Fig. 12.1
Comparison of the RAT and RFT approaches. Dashed and dotted lines show the extent of dissection for each procedure. A robotic axillary thyroidectomy (RAT), B robotic facelift thyroidectomy (RFT) (From Duke and Terris [22] © 2013 Georgia Regents University)
12.1.1 RAT Technique
The remote access robotic axillary thyroidectomy procedure has been extensively described [1, 2, 8, 9] and though it has undergone some modifications since its initial description, a generalized overview of the technique is presented here. The patient is placed supine on the operating table and the ipsilateral arm is extended at the shoulder and secured to an armrest. Flexing the elbow may minimize the risk of brachial plexus or ulnar nerve injury [2]. A 5–6 cm vertical incision is marked in the anterior axilla. A second 1 cm working port may be created on the patient’s chest 2 cm above the nipple line and 2 cm off the midline, though many surgeons now omit this extra incision and introduce all the instruments through the axilla.
The axillary incision is continued down to the fascia overlying the pectoralis major muscle. Dissection proceeds across the pectoralis major to the midline and superiorly above the clavicle. The sternocleidomastoid muscle (SCM) is identified and the space between the sternal and clavicular heads of the SCM is developed. The sternal head is retracted ventrally to expose the strap muscles, avoiding injury to the internal jugular vein or its tributaries. The strap muscles are elevated off the thyroid gland from the sternal notch to the superior pole and across the midline, dividing the omohyoid muscle if necessary to improve access. The surgical field is maintained with a fixed retractor system.
The robot console is then introduced on the opposite side of the operating table. A 30° downward facing camera is inserted through the axillary incision. Harmonic shears (Ethicon Endosurgery Inc., Cincinnati, OH) are placed in the dominant arm, and ProGrasp forceps (Intuitive Surgical, Sunnyvale, CA) and a Maryland grasper are placed in the nondominant arms.
Using robotic assistance, the gland is retracted inferiorly, and the superior vascular pedicle is transected with the Harmonic device. Soft tissue attachments and vessels along the lateral and inferior aspect of the gland are divided and the gland is rotated medially. The recurrent laryngeal nerve (RLN) and parathyroid glands are identified and preserved. The isthmus and ligament of Berry are divided and the lobe is removed. Removal of the contralateral lobe through the same incision may be accomplished in select cases by performing a subcapsular dissection between the thyroid and the trachea to identify the contralateral RLN and remove the gland. A surgical drain is placed prior to wound closure, and patients are generally admitted for inpatient observation.
12.1.2 RFT Technique
The remote access robotic facelift thyroidectomy procedure has also been described in detail [10, 11]. A transverse anterior cervical incision is marked in a natural neck crease while the patient is sitting in an upright neutral position in the preoperative holding area in the unlikely event that conversion to an open procedure is necessary. The patient is positioned just off-center of the operating table toward the side to be operated on, with the top of the patient’s head level with the top of the operating table.
A propofol infusion is used to maintain general anesthesia, allowing rapid titration of the anesthetic depth. A short-acting muscle relaxant may be used to facilitate intubation, but no paralytics should be used during the dissection. The patient is intubated with an EMG endotracheal tube (ETT) to permit intraoperative laryngeal nerve monitoring. GlideScope (Verathon Inc, Bothell, WA) visualization is useful during intubation so that proper positioning of the EMG electrodes can be confirmed by the surgeon. A straight extension attached to the anesthesia circuit limits tension on the tubing, and a 3-way stop-cock valve connected to the CO2 return tubing prevents kinking of this tube. The patient’s arms are tucked at their sides and secured with wide silk tape. No safety straps are attached to the table above the patient’s waist because they interfere with placement of the retractors. The bed is rotated 180° and patient’s head is turned 20–30° towards the contralateral side, with the face supported by soft towels. Taping the anesthesia circuit to the operating table prevents any excessive tension which might cause the endotracheal tube to twist or migrate.
The occipital hairline is shaved back 1 cm and the facelift incision is marked. The incision begins in the postauricular crease near the inferior extent of the earlobe. It continues superiorly and then posteriorly into the shaved region of the occipital hairline in a gentle curve behind the auricle (Fig. 12.2). This placement ensures the incision will be completely concealed once the hair grows back. The incision is continued as far posteriorly and inferiorly as necessary to ensure adequate exposure.
A subplatysmal flap is developed and continued until the SCM is identified. A series of landmarks are then encountered as dissection continues anteriorly and inferiorly along the SCM. The great auricular nerve (GAN) is identified first, followed by the external jugular vein and the anterior border of the SCM. The external jugular vein is generally preserved, though it may be divided if necessary to improve exposure. Dissection continues along the anteromedial border of the SCM to the clavicle. Visualization during the deeper portions of the dissection is facilitated by placing the operating table in reverse Trendelenburg and rotating it away from the surgeon.
The omohyoid is identified, and a muscular triangle bounded by the anterior border of the SCM, the superior border of the omohyoid and the posterior border of the sternohyoid is defined. The strap muscles are retracted ventrally to expose the superior pole of the thyroid gland and the superior vascular pedicle is isolated. To limit the amount of robotic manipulation required, the lobe is mobilized as much as possible at this time. A modified Chung retractor (Marina Medical, Sunrise, FL) is fixed to the contralateral side of the table to retract the strap muscles ventrally. A Singer hook (Medtronic, Jacksonville FL) attached to a Greenberg retractor (Codman & Shurtleff, Inc., Raynham, MA) is secured to the ipsilateral side of the table and used to retract the SCM.
The robotic console is then positioned near the opposite side of the operating table, with the pedestal angled 30° away from the table. Fine positioning adjustments are more easily accomplished by moving the table rather than by moving the robot console. The camera arm with a 30° down facing endoscope is positioned along the long axis of the modified Chung retractor. The camera arm is nearly fully extended so the hinges of the camera arm will not collide with the other arms. A Harmonic device is placed in the dominant arm and a Maryland grasper is used in the nondominant arm.
The robotic portion of the procedure begins by dividing the superior vascular pedicle with the Harmonic device. The superior thyroid pole is retracted inferiorly and ventrally, exposing the inferior constrictor muscle and preserving the superior laryngeal nerve. The superior parathyroid gland is identified on the posterior aspect of the thyroid and preserved. The RLN is then identified laterally as it courses under the inferior constrictor (Fig. 12.3). Tracing the nerve inferiorly exposes the ligament of Berry. The middle thyroid vein is divided. With the nerve under direct visualization, the ligament is transected with the Harmonic device and the thyroid isthmus is divided. The inferior parathyroid gland is preserved, and the inferior vessels are transected with the Harmonic device. Any remaining soft tissue attachments to the thyroid are divided and the specimen is removed.
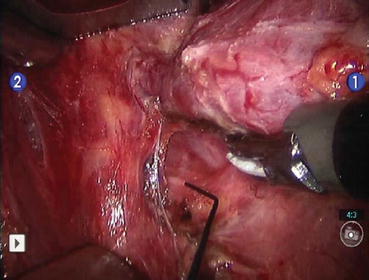
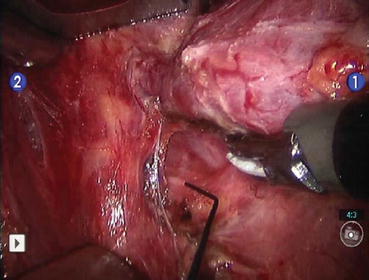
Fig. 12.3
The recurrent laryngeal nerve is identified and electrically stimulated during the robotic facelift thyroidectomy (From Terris et al. [10])
The robotic cart is removed. The surgical field is irrigated and Surgicel (Ethicon, Inc., Somerville, NJ) is placed into the thyroid bed. The incision is approximated using buried interrupted deep dermal 4-0 Vicryl sutures (Ethicon, Inc., Somerville, NJ). The skin edges are sealed with tissue adhesive and ¼ inch Steri-Strips (3M Corporation, St. Paul, MN) placed horizontally along the incision. No drains are utilized. Deep extubation is recommended to minimize coughing or straining on emergence from anesthesia.
12.2 Indications for Remote Access Robotic Thyroid Surgery
Patients interested in remote access robotic assisted thyroid surgery place a high premium on cosmetic outcomes. Either for personal or professional reasons, they are highly motivated to avoid a visible neck scar, and they must be willing to accept the potential disadvantages of these procedures, such as a longer operative time, a prolonged recovery course, and procedure-specific risks not generally associated with other types of thyroid surgery. Candidates should be counseled that these procedures are not minimally invasive and are not “scarless.” The scars associated with these procedures are usually longer than those of anterior cervical approaches; they are just concealed in remote locations. Finally, patients must be willing to accept the unlikely but possible chance that conversion to an anterior approach may be required.
12.2.1 RAT Patient Selection
There is no uniform set of selection criteria for the RAT [2, 5]. The procedure was initially described in patients with benign nodules ≤5 cm and malignant lesions ≤2 cm [1, 8]. Early exclusion criteria included prior neck surgery, “severe” Graves’ disease, extrathyroidal extension of malignant disease, multiple lateral neck nodal metastases, nodal extracapsular spread or lesions in the dorsal aspect of the thyroid [8]. Patients with substernal or retropharyngeal extension have also been excluded [4].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree