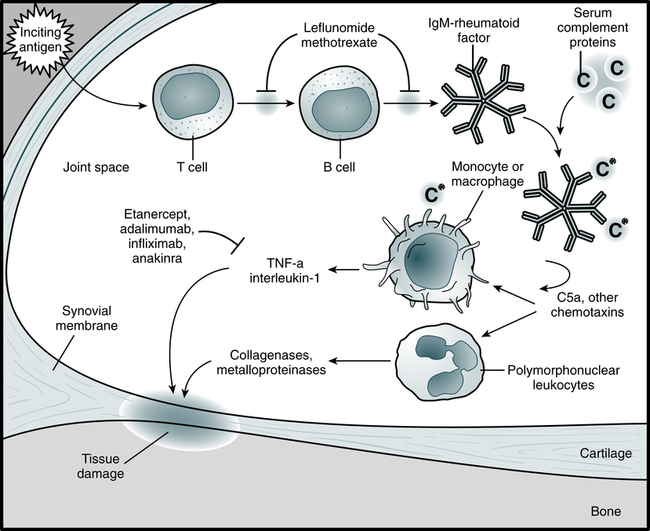
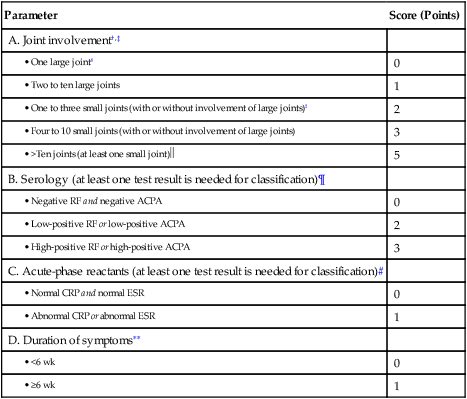
At the conclusion of this chapter, the reader should be able to: • Name significant factors related to the development of arthritis. • Describe the etiology, epidemiology, and signs and symptoms of rheumatoid arthritis. • Discuss the immunologic manifestations and diagnostic evaluation of rheumatoid arthritis. • Briefly describe juvenile rheumatoid arthritis. • Explain diagnostic procedures used in the identification and evaluation of rheumatoid arthritis. • Analyze representative rheumatoid arthritis case studies. • Correctly answer case study related multiple choice questions. • Be prepared to participate in a discussion of critical thinking questions. • Describe the principle, sources of error, clinical applications, and limitations of a rapid rheumatoid factor procedure. • 49.9 million (22.2%) of adults aged 18 years or older have self-reported physician-diagnosed arthritis. Rheumatoid arthritis is a chronic, multisystemic, autoimmune disorder and a progressive inflammatory disorder of the joints (Fig. 30-1). It is, however, a highly variable disease that ranges from a mild illness of brief duration to a progressive destructive polyarthritis associated with a systemic vasculitis (Fig 30-2).The pathogenesis of RA has the following three distinct stages: 1. Initiation of synovitis by the primary causative factor 2. Subsequent immunologic events that perpetuate the initial inflammatory reaction 3. Transition of an inflammatory reaction in the synovium to a proliferative, destructive tissue process Rheumatoid arthritis often begins with prodromal symptoms such as fatigue, anorexia, weakness, and generalized aching and stiffness not localized to articular structures. Joint symptoms usually appear gradually over weeks to months. The patient may display a wide variety of extra-articular manifestations (Box 30-1). The revised American Rheumatism Association’s criteria for diagnosis of RA are presented in Table 30-1. If these conditions are present for at least 6 weeks, the patient is designated as having classic RA. Prognostic markers such as a persistently high number of swollen joints, high serum levels of acute-phase reactants of immunoglobulin M (IgM) rheumatoid factor, early radiographic and functional abnormalities, and the presence of certain HLA class II alleles may help identify patients with more severe RA who are still in the early stages of the disease. Table 30-1 2010 ACR-EULAR Classification Criteria For Rheumatoid Arthritis∗ Adapted from American College of Rheumatology: The 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis, 2011 (http://www.rheumatology.org/practice/clinical/classification/ra/ra_2010.asp). ∗The criteria are aimed at the classification of newly presenting patients. In addition, patients with erosive disease typical of RA with a history compatible with prior fulfillment of the 2010 criteria should be classified as having RA. Patients with long-standing disease, including those whose disease is inactive (with or without treatment) who, based on retrospectively available data, have previously fulfilled the 2010 criteria should be classified as having RA. †Joint involvement refers to any swollen or tender joint on examination, which may be confirmed by imaging evidence of synovitis. Distal interphalangeal joints, first carpometacarpal joints, and first metatarsophalangeal joints are excluded from assessment. Categories of joint distribution are classified according to the location and number of involved joints, with placement into the highest category possible based on the pattern of joint involvement. ‡”Small joints” refers to the metacarpophalangeal joints, proximal interphalangeal joints, second through fifth metatarsophalangeal joints, thumb interphalangeal joints, and wrists. §“Large joints” refers to shoulders, elbows, hips, knees, and ankles. ¶Negative refers to IU values that are ≤ to the upper limit of normal (ULN) for the laboratory and assay; low-positive refers to IU values that are higher than the ULN but ≤3 times the ULN for the laboratory and assay; high-positive refers to IU values that are >3 times the ULN for the laboratory and assay. If RF information is only available as positive or negative, a positive result should be scored as low-positive for RF. #Normal/abnormal is determined by local laboratory standards. ∗∗Duration of symptoms refers to patient self-report of the duration of signs or symptoms of synovitis (e.g., pain, swelling, tenderness) of joints that are clinically involved at the time of assessment, regardless of treatment status.
Rheumatoid Arthritis
Signs and Symptoms

Shown are swan-neck deformity, ulnar deviation, dorsal interosseous atrophy, and swelling of wrist. (From Kaye D, Rose LF: Fundamentals of internal medicine, St Louis, 1983, Mosby.)
Parameter
Score (Points)
A. Joint involvement†,‡
0
1
2
3
5
B. Serology (at least one test result is needed for classification)¶
0
2
3
C. Acute-phase reactants (at least one test result is needed for classification)#
0
1
D. Duration of symptoms∗∗
0
1
 In this category, at least one of the involved joints must be a small joint; the others can include any combination of large and additional small joints, as well as other joints not specifically listed elsewhere (e.g., temporomandibular, acromioclavicular, sternoclavicular).
In this category, at least one of the involved joints must be a small joint; the others can include any combination of large and additional small joints, as well as other joints not specifically listed elsewhere (e.g., temporomandibular, acromioclavicular, sternoclavicular).
Oncohema Key
Fastest Oncology & Hematology Insight Engine






