Risk: Basic Principles
The lesson … is that a large number of people at a small risk may give rise to more cases of disease than the small number who are at a high risk.
—Geoffrey Rose 1985
KEY WORDS
Risk
Risk factor
Exposure
Latency period
Immediate causes
Distant causes
Marker
Risk prediction model
Risk prediction tool
Risk stratification
Calibration
Discrimination
Concordance statistic
C-statistic
Sensitivity
Specificity
Receiver operating characteristic (ROC) curve
Risk generally refers to the probability of some untoward event. In medicine, clinicians deal with probabilities in virtually every patient encounter. They work with basic principles of risk whether they are diagnosing a complaint, describing prognosis, deciding on treatment, or discussing prevention with the patient. Patient encounters no longer deal only with the patient’s complaints, but increasingly involve checking for risk factors that might lead to poor health in the future. In medical research, more and more effort is devoted to elucidating risk factors for diseases. A major rationale for the Human Genome Project is to predict diseases that will become manifest over a person’s lifetime. Clinical journals publish epidemiologic studies investigating possible health risks. All this effort has improved our understanding about risks to health and how to study them, and has helped improve the health of patients and populations, sometimes in dramatic ways. For example, research that led to the understanding that smoking, hypertension, and hyperlipidemia increase the risk of cardiovascular disease (CVD) has helped decrease cardiovascular mortality in the United States by half over the past several decades.
People have a strong interest in their risk of disease, a concern reflected in television and newspaper headlines, and the many Web sites and popular books about risk reduction. The risk of breast and prostate cancer, heart disease and stroke, Alzheimer disease, autism, and osteoporosis are examples of topics in which the public has developed a strong interest. Discerning patients want to know their individual risks and how to reduce them.
In this chapter, we will concentrate on the underlying principles about risk, important regardless of where risk confronts the clinician and patient along the spectrum of care. As much as possible, we will deal with concepts rather than terminology and methods, covering those important details in later chapters. Chapters 5 and 6 deal with risks for adverse health effects in the distant future, often years or even decades away; they describe scientific methods used to indicate the probability that people who are exposed to certain “risk factors” will subsequently develop a particular disease or bad health outcome more often than similar people who are not exposed. In acute care settings such as intensive care units, emergency rooms, and hospital wards, the concern is about risks patients with known disease might or might not experience, termed prognosis (Chapter 7); the time horizon of prognosis spans from minutes and hours to months and years, depending on the study. Chapters 8, 9, and 10 revisit risk as it relates to diagnosis, treatment, and prevention. In each case, the approach to assessing risk is somewhat different. However, the fundamental principles of determining risks to health are similar.
RISK FACTORS
Characteristics associated with an increased risk of becoming diseased are called risk factors. Some risk factors are inherited. For example, having the haplotype HLA-B27 greatly increases one’s risk of acquiring the spondyloarthropathies. Work on the Human Genome Project has identified many other diseases for which specific genes are risk factors, including colon and breast cancer, osteoporosis, and amyotrophic lateral sclerosis. Other risk factors, such as infectious agents, drugs, and toxins, are found in the physical environment. Still others are part of the social environment. For example, bereavement after the loss of a spouse, change in daily routines, and crowding all have been shown to increase rates of disease—not only for emotional illness but physical illness as well. Some of the most powerful risk factors are behavioral; examples include smoking, drinking alcohol to excess, driving without seat belts, engaging in unsafe sex, eating too much, and exercising too little.
Exposure to a risk factor means that a person, before becoming ill, has come in contact with or has manifested the factor in question. Exposure can take place at a single point in time, as when a community is exposed to radiation during a nuclear accident. More often, however, contact with risk factors for chronic disease takes place over a period of time. Cigarette smoking, hypertension, sexual promiscuity, and sun exposure are examples of risk factors, with the risk of disease being more likely to occur with prolonged exposure.
There are several different ways of characterizing the amount of exposure or contact with a putative risk factor: ever been exposed, current dose, largest dose taken, total cumulative dose, years of exposure, years since first exposure, and so on. Although the various measures of dose tend to be related to one another, some may show an exposure-disease relationship, whereas others may not. For example, cumulative doses of sun exposure constitute a risk factor for non-melanoma skin cancer, whereas episodes of severe sunburn are a better predictor of melanoma. If the correct measure is not chosen, an association between a risk factor and disease may not be evident. Choice of an appropriate measure of exposure to a risk factor is usually based on all that is known about the clinical and biologic effects of the exposure, the pathophysiology of the disease, and epidemiologic studies.
RECOGNIZING RISK
Risk factors associated with large effects that occur rapidly after exposure are easy for anyone to recognize. It is not difficult to appreciate the relationship between exposure and medical conditions such as sunburn and aspirin overdose, or the poor prognosis of hypotension at the onset of myocardial infarction, because the deleterious effect follows exposure relatively rapidly and is easy to see.
The sudden increase of a rare disease, or the dramatic clinical presentation of a new disease is also easy to recognize, and invites efforts to find a cause. AIDS was such an unusual syndrome that the appearance of just a few cases raised suspicion that some new agent (as it turned out, a retrovirus) might be responsible, a suspicion confirmed relatively quickly after the first cases of the disease. A previously unidentified coronavirus was confirmed as the cause of severe adult respiratory syndrome (SARS) in a matter of weeks after the first reported cases of the highly lethal infection in 2003. Similarly, decades ago, physicians quickly noticed when several cases of carcinoma of the vagina, a very rare condition, began appearing. A careful search for an explanation was undertaken, and maternal exposure to diethylstilbestrol (a hormone used to stabilize pregnancies in women with a history of miscarriage) was found.
Most morbidity or mortality, however, is caused by chronic diseases for which the relationship between exposure and disease is far less obvious. It is usually impossible for individual clinicians, however astute, to recognize risk factors for chronic disease based on their own experiences with patients. This is true for several reasons, which are discussed in the following pages.
Long Latency
Many chronic diseases have a long latency period between exposure to a risk factor and the first manifestations of disease. Radiation exposure in childhood, for example, increases the risk for thyroid cancer in adults decades later. Similarly, hypertension precedes heart disease by decades, and calcium intake in young and middle-aged women affects osteoporosis and fracture rates in old age. When patients experience the consequence of exposure to a risk factor years later, the original exposure may be all but forgotten and the link between exposure and disease obscured.
Immediate Versus Distant Causes
The search for risk factors usually is a search for causes of disease. In clinical medicine, physicians are more interested in immediate causes of disease— infectious, physiologic, or anatomic changes leading to sickness such as a coronavirus causing SARS or hypocalcemia leading to seizures. But distant causes,
more remote causes, may be important in the causal pathway. For example, lack of maternal education is a risk factor for low-birth-weight infants. Other factors related to education, such as poor nutrition, less prenatal care, cigarette smoking, and the like are more direct causes of low birth weight. Nevertheless, studies in India have shown that improving maternal education lowers infant mortality.
more remote causes, may be important in the causal pathway. For example, lack of maternal education is a risk factor for low-birth-weight infants. Other factors related to education, such as poor nutrition, less prenatal care, cigarette smoking, and the like are more direct causes of low birth weight. Nevertheless, studies in India have shown that improving maternal education lowers infant mortality.
Common Exposure to Risk Factors
Many risk factors, such as cigarette smoking or eating a diet high in sugar, salt, and fat, have become so common in Western societies that for many years their dangers went unrecognized. Only by comparing patterns of disease among people with and without these risk factors, using cross-national studies or investigating special subgroups—Mormons, for example, who do not smoke, or vegetarians who eat diets low in cholesterol—were risks recognized that were, in fact, large. It is now clear that about half of lifetime users of tobacco will die because of their habit; if current smoking patterns persist, it is predicted that in the 21st century, more than 1 billion deaths globally will be attributed to smoking (1).
A relationship between the sleeping position of babies and the occurrence of sudden infant death syndrome (SIDS) is another example of a common exposure to a risk factor and the dramatic effect associated with its frequency, an association that went unrecognized until relatively recently.
Example
SIDS, the sudden, unexplained death of an infant younger than 1 year of age, is a leading cause of infant mortality. Studies suggest that there are many contributing factors. In the late 1980s and 1990s, several investigations found that babies who were placed face down in their cribs were three to nine times more likely to die of SIDS than those placed on their backs. In 1992, the American Academy of Pediatrics issued a recommendation to place infants on their backs to sleep but indicated that side positioning for sleep was an acceptable alternative. The percentage of babies placed in the prone position for sleep fell from 70% in 1992 to 24% in 1996, with a concomitant 40% drop in the number of SIDS cases (2). Ongoing research led to evidence that side positioning of babies also increased the risk of SIDS (3), and the American Academy of Pediatrics updated its recommendations in 2005 to make it clear that side sleeping was no longer recommended.
Low Incidence of Disease
The incidence of most diseases, even ones thought to be “common,” is actually uncommon. Thus, although lung cancer is the most common cause of cancer deaths in Americans, and people who smoke are as much as 20 times more likely to develop lung cancer than those that do not smoke, the yearly incidence of lung cancer in people who have smoked heavily for 30 years, is 2 to 3 per 1,000. In the average physician’s practice, years may pass between new cases of lung cancer. It is difficult for the average clinician to draw conclusions about risks from such infrequent events.
Small Risk
The effects of many risk factors for chronic disease are small. To detect a small risk, a large number of people must be studied to observe a difference in disease rates between exposed and unexposed persons. For example, drinking alcohol has been known to increase the risk of breast cancer, but it was less clear whether low levels of consumption, such as drinking just one glass of wine or its equivalent a day, conferred risk. A study of 2,400,000 women-years was needed to find that women who averaged a glass a day increased their risk of developing breast cancer 15% (4). Because of the large numbers of woman-years in the study, chance is an unlikely explanation for the result, but even so, such a small effect could be due to bias. In contrast, it is not controversial that hepatitis B infection is a risk factor for hepatoma, because people with certain types of serologic evidence of hepatitis B infection are up to 60 times (not just 1.15 times) more likely to develop liver cancer than those without it.
Multiple Causes and Multiple Effects
There is usually not a close, one-to-one relationship between a risk factor and a particular disease.
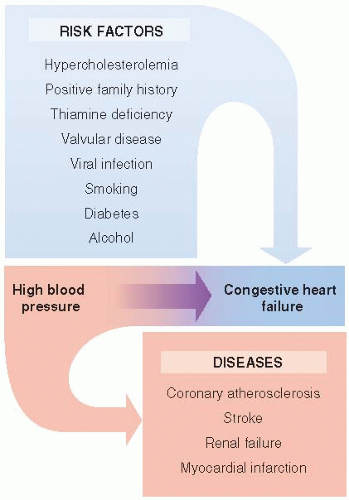
A given risk factor may contribute to many diseases, and a disease may have multiple causes. The relationship between hypertension and congestive failure is an example (Fig. 4.1). Some people with hypertension develop congestive heart failure, and many do not. Also, many people who do not have hypertension develop congestive heart failure because there are other causes. The relationship is also difficult to recognize because hypertension causes several diseases other than congestive heart failure. Thus, although hypertension is the third leading cause of congestive heart failure, physicians were not aware of this relationship until the 1970s, when adequate evidence became available after careful study of large numbers of people over many years.
A given risk factor may contribute to many diseases, and a disease may have multiple causes. The relationship between hypertension and congestive failure is an example (Fig. 4.1). Some people with hypertension develop congestive heart failure, and many do not. Also, many people who do not have hypertension develop congestive heart failure because there are other causes. The relationship is also difficult to recognize because hypertension causes several diseases other than congestive heart failure. Thus, although hypertension is the third leading cause of congestive heart failure, physicians were not aware of this relationship until the 1970s, when adequate evidence became available after careful study of large numbers of people over many years.
Risk Factors May or May Not Be Causal
Just because risk factors predict disease, it does not necessarily follow that they cause disease. A risk factor may predict a disease outcome indirectly, by virtue of an association with some other variable that actually is a determinant of disease. That is, the risk factor is confounded with a truly causal factor.
A risk factor that is not a cause of disease is called a marker of disease, because it “marks” the increased probability of disease. Not being a cause does not diminish the value of a risk factor as a way of predicting the probability of disease, but it does imply that removing the risk factor might not remove the excess risk associated with it.
Example
Homocystinuria, a rare pediatric disease caused by autosomal recessive genes and very high levels of the amino acid homocysteine, is associated with severe premature atherosclerosis. The possibility that slightly elevated homocysteine levels also could be a risk factor for coronary heart disease in adults has been investigated. Multiple studies have found that there is a relationship; each increase of 5 µmol/L in homocysteine level increases the risk of CVD by 20% (5). Because of this relationship, clinical studies were undertaken to determine if lowering homocysteine levels with folic acid as well as vitamins B6 and B12 would reduce the risk of major cardiovascular events among people with known CVD or diabetes. Surprisingly, several large studies found that even though homocysteine levels were lowered, the vitamin supplementation did not protect against future cardiovascular events in these patients (6). Thus, although elevated homocysteine levels was a marker for future CVD in adults, it does not appear to be a causal factor, at least among patients with known CVD or diabetes.
There are several ways of deciding whether a risk factor is a cause or merely a marker for disease. These are covered in Chapter 5.
For all these reasons, individual clinicians are rarely in a position to recognize, let alone confirm, associations between exposure and chronic diseases. They may notice an association when a dramatic
disease occurs quickly after an unusual exposure, but most diseases and most exposures do not conform to such a pattern. For accurate information about risk, clinicians must turn to the medical literature, particularly to carefully constructed studies that involve a large number of patients.
disease occurs quickly after an unusual exposure, but most diseases and most exposures do not conform to such a pattern. For accurate information about risk, clinicians must turn to the medical literature, particularly to carefully constructed studies that involve a large number of patients.
PREDICTING RISK
A single powerful risk factor, as in the case of hepatitis B and hepatocellular cancer, can be very helpful clinically, but most risk factors are not strong. If drinking a glass of wine a day increases the risk of breast cancer by 15%, and the average 10-year risk of developing breast cancer for women in their 40s is 1 in 69 (or 1.45%), having a glass of wine with dinner would increase the 10-year risk to about 1 in 60 (or 1.67%). Some women might not think such a difference in the risk of breast cancer is meaningful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree