Abstract
Introduction
Stage III adrenocortical carcinoma encompasses both lymph node positive (TanyN1M0) and negative (T3-4N0M0) disease. Given the disease’s rarity, the current staging paradigm’s estimates of survival are supported by limited evidence. Consequently, we examined the impact of clinical lymph node positivity on survival outcomes in the context of the current staging of advanced adrenocortical carcinoma.
Methods
We identified patients with clinical stage III and IV disease from the National Cancer Database. Kaplan-Meier methods and Cox proportional hazards models estimated overall survival for stage III lymph node negative, stage III lymph node positive, and stage IV disease.
Results
We identified 917 patients with adrenocortical carcinoma – 322 (35.1%) stage III lymph node negative, 67 (7.3%) stage III lymph node positive, and 528 (57.6%) stage IV. 3-year overall survival for patients with stage III lymph node negative, stage III lymph node positive, and stage IV disease was 48.6%, 29.4%, and 15.6%, respectively. On univariable analysis, patients with stage III lymph node positive disease were associated with worse survival than those with stage III lymph node negative disease (HR 1.72, 95% CI 1.26-2.37, P < 0.001); however, this relationship did not maintain significance in multivariable analysis (HR 1.27, 95% CI 0.88-1.83, P = 0.21).
Conclusion
Our study finds that patients with clinical stage III lymph node positive adrenocortical carcinoma may have worse survival outcomes than stage III patients without lymph node involvement. The results of this study suggest the need for an updated, more nuanced staging paradigm, which differentiates stage III disease by lymph node positivity.
1
Introduction
Adrenocortical carcinoma is a rare malignancy, with only approximately 600 incident cases diagnosed annually in the United States [ ]. Patients often have nonspecific symptoms and roughly a quarter of patients may present with advanced disease [ ]. Given this, patients with stage III and IV disease have reported 5-year overall survival rates of 24-50% and 0-17%, respectively [ ].
The American Joint Committee on Cancer (AJCC) has 2 definitions of stage III adrenocortical carcinoma: 1) lymph-node negative disease (T3-4N0M0) or 2) lymph-node positive disease (TanyN1M0). Patients with stage IV disease must have metastatic spread (TanyNanyM1) [ ]. Even among those with surgically resectable disease, 70% of patients may have a recurrence within 28 months, implying aggressive tumor biology [ ]. Characterizing which patients are at higher risk for poor oncologic outcomes may help define roles for adjuvant treatment, closer surveillance schedules, and clinical trial enrolment. Though a paucity of such literature exists, owing to the disease’s rarity, prior literature suggests that lymph node involvement portends a worse prognosis. Importantly, this represents an opportunity for more precise stratification within the AJCC staging system, to improve alignment of stage and tumor risk [ , , ].
In this study, we assessed survival outcomes in patients with clinical stage III lymph node negative, clinical stage III lymph node positive, and clinical stage IV disease. We hypothesize that patients with clinical stage III lymph node positive adrenocortical carcinoma will have inferior survival compared to those with clinical stage III lymph node negative disease. Instead, those patients with stage III node positive disease will exhibit survival patterns similar to patients with stage IV disease (i.e., those with metastasis). Consequently, we should consider an updated staging classification that differentiates between stage III lymph node positive and lymph node negative disease.
2
Methods
2.1
Study population and outcomes
The National Cancer Database (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC’s NCDB are the source of de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions by the authors. There are over 1,500 accredited hospitals that are required to report new cancer diagnoses to the NCDB. The NCDB captures >70% of new cancer cases reported each year. Information regarding patient demographics, cancer staging, tumor characteristics, surgical treatment, and patient prognosis is recorded [ ].
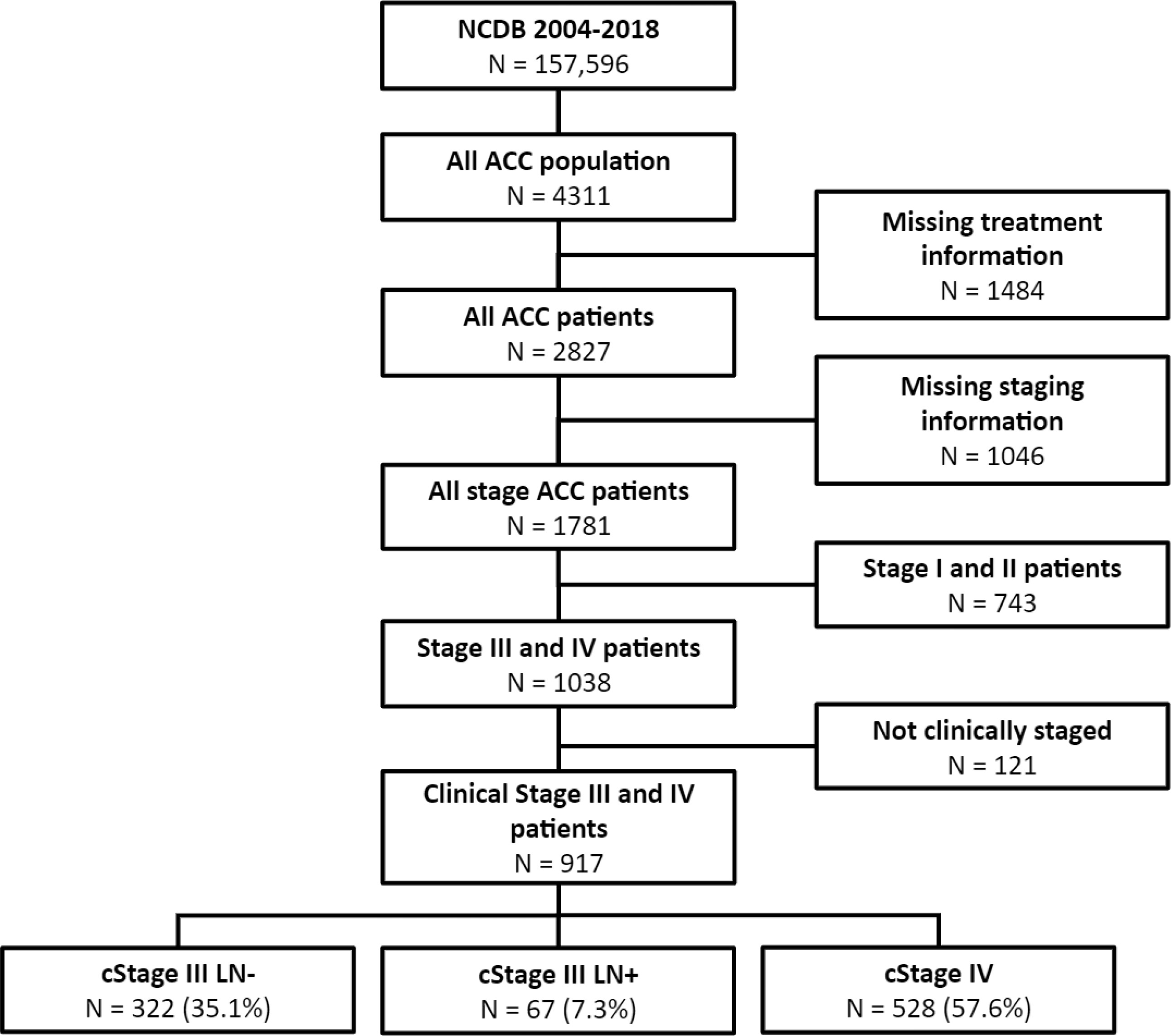
From the NCDB we captured 4,311 patients with adrenocortical carcinoma from 2010 to 2017. We included only those with complete treatment and clinical staging data ( N = 1,781) ( Fig. 1 ). Only those with clinical stage III or IV disease were included ( N = 917). Only 109 patients with stage III or IV disease and complete pathologic data were found in the NCDB.
Our primary outcome was overall survival. The primary exposure was presence of clinical lymph node positive disease in patients with stage III adrenocortical carcinoma. We adjusted multivariable models for age, receipt of surgery, receipt of systemic therapy and Charlson Comorbidity Index.
2.2
Data analysis
Patients from the NCDB were stratified into 3 groups by clinical staging: 1) those with lymph node negative stage III disease (cT3-4N0M0); 2) those with lymph node positive stage III disease (cTanyN1M0); and 3) those with stage IV metastatic disease (cTanyN0- 1M1). Patient characteristics were enumerated. Kaplan-Meier survival estimates and Cox proportional hazards regression models assessed overall survival between stage III (lymph node positive and lymph node negative) and stage IV disease. Survival estimates and 95% confidence intervals (95% CIs) were calculated from survival functions at 12, 24, and 36 months. In an effort to assess the impact of treatment on survival, Kaplan-Meier survival estimates were assessed between those who did and did not receive treatment of any kind in stage III lymph node positive disease as well as stage IV disease. All data analyses were conducted using R Statistical Software (version 4.3.0; R Foundation for Statistical Computing, Vienna, Austria).
3
Results
Final analysis included 917 patients from 2010 to 2017, 322 (35.1%) patients with lymph node negative stage III disease, 67 (7.3%) patients with lymph node positive stage III disease, and 528 (57.6%) with stage IV disease. Demographic information for each cohort is described in Table 1 . Table 2 Median follow-up was 11.07 months (IQR 3.75-30.06). The mean age of the stage III lymph node positive group was 58.1 years (SD 15.2) compared to 54.0 (SD 17.5) and 54.2 (SD 16.4) for the stage III lymph node negative and stage IV groups, respectively. A greater percentage of patients with stage III lymph node negative (75.8%) disease received surgery, compared with stage III lymph node positive (58.2%), and stage IV (27.1%) disease. Similarly, patients deemed stage III lymph node negative (56.2), underwent systemic therapy more commonly than those with stage III node positive (43.3%) or stage IV (36.2%) disease.
| Demographics | cStage III LN (-) | cStage III LN (+) | cStage IV | |||
|---|---|---|---|---|---|---|
| Variable | Count | Percentage/SD | Count | Percentage/SD | Count | Percentage/SD |
| Total | 322 | 67 | 528 | |||
| Lymph node dissection * | ||||||
| LN dissected | 81 | 25.2% | 36 | 53.7% | 72 | 13.6% |
| LN not dissected/unknown | 241 | 74.8% | 31 | 46.3% | 456 | 86.4% |
| Tumor grade | ||||||
| 1 | 8 | 2.5% | 1 | 1.5% | 9 | 1.7% |
| 2 | 10 | 3.1% | 2 | 3.0% | 8 | 1.5% |
| 3 | 38 | 11.8% | 5 | 7.5% | 56 | 10.6% |
| 4 | 21 | 6.5% | 1 | 1.5% | 22 | 4.2% |
| Cell type undetermined | 245 | 76.1% | 58 | 86.6% | 433 | 82.0% |
| Received surgery * | ||||||
| Yes | 244 | 75.8% | 39 | 58.2% | 143 | 27.1% |
| No | 78 | 24.2% | 28 | 41.8% | 385 | 72.9% |
| Systemic therapy * | ||||||
| Yes | 181 | 56.2% | 29 | 43.3% | 191 | 36.2% |
| No | 141 | 43.8% | 38 | 56.7% | 337 | 63.8% |
| Chemotherapy * | ||||||
| None | 179 | 55.6% | 29 | 43.3% | 190 | 36.0% |
| Neoadjuvant | 6 | 1.9% | 2 | 3.0% | 20 | 3.8% |
| Adjuvant | 118 | 36.6% | 23 | 34.3% | 113 | 21.4% |
| Unknown/Unknown sequence | 19 | 5.9% | 13 | 19.4% | 205 | 38.8% |
| Age, y | 54.0 | 17.5 | 58.1 | 15.2 | 54.2 | 16.4 |
| Sex | ||||||
| Female | 183 | 56.8% | 37 | 55.2% | 322 | 61.0% |
| Male | 139 | 43.2% | 30 | 44.8% | 206 | 39.0% |
| Race | ||||||
| White | 267 | 82.9% | 60 | 89.6% | 445 | 84.3% |
| Black | 42 | 13.0% | 4 | 6.0% | 58 | 11.0% |
| Native American | 2 | 0.6% | 1 | 1.5% | 0 | 0.0% |
| Asian | 7 | 2.2% | 1 | 1.5% | 11 | 2.1% |
| Other | 4 | 1.2% | 1 | 1.5% | 14 | 2.7% |
| Charlson comorbidity index | ||||||
| 0 | 233 | 72.4% | 50 | 74.6% | 389 | 73.7% |
| 1 | 63 | 19.6% | 9 | 13.4% | 98 | 18.6% |
| 2 | 17 | 5.3% | 3 | 4.5% | 28 | 5.3% |
| 3 | 9 | 2.8% | 5 | 7.5% | 13 | 2.5% |
| Distance from treatment center, mi * | ||||||
| ≤6.4 | 68 | 21.1% | 14 | 20.9% | 151 | 28.6% |
| >6.4–16.2 | 67 | 20.8% | 20 | 29.9% | 139 | 26.3% |
| >16.2–31 | 51 | 15.8% | 12 | 17.9% | 71 | 13.4% |
| >31 | 105 | 32.6% | 14 | 20.9% | 137 | 25.9% |
| N/A | 31 | 9.6% | 7 | 10.4% | 30 | 5.7% |
| Annual income * | ||||||
| ≥$63,333 | 85 | 26.4% | 21 | 31.3% | 188 | 35.6% |
| $50,354–$63,332 | 84 | 26.1% | 20 | 29.9% | 116 | 22.0% |
| $40,227–$50,353 | 70 | 21.7% | 14 | 20.9% | 87 | 16.5% |
| <$40,227 | 48 | 14.9% | 5 | 7.5% | 101 | 19.1% |
| N/A | 35 | 10.9% | 7 | 10.4% | 36 | 6.8% |
| Regional education * | ||||||
| <6.3% | 76 | 23.6% | 12 | 17.9% | 135 | 25.6% |
| 6.3%–10.8% | 70 | 21.7% | 23 | 34.3% | 135 | 25.6% |
| 10.9%–17.5% | 81 | 25.2% | 8 | 11.9% | 104 | 19.7% |
| ≥17.6% | 60 | 18.6% | 17 | 25.4% | 118 | 22.3% |
| N/A | 35 | 10.9% | 7 | 10.4% | 36 | 6.8% |
| Insurance status | ||||||
| Private | 171 | 53.1% | 28 | 41.8% | 256 | 48.5% |
| Not Insured | 17 | 5.3% | 5 | 7.5% | 33 | 6.3% |
| Medicaid | 29 | 9.0% | 7 | 10.4% | 59 | 11.2% |
| Medicare | 83 | 25.8% | 27 | 40.3% | 153 | 29.0% |
| Other government | 13 | 4.0% | 0 | 0.0% | 7 | 1.3% |
| Insurance status unknown | 9 | 2.8% | 0 | 0.0% | 20 | 3.8% |
| Hospital type | ||||||
| Academic/Research program | 156 | 48.4% | 31 | 46.3% | 216 | 40.9% |
| Community cancer program | 7 | 2.2% | 3 | 4.5% | 22 | 4.2% |
| Comprehensive community cancer program | 55 | 17.1% | 13 | 19.4% | 129 | 24.4% |
| Integrated network cancer program | 42 | 13.0% | 10 | 14.9% | 62 | 11.7% |
| N/A | 62 | 19.3% | 10 | 14.9% | 99 | 18.8% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree