is introduced left paraumbilically, and an 11-mm working port is placed at the right midclavicular line at the umbilical level. A 5-mm working port is placed more cranially at the right midclavicular line. A 5-mm assisting port is placed in the left subcostal area, and a 12-mm port is placed pararectally right for the liver retractor (Fig. 18.6). The abdomen is insufflated to a carbon dioxide pressure level of 15 mmHg.
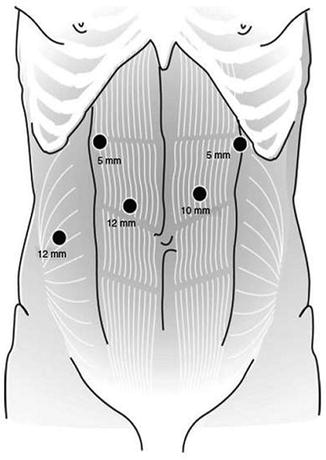
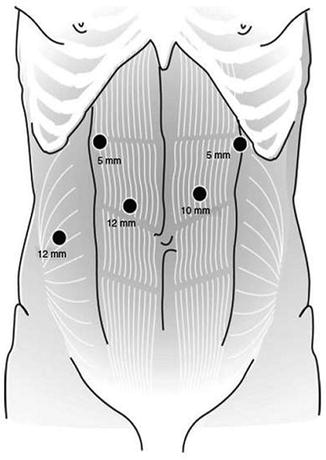
Fig. 18.6
Laparoscopic trocar placement
Operative Steps
The hepatogastric ligament is opened. The greater and lesser curvatures are dissected with ultrasonic harmonic scalpel (Harmonic Ace®, Ethicon Endo-Surgery, Johnson & Johnson, New Brunswick, New Jersey, USA). The hiatus is opened, and the distal esophagus is dissected from the right and left crus. The carbon dioxide pressure level is reduced to 6 mmHg to avoid excessive intrathoracic pressure, and a chest tube is placed in the left pleural sinus. Dissection and lymphadenectomy then continue around the celiac trunk. The left gastric artery and vein then are transected at their origin with Hem-o-lok® Ligation clips (Teleflex Medical, NC, USA). Abdominal lymphadenectomy includes lymph nodes surrounding the left gastric artery and the lesser omental lymph nodes.
The cervical esophagus is mobilized through a left-sided longitudinal neck incision along the sternocleidoid muscle. No formal cervical lymph node dissection is carried out, but cervical lymph nodes are dissected if lymph node metastases are suspected macroscopically during the cervical phase of esophagectomy. The esophagus is dissected and a cord is attached to the proximal part of the specimen to enable pull-up of the gastric conduit along the anatomical tract of the esophagus.
The esophagus and surrounding lymph nodes are pulled into the abdomen under laparoscopic vision. A 7-cm transverse incision is made at the level of the left paraumbilical port for extraction of the specimen and stomach using a wound protector.
Outside the abdomen, a 5-cm-wide gastric tube is constructed with staplers (GIA TM 80, 3 · 8 mm; Covidien, Dublin, Ireland), and the stapled line is oversewn with 3-0 polydioxanone. Routine extracorporal oversewing was reintroduced as two serious complications occurred when the staple line was not oversewn [14]. The specimen consisting of the esophagus and cardia of the stomach is sent for pathological examination. After the gastric tube has been pulled to the neck, a hand-sewn end-to-side esophagogastrostomy is performed in the neck using 3-0 polydioxanone single-layer running sutures. Excess gastric tubing is removed using a GIA stapler.
A feeding jejunostomy (Freka® FCJ-Set, Fresenius Kabi AG, Bad Homburg vd H., Germany) is placed at the level of the transverse incision.
Postoperative Care
Clinical Care
Postoperatively, patients are transferred to the intensive care unit (ICU). After leaving the operating room, mechanical ventilation is continued briefly usually extubating later that evening. After 1 day in the ICU, patients are transferred to a medium care (MC) ward.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree