Highlights
- •
Partial cystectomy serves as a less invasive alternative for muscle-invasive bladder cancer.
- •
The 5-year Overall Survival rate was 55%, Cancer Specific Survival was 67%, and Recurrence-Free Survival was 51%.
- •
Advanced T-stages, positive margins, vascular invasion, and lymphovascular invasion are linked to decreased survival.
- •
Major complication rates within 90 days postsurgery include Clavien-Dindo grade III at 4% and grade IV at 4%.
Abstract
Objectives
Partial cystectomy (PC) has been proposed as a less invasive alternative to radical cystectomy (RC) for the treatment of localized muscle-invasive bladder cancer (MIBC). The aim of this study was to evaluate the outcome of PC in a contemporary patient cohort to identify potential risk factors for this procedure.
Methods
Data from 58 MIBC patients who underwent PC were retrospectively analyzed. Demographics, tumor characteristics, clinical outcomes, and pathology results were collected. Statistical analysis was performed using Cox regression and Kaplan-Meier method to determine survival rates and risk factors.
Results
The cohort consisted of 58 patients with MIBC with a median age of 71 years. The 5-year overall survival (OS), cancer specific survival (CSS) and recurrence-free survival (RFS) rates were 55%, 67% and 51%, respectively. Clinical suspicion for lymph node metastases (HR 3.82, CI 1.09–13.39, P = 0.036), advanced T-stages (HR 3.80, CI 1.38 – 10.49, P = 0.010), a higher grading (HR 6.57, CI 0.76 – 49.19, P = 0.010), positive resection margins (HR 1.81, CI 1.10 – 2.96, P = 0.012), lymphovascular invasion (HR 5.14, CI 1.77 – 14.88, P = 0.003), vascular invasion (HR 6.62, CI 2.16 – 20.27, P = 0. 001), and longer time from initial diagnosis to surgery (HR 1.003, CI 1.001 – 1.01, days, P = 0.010) were associated with decreased OS. Complications within the first 30 and 90 postoperative days were observed in 31% and 36% of patients, respectively. 4% experienced a Clavien-Dino grade III/IV complication. One patient developed acute respiratory distress syndrome and died 46 days after surgery.
Conclusion
Partial cystectomy appears to be a safe bladder-sparing approach for highly selected MIBC patients with favorable oncologic outcomes and acceptable complication rates. Patient selection and assessment of tumor characteristics are essential for successful outcomes. Prospective randomized controlled trials are needed.
1
Introduction
Bladder cancer (BC) accounts for 3% of all malignant cancers and therefore is one of the most common malignancies globally [ ]. The gold standard of surgical treatment for patients with localized muscle-invasive bladder cancer (MIBC) and certain types of high-risk nonmuscle-invasive bladder cancer (NMIBC) is radical cystectomy (RC) with complete bladder removal and pelvic lymphadenectomy (PLND). However, RC often has a significant impact on patients’ quality of life either due to urinary diversion or because of side effects such as erectile dysfunction, leading to long-term functional and psychological distress [ ]. Furthermore, even in experienced centers, RC is considered one of the most complex urologic procedures with a high perioperative mortality and morbidity, with complication rates of up to 67% [ , ].
To mitigate these complications, partial cystectomy (PC) has been proposed as a less invasive alternative to RC for carefully selected patients. PC is a surgical approach, in which the tumor is selectively removed, including a surrounding safety margin, with the goal of maintaining oncologic control and preserving bladder function without need for urinary diversion. Therefore, it provides the potential to improve quality of life and reduce complication rates [ ]. Selecting the right candidate for PC is crucial for a good oncologic outcome [ ]. Early studies showed poor tumor control and high local recurrence rates of 40% to 78% [ ], but more recent series introduced stricter selection criteria with positive margins of 0% to 14% and local recurrence rates of 8% to 19% as a result [ , , ]. Despite the promising prospects of PC and its potential to provide a less invasive treatment option of localized MIBC, there is still a paucity of comprehensive literature with relatively small case numbers. In the present study, we conducted a retrospective analysis of the postoperative outcome after PC in patients diagnosed with localized MIBC to evaluate potential selection criteria.
2
Methods
2.1
Patient data and surgical technique
We retrospectively analyzed data of patients who underwent PC for localized BC at the Department of Urology, Charité, Berlin, Germany, between 2008 and 2018. After filtering out cases with NMIBC and unusual pathologies such as urachal tumors, ureteral and renal carcinomas, trophoblastic tumors, and persistent omphalomesenteric ducts, 58 out of 104 patients remained. The indication for PC has been largely based on the patient’s choice of bladder preservation. This was driven by several concerns, including the risk of impact on quality of life due to incontinence, the need for urinary diversion, erectile dysfunction, morbidity, and potential complications. In addition, PC was offered to patients with severe comorbidities making them ineligible for RC or to those who declined (chemo) radiotherapy. In contrast to other recent studies, our cohort did not adhere to additional strict inclusion criteria [ , , ]. Neoadjuvant chemotherapy was offered selectively based on individual patient factors, including comorbidities, general health and patient preference, often leading to deviations from guideline recommendations. We collected comprehensive patient data from medical records, including demographic data, tumor characteristics and location, intraoperative and postoperative clinical outcome parameters, pathology results of performed TURBTs, PCs, and tumor recurrence, information about neo-/adjuvant therapies, and radiological reports. Patients were also contacted by telephone to update overall survival (OS) data. Missing patient survival data were supplemented by inquiries to the clinical cancer registry of the Charité Comprehensive Cancer Center and the Berlin registry office to obtain possible information on patient deaths. The request was made on June 30, 2021. Follow-up was performed by calculating the time in months between the PC and the last contact with the patient or death.
Patient preparation and surgical technique (open PC with PLND) were described previously [ ].
2.2
Statistical analysis
Statistical analysis was performed using Microsoft Office Excel 2022, STATA Version SE 12.0 and IBM SPSS Statistics 17 software. OS, cancer-specific survival (CSS) and recurrence-free survival (RFS) were determined using the Kaplan-Meier method. Cox regressions were used to analyze the relationships between preoperative, intraoperative, and postoperative factors and OS, CSS or RFS. Statistical significance was assumed at P < 0.05.
3
Results
In this retrospective study, postoperative outcomes of 58 patients who underwent PC for MIBC were examined. The cohort consisted of 37 men and 21 women, with a median age of 71 years (IQR 63–79 years) and a median Body Mass Index (BMI) of 25 kg/m 2 . Median Charlson Comorbidity Index was 3 (IQR 1–5), indicating a high burden of comorbid conditions, and median ASA physical status was 2 (IQR 2–3). Prior abdominal surgery was described in 28 (48%) patients. The median follow-up period was 44 months. PC was conducted within 3 months after the initial TURBT in 89%. 94% of the patients presented with one solitary tumor, while the remaining cases involved 2 or 3 tumors. Urothelial carcinoma was the predominant histological type, accounting for 49 (84%) cases. The remaining cases displayed a squamous cell, adenocarcinoma or sarcomatoid differentiation. Neoadjuvant chemotherapy was administered in 6 cases (10%). Lymph node metastasis was clinically suspected in 8 cases (14%). In 88% of the PCs, intraoperative frozen section analysis was performed, with 95% confirming tumor-free margins and positive margins in 3 cases (5%). Overall, in the final pathologic examination, 12 specimens had positive resection margins. Furthermore, the histological examination revealed a median tumor size of 30 mm and a predominance of T3 cases (55%), followed by T2 (29%), and less frequently, T1, Ta, and T4 stages ( Table 1 ). The PC specimens showed pathologic upstaging in 44% of T2 tumors and down-staging in 7%, while no malignancy was detected in 24%. PLND was performed in 46 (79%) cases with a median number of 12 (2-33) removed lymph nodes. N1-stage was found in 9 (16%) patients, and N2-stage in another 9 (16%). Lymphovascular invasion was described in 43%, and vascular invasion in 16% ( Table 1 .). In 14 cases, there was no information available on the lymphovascular or vascular invasion. Data for grading according to the WHO 1973 classification was available in 56 cases, with 2 (3%) classified as Grade 1, 10 (18%) as Grade 2, and 44 (79%) as Grade 3.
| Characteristics | N (% or stated otherwise) |
|---|---|
| Epidemiologic characteristics Gender male/female (%) Median age (years) Median BMI (kg/m 2 ) Median Charlson Comorbidity Index Median ASA physical status classification Prior abdominal surgery Mean follow-up period (months) | 37/21 (64/36) 71 (IQR 63-79) 25 (IQR 23-28) 3 (IQR 1–5) 2 (IQR 2–3) 28 (48) 44 |
| Pathological tumor stage (UICC 2009) pTa pT1 pT2 a pT3 b pT4 c | 58 2 (3) 5 (9) 17 (29) 32 (55) 2 (3) |
| Tumor grading (WHO 1973) 1 2 3 | 56 2 (3) 10 (18) 44 (79) |
| Carcinoma in situ No Yes | 58 50 (86) 8 (14) |
| Regional lymph node status (N) pN0 pN1 pN2 pNX | 58 28 (48) 9 (16) 9 (16) 12 (21) |
| Surgical margins (R) R0 R1 RX | 58 36 (62) 12 (21) 10 (17) |
| Lymphovascular invasion (L) L0 L1 | 44 25 (57) 19 (43) |
| Vascular invasion (V) V0 V1 | 44 37 (84) 7 (16) |
a Of which T2a in 7 cases, T2b in 5 cases.
b Of which T3a in 18, T3b in 10 cases.
Complications within the first 30 and 90 postoperative days were observed in 31% and 36% of patients, respectively. Most complications were Clavien-Dindo grade I or II, but 2 patients (4%) experienced a Clavien-Dino grade III complication with one fascial dehiscence and one infected lymphocele [ ]. Urinary leakage occurred in 4 (7%) in the early postoperative period after Clavien Dindo (30 days). Most cases were larger tumors (46–50 mm) with localization on the side walls. All patients were treated conservatively with prolonged permanent catheterization. Within the first 90 days after surgery, leakage occurred in one further case, resulting in a total of 5 (9%) cases of urine leakage during this period. In this 1 case, the leakage occurred in the context of a urinary tract infection together with an infected lymphocele with urosepsis. In this case a consecutive surgical revision a prolonged transurethral catheterization was performed. Two patients (4%) had a Clavien-Dino grade IV complication. One patient developed acute respiratory distress syndrome and died 46 days after surgery ( Table 2 ).
| Complication | N (%) 30 d | N (%) 90 d |
|---|---|---|
| Postoperative bleeding events | 0 (0) | 0 (0) |
| Ileus | 0 (0) | 0 (0) |
| Hydronephrosis | 1 (2) | 2 (4) |
| Lymphocele without the need for therapy | 1 (2) | 2 (4) |
| Infected lymphocele | 0 (0) | 1 (2) |
| Fascial dehiscence | 1 (2) | 1 (2) |
| Urosepsis | 2 (4) | 3 (5) |
| Urinary leak | 4 (7) | 5 (9) |
| Urinary tract infection | 6 (10) | 10 (17) |
| Acute Respiratory Distress Syndrome | 0 (0) | 1 (2) |
| Clavien-Dindo grade | ||
| I | 5 (9) | 5 (9) |
| II | 8 (14) | 10 (17) |
| III | 2 (4) | 2 (4) |
| IV | 2 (4) | 2 (4) |
| V | 0 (0) | 1 (2) |
Data on adjuvant therapy was available for 28 (48%) cases. Among these, 10 (36%) patients received adjuvant chemotherapy, 3 (11%) received radio chemotherapy and one (4%) immunotherapy. Intravesical Bacillus Calmette-Guerin was administered in 12 (43%) patients and one (4%) patient received intravesical chemotherapy.
Local recurrence occurred in 23 (40%) patients, with tumor location within the PC resection area in 17 cases and 5 cases in another bladder area. In 1 case multilocular recurrence was described. RFS at the scar site was calculated at 59.8%, while the RFS at other bladder locations was 82.2%. The pathological outcomes of the cases with local recurrence showed superficial growth (pTa and pT1) in 9 cases (15.5%) and muscle-invasive growth ≥pT2 in 6 cases (10.3%). In 8 cases (13.8%) the pT stage was unknown. Subsequently, a total of 8 (14%) patients underwent salvage cystectomy with a median time-interval of 13.5 months. Of the 12 patients with positive resection margins, data on subsequent treatment were available in 9 cases. Of these patients, 3 (33%) received radiochemotherapy and 5 (55%) were treated with cisplatin-containing chemotherapy. One patient received immunotherapy with a checkpoint inhibitor. Four patients developed distant metastases and 1 patient had positive lymph nodes. In this group, 3 patients (33%) died at 6, 14 and 32 months after PC, respectively.
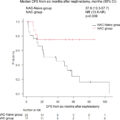
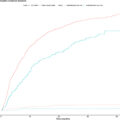
As shown in Fig. 2 The data revealed 1-year, 3-year, and 5-year OS rates of 92.8%, 68.7%, and 55.4%, respectively. Additionally, the 1-year, 3-year, and 5-year RFS rates were 79.6%, 64.6%, and 51%. The 1-year, 3-year and 5-year CSS rates were 94,8%, 79,1%, and 67.1%.
As shown in Table 3 , an increase in the time interval between the initial TURBT and PC (HR 1.003, CI 1.001–1.01, days, P = 0.01), as well as clinical suspicion for lymph node metastases (HR 3.82, CI 1.09–13.39, P = 0.036) was associated with reduced OS in univariate Cox regression analysis. Moreover, a significant risk for inferior OS for T3 and T4 tumors compared to lower T-stages (HR 3.80, CI 1.38–10.49, P = 0.01), as well as lymphovascular invasion (HR 5.14, CI 1.77–14.88, P = 0.003), vascular invasion (HR 6.62, CI 2.16–20.27, P = 0.001), a higher grading of G3 (HR 6.57, CI 0.76–49.19, P = 0.010) and positive resection margins (HR 1.81, CI 1.10–2.96, P = 0.012) was revealed ( Table 3 ). Multivariate regression revealed lymphovascular invasion (HR 4.14, CI 1.20–14.27, P = 0.024) and vascular invasion (HR 5.03, CI 1.19–21.21, P = 0.028) as risk factors for inferior OS ( Table 4 ). Additionally, Kaplan-Meier survival analysis and log-rank test ( Fig. 1 ) presented a reduced overall survival (OS) for a higher T-Stage (Ta–T2 vs T3–T4, P = 0.006), lymphovascular invasion (L0 vs L1, P = 0.001) and vascular invasion (V0 vs V1, P < 0.001). No statistically significant association with RFS was found for any of the variables. As shown in Suppl. Table 1 ., time interval between the initial TURBT and PC (HR 1.09, CI 1.02–1.15, days, P = 0.004), a higher T stage (HR 5.27, CI 1.15–15.73, P = 0.029), vascular invasion (HR 4.76, CI 1.19–19.07, P = 0.028), positive resection margins (HR 1.90, CI 1.05–3.46, P = 0.033), and length of hospital stay (HR 1.09, CI 1.02–1.19, days, P = 0.004) was associated with reduced CSS in univariate Cox regression analysis.