4 Risk Factors and Risk Assessment
Breast Cancer and Risk
Breast cancer is the most common non–skin cancer and is second only to lung cancer as a leading cause of cancer death in women. An estimated 192,370 women were diagnosed with invasive breast cancer, and an estimated 41,170 women died of this disease in 2009.1
As a result of increased longevity, the incidence of breast cancer has been growing since the 1980s.2 In the 1970s, a woman’s lifetime risk of being diagnosed with breast cancer in the United States was just under 10% (1 in 10). Since then, the estimated lifetime risk increased gradually until the beginning of the new millennium, when a slight decrease occurred. One in eight girls (or 12.5%) born in the United States today will be diagnosed with breast cancer at some time in their lives.3
Individual differences in age, family history, reproductive history, race or ethnicity, and other factors can dramatically reduce or increase a woman’s risk of breast cancer.3 Individual evaluation and assessment can help practitioners and patients determine individual risk and plan the proper course of action for follow-up.
What Is Risk?
A risk factor is anything that increases the probability of the development of a disease process.4 In evaluating clinical management strategies, individual risk assessment is more useful for patients than data on the overall population risk.5 An individual’s risk can be expressed in a number of ways: lifetime risk, 5-year risk, absolute risk, and relative risk. Risk assessment can be determined by means of a variety of valid and reliable tools, which are discussed in detail later in this chapter.
Like all medical decisions, the potential benefits of a course of treatment or more intensive screening should be balanced against the risks and costs. Many women have one or more risk factors for breast cancer but do not develop the disease. Most women with breast cancer have no apparent risk factors other than gender and age. Also, most women who have a risk factor and develop breast cancer cannot actually confirm that the risk factor contributed to their diagnosis. Risk factors should not be seen as predictive of breast cancer, and similarly the absence of risk factors should not lead to complacency. Risk assessments can be a guide to help women and their health care providers make informed decisions about the need for earlier, more intensive, or more frequent screenings, genetic counseling, or even prophylactic treatments.
Risk Factors
Table 4-1 shows the relative risk of many modifiable and nonmodifiable risk factors. Nonmodifiable factors tend to have the greater relative risk (1.1 to 10 times greater risk, excluding “being female” as a risk factor) than modifiable factors (1.1 to 4.0 times greater risk).6 However, since most women with breast cancer have no identifiable risk factors other than gender and age, it behooves women and their physicians to reduce risk wherever possible by addressing lifestyle changes such as losing weight and increasing exercise. See Chapter 7 for an in-depth discussion of lifestyle changes that may reduce risk.
Table 4-1 Modifiable versus Nonmodifiable Risks
| Risk Factor | Approximate Relative Risk |
|---|---|
| Modifiable Risk Factors (Range 1.1–4 times greater risk) | |
| Radiation exposure or frequent x-rays during youth | 2.0–4.0 |
| Fist child after age 30 | 1.4–2.0 |
| Not having children (vs women who give birth at age 35 or younger) | 1.5–2.0 |
| Postmenopausal hormone use, estrogen plus progestin (current or recent use for 5 or more years) | 1.3–2.0 |
| Overweight/weight gain | 1.2–1.5 |
| Drinking alcohol (2–4 drinks/day) | 1.4 |
| Current or recent use of birth control pills | 1.1–1.3 |
| Lack of exercise | 1.2 |
| Not breastfeeding | 1.1–1.2 |
| Nonmodifiable Risk Factors (Range 1.1–99 times greater risk) | |
| Female (vs male) | 99.0 |
| Carcinoma in situ (lobular) | 7.0–10.0 |
| Confirmed genetic mutations (BRCA1 or BRCA2) | 6.0–10.0 |
| Age (risk over age 50 vs risk up to age 50)* | 6.0 |
| Family history of breast cancer (2 immediate family members affected) | 4.0–6.0 |
| High breast density | 3.0–6.0 |
| Personal history of breast cancer | 2.0–6.0 |
| Benign breast disease (proliferative): atypical hyperplasia | 4.0 |
| High bone density | 1.5–3.5 |
| Family history of breast cancer (mother affected before age 60) | 2.0–3.0 |
| High levels of estrogen in the blood after menopause | 2.0 |
| Menopause at age 55 or older | 2.0 |
| Benign breast disease (proliferative): usual hyperplasia | 1.5–1.9 |
| High socioeconomic status | 1.2–1.8 |
| Family history of breast cancer (mother affected after age 60) | 1.4 |
| First period before age 12 | 1.2–1.3 |
| Being tall | 1.2 |
| Ashkenazi Jewish heritage | 1.1 |
Based on Susan G. Komen for the Cure website: Risk Factors and Prevention, Summary Table of Relative Risks. cms.komen.org/komen/AboutBreastCancer/RiskFactorsPrevention/index.htm.
Gender
The number one risk factor for breast cancer is gender. Less than 1% of all breast cancers are found in men, although the incidence among men has increased 60% since 1990.7 The mean age at diagnosis for men is 60 to 70 years. Survival rates for men are more or less the same as for women, although recent studies have found that African-American men have a lower survival rate.8 A family history of male breast cancer is indicative of a possible genetic mutation, and high-risk screening should be considered for others in the family.9
Age
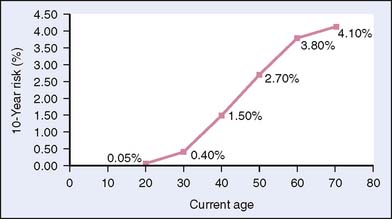
Age is a common risk factor for all women. As a woman gets older, she has a greater risk of developing breast cancer (Fig. 4-1). In the United States, 95% of the women diagnosed with breast cancer each year are age 40 or older.10 A woman today faces a one in eight chance of being diagnosed with breast cancer in her lifetime, and half of that risk is incurred after age 60.5 From 2005 to 2006, the median age at diagnosis for cancer of the breast was 61.1 Because rates of breast cancer rise with age, estimates of risk at specific ages are more meaningful as a clinical tool than estimates of lifetime risk.3 Table 4-2 shows the probability of a woman developing breast cancer by age group.10
Table 4-2 Age-Specific Probabilities of Developing Invasive Female Breast Cancer*
| If Current Age Is: | The Probability of Developing Breast Cancer in the Next 10 Years Is:† | Or 1 in: |
|---|---|---|
| 20 | 0.06% | 1760 |
| 30 | 0.44% | 229 |
| 40 | 1.44% | 69 |
| 50 | 2.39% | 42 |
| 60 | 3.40% | 29 |
| 70 | 3.73% | 27 |
| Lifetime risk | 12.08% | 8 |
* Among those free of cancer at beginning of age interval. Based on cases diagnosed 2004–2006. Percentages and “1 in” numbers may not be numerically equivalent due to rounding.
† Probability derived using NCI DevCan Software, Version 6.4.0. From American Cancer Society, Breast Cancer Facts & Figures 2009–2010. Atlanta: American Cancer Society, Inc., Table 5.
Worldwide, this pattern of late-life or postmenopausal breast cancer is associated with more developed economies or Westernized societies. Premenopausal breast cancer rates are similar throughout the world, suggesting that the disease mechanisms for premenopausal breast cancer are the same worldwide. However, because developed countries see much higher rates of postmenopausal breast cancer,10 the disease mechanism is thought to be secondary to lifestyle decisions. Within one or two generations, women who move from an undeveloped country to a more developed country exhibit breast cancer rates similar to those of their adopted country, which suggests environmental influences.10
Inherited Risk Factors
Family history and genetics affect a woman’s risk for breast cancer. Overall, only 5% to 10% of breast cancers are thought to be due to an inherited trait. Women up to age 70 who are BRCA1 or BRCA2 mutation carriers have a cumulative risk of 46% and 43%, respectively.11
Our understanding of the genetic link to breast cancer and our ability to test for genetic causes is incomplete. Many families have evidence of a genetic risk factor, but no specific mutated gene can be identified. It is important for the health care provider to take a detailed multigenerational family history to identify families with potential genetic risk for breast cancer.12
Family History
Because of the high incidence of breast cancer in the general population, it is not uncommon for a woman to report a history of breast cancer in her family. Fully 50% of women diagnosed with breast cancer report a relative of any degree with breast cancer.2 Yet BRCA1 and BRCA2 genes are present in less than 10% of women with breast cancer.2
A woman with a first-degree relative with breast cancer has a two to three times greater risk for the disease than a woman with no family history. For women with more than one immediate female family member with breast cancer, the lifetime excess incidence of disease is 13.3%.14
Breast cancer in a close male relative (father, brother, uncle) is rare but should be regarded as a significant risk factor. The paternal family history should also be included in any assessment, since genetic mutations may pass from the father’s side without resulting in a male breast cancer (see Chapter 5). A history of prostate cancer may also be an indicator of increased risk or a genetic cause, especially when prostate cancer was found at an early age.14
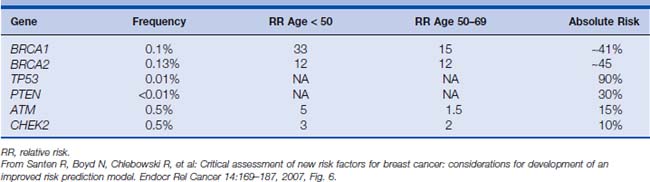
Table 4-3 shows the genes that have been identified as playing a role in breast cancer, along with the frequency of the mutation in the general population, the relative risk both under age 50 and for the decade following age 50, and the absolute lifetime risk. Genetic counseling is important for a woman with a strong family history of breast cancer or related cancers so that she and her family can understand what genetic testing means and, more important, what it doesn’t mean.
Race and Ethnicity
The incidence of breast cancer in the United States varies by race, as shown in Table 4-4. White women have the highest incidence, followed by African-American women, with an 11% lower incidence. Women of Hispanic or Asian/Pacific Island heritage have an incidence of breast cancer around 33% lower than that of white women.1
Table 4-4 Breast Cancer Incidence Rates by Race (U.S. 2002–2006)
| Race/Ethnicity | Female |
|---|---|
| All races | 123.8 per 100,000 women |
| White | 127.8 per 100,000 women |
| Black | 117.7 per 100,000 women |
| Asian/Pacific Islander | 89.5 per 100,000 women |
| American Indian/Alaska Native* | 74.4 per 100,000 women |
| Hispanic† | 88.3 per 100,000 women |
* Rates are age-adjusted to the 2000 standard population.
† Persons of Hispanic origin may be any race. Data from SEER Stat Fact Sheets: Cancer of the Breast. http://seer.cancer.gov/statfacts/html/breast.html
The causes of these differences are not well understood, although differences in genetics, lifestyle, and access to health care all are likely to play a role. Women born in Asia, for example, have a low risk of developing breast cancer, but their daughters and relatives who are born in North America have a risk profile similar to that of white American women. This seems to indicate that environmental or lifestyle factors are at play. African-American women under age 50 have a higher age-specific incidence of breast cancer than that of white women,1 and the stage at diagnosis for all African Americans is often more advanced than that for white women. This points to differences in genetics that put African-American women at slightly greater risk for premenopausal breast cancer.
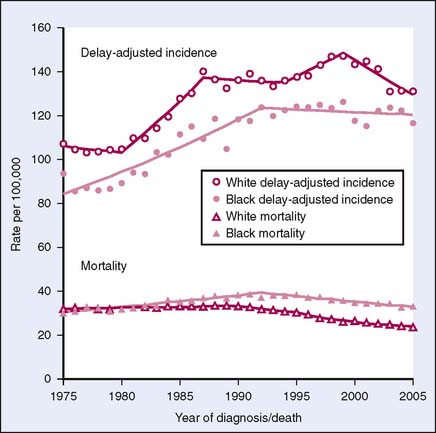
The mortality of breast cancer also differs among different races. As Figure 4-2 demonstrates, African-American women have a lower incidence of breast cancer than white women, but the mortality of breast cancer is greater among African-American women. Incidence and mortality rates have been declining for both races since 2000. Current 5-year relative survival rates by race are 89.4% for white women and 85.4% for black women.1 This decline followed the decrease in use of exogenous hormones in postmenopausal women. Factors associated with improved survival may include increased screening leading to early detection and improved screening technologies.
Behavioral Factors
For women concerned about breast cancer, some lifestyle changes may lead to reduced risk. For a more in-depth analysis of these lifestyle risk factors, see Chapter 7.
Weight
Postmenopausal women who have gained 25.0 kg or more since age 18 have an increased risk of developing breast cancer.15 Adipose tissue stores endogenous hormones; therefore, excess weight may be a modifiable risk factor. Before menopause, being slightly overweight decreases a woman’s risk of breast cancer. After menopause, however, being overweight increases risk by 30% to 60%.16 Increased body fat during childhood and adolescence is associated with reduced incidence of premenopausal breast cancer, independent of adult body mass index and menstrual cycle characteristics.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree