and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Acute Chest Syndrome
Definition
Acute chest syndrome (ACS) is a potentially life-threatening acute respiratory illness, often preceded by an acute painful crisis. It is characterized by fever, pleuritic chest pain, inspiratory crepitations on auscultation of the chest, and is accompanied by a new infiltrate on chest X-ray (CXR). The broadest definition is simply the presence of respiratory signs and symptoms and a new infiltrate on CXR. It is specific to sickle cell disease (SCD) and general physicians who are not familiar with SCD may misdiagnose ACS as pneumonia, pulmonary edema or adult respiratory distress syndrome and institute inappropriate treatment.
Etiology and Pathophysiology
A variety of insults can precipitate intrapulmonary vaso-occlusion, progressive hypoxemia and lung damage. An infective agent is sometimes identified, more often in children than adults. The most common infections diagnosed are Chlamydia pneumoniae, Mycoplasma pneumoniae and viruses causing pneumonia, including respiratory syncytial virus. Bronchoscopic investigation has demonstrated fat laden macrophages in the airways, supporting the suggestion that acute fat embolism is important in the pathophysiology (Fig. 6.1). It is suggested that infarction of bone marrow during a severe acute painful crisis leads to necrosis and release of fat emboli which can lodge in the pulmonary vasculature. This provokes an acute inflammatory reaction with activation of the pulmonary endothelium leading to adhesion of leucocytes and sickled red cells. The result is a cycle of further hypoxia, sickling and vaso-occlusion. The mechanisms involved in vaso-occlusion, including hypoxia-reperfusion injury, free radical formation and activation of the coagulation proteins and platelets are likely to be involved in driving the process (see Fig. 1.4). Hypoventilation due to excessive pain during respiration, or opioid-induced respiratory suppression can exacerbate the situation further. The consequence of this cycle of insults can be appreciated from post-mortem histology of patients who have died during a severe ACS episode. There is engorgement and occlusion of the pulmonary vasculature with sickled red cells, and sometimes accompanying widespread thrombotic occlusion (Figs. 6.2 and 6.3).
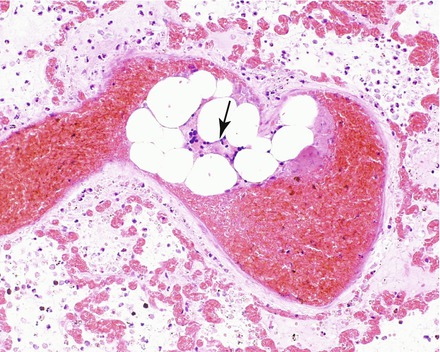
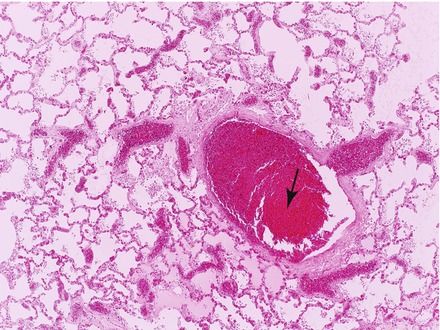
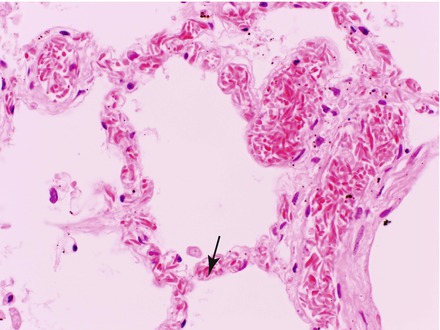
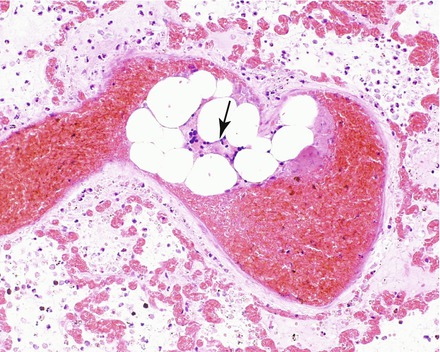
Figure 6.1
Post mortem histopathology section of lung from a patient with HbSS and acute chest syndrome. There is a prominent pulmonary vessel containing sickled red cells and marrow fat embolism (arrow)
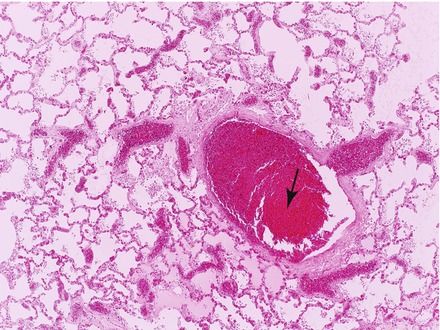
Figure 6.2
Histopathology of acute chest syndrome showing vessels congested with sickled red cells and thrombus (arrow)
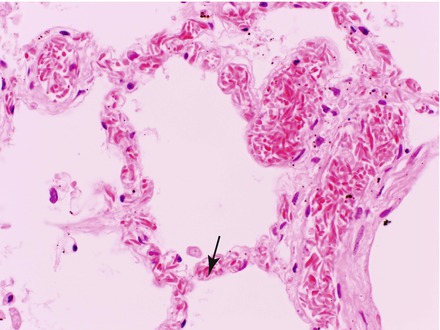
Figure 6.3
Histopathology of acute chest syndrome (high power) showing small blood vessels congested with sickled red cells surrounding alveolar spaces (arrow)
Risk Factors
These include high steady state hemoglobin and WBC, low HbF, a past history of ACS and of asthma.
Incidence
Incidence rates have reduced with increasing use of hydroxyurea in children and adults. Rates in the pre-hydroxyurea era were higher in young children, and in HbSS. In the East London Cohort, the overall rate in childhood for HbSS was 17 per 100 patient years and for HbSC 4 per 100 patient years. In the Co-operative Study of Sickle Cell Disease in North America (CSSD) the incidence in patients over 20 years of age was 8.7/100 person years. ACS is the second most common cause of admission to hospital after acute pain.
Clinical Presentation
Sometimes patients present with clinical features of ACS in the Emergency Department, but more commonly ACS is preceded by a severe painful crisis, and respiratory symptoms develop 24–72 h after the onset of pain, with evolving chest pain, together with fever and falling oxygen saturation on pulse oximetry. Regular monitoring of vital signs (in particular oxygen saturation) and chest examination are therefore essential during admission for painful crisis. The most common respiratory symptoms are cough, chest pain and shortness of breath. The chest pain may be felt in the ribs, sternum, or deeper within the chest, and restricts respiration. Wheezing and hemoptysis may also occur.
Low oxygen saturations (O2 saturations <94 % or a fall of 3 % or more from baseline) is common, and a diagnosis of ACS should be considered in any hypoxic patients with SCD. On examination fever, tachypnoea (and intercostal recession in children), tachycardia and wheeze may be apparent. Chest examination is often abnormal, typically with inspiratory crepitations evolving into reduced breath sounds and signs of consolidation (bronchial breathing, reduced air entry, dullness to percussion) at the lung bases, either unilaterally or bilaterally. Although ACS is more common in HbSS, it can occur with similar severity in all genotypes and diagnosis and management are the same irrespective of genotype.
Clinical Course
The severity is very variable, ranging from a mild illness to a severe life threatening condition. In young children, the picture may resemble a lobar pneumonia, and chest pain is not so prominent, however, we frequently see a severe, rapidly progressive course in young children as well. ACS can progress rapidly to respiratory failure and a minority of patients will need mechanical ventilation. There is a risk of associated neurological complications including acute ischaemic stroke (AIS) and posterior reversible encephalopathy syndrome (PRES) and even without other complications, hospital admission is likely to be prolonged. ACS is a common cause of premature mortality in SCD and is a common cause of death in patients with SCD in the UK.
Differential Diagnosis
Other conditions to consider include pneumonia, pulmonary embolism, fluid overload and atelectasis with hypoventilation due to excessive pain or overdose of opioid analgesics.
Investigations
The investigations in Table 4.3 should always be requested. A fall in hemoglobin from steady state is almost universal, and is associated with markers of increased hemolysis. A low platelet count may be a marker of acute fat embolism and indicates that the course is likely to be more severe. Renal function may deteriorate, particularly in older patients with underlying chronic renal damage. CRP is not particularly helpful in distinguishing infection from acute vaso-occlusion, as it tends to be markedly raised during the course of ACS whatever the etiology. Additional essential investigations are listed in Table 6.1

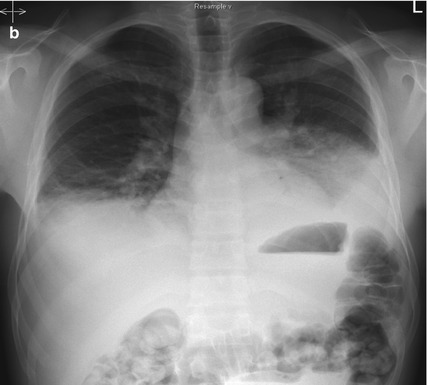
Table 6.1
Additional investigations for ACS
Investigation | Purpose | Comments |
|---|---|---|
Chest X-Ray | Location and extent of infiltration. Identification of pleural effusion, atelectasis, pulmonary edema. | May be normal early in ACS. The usual progression is from unilateral or bilateral basal opacification to involvement of multiple lung segments, air bronchograms, sometimes with pleural effusions (Fig. 6.4). |
Arterial blood gas (on room air) | To assess gas transfer and acid-base balance | Should be done on air. Hypoxemia is very common. Decreasing pO2 and increasing pCO2 are indications for intensification of respiratory support and for exchange transfusion. |
Microbiological investigations | All cases of ACS | It is good practice to request bacterial culture of blood and sputum, PCR of nasopharyngeal aspirate, serology for atypical pneumonia, acute and convalescent samples for Mycoplasma, Chlamydia, Legionella, and urinary pneumococcal antigen. |

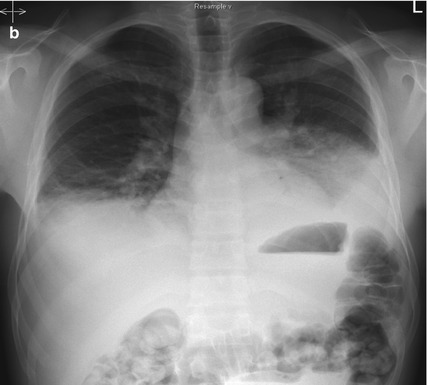
Figure 6.4
Chest X-rays of patient with acute chest syndrome. (a) Day 1, (b) Day 2, showing rapid progression of consolidation
Management
ACS is a medical emergency, requiring early involvement of specialist hematology or pediatric hematology and critical care teams. A suggested management algorithm is shown in Fig. 6.5.
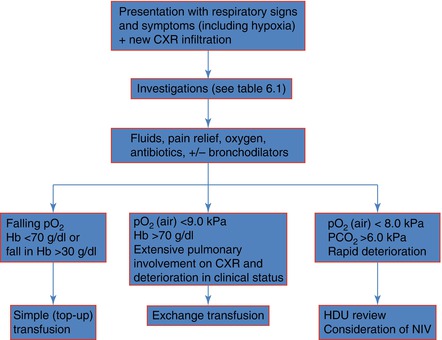
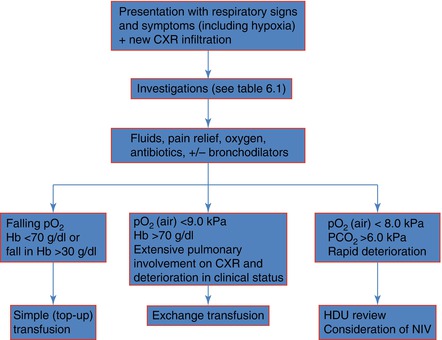
Figure 6.5
Algorithm for management of acute chest syndrome. HDU High dependency unit, NIV Non-invasive ventilation
Oxygen should be given to maintain oxygen saturations >95 %.
Intravenous fluids should be administered to maintain adequate hydration, but it is important not to over-hydrate, particularly in the case of children. Fluid overload is a risk factor for posterior reversible encephalopathy syndrome (PRES) and may precipitate pulmonary edema in older patients with impaired renal function. Usually, replacement of daily fluid requirements is sufficient.
Analgesia is very important to control chest pain and permit adequate ventilation, but opioids must be used carefully to avoid over-sedation and respiratory suppression. Frequent monitoring of pain score, sedation score and respiratory rate is essential. One of the authors has found that intravenous fentanyl given by PCA is useful in this situation. Fentanyl is a potent synthetic opioid with a shorter half-life than morphine. Titration of opioid dose against pain is easier and there is less risk of opioid accumulation and overdosage.
Respiratory support and physiotherapy. There is evidence from a randomized clinical trial that incentive spirometry reduces the risk of ACS in children with chest pain. It is also useful as an adjunct to physiotherapy for ACS. In more severe cases, positive expiratory pressure devices (PEP) can be very helpful. These inputs help to optimize inspiratory effort and avoid atelectasis. Thick airway secretions often build up during the course of ACS, and are only expectorated as the condition resolves. Often they have a striking bright yellow colour due to bilirubin from breakdown of red cells in the lungs. These secretions can cause blockage or airways resulting in segmental collapse and further deterioration in respiratory state. Sedation and mechanical ventilation may be needed and early advice should be sought from the HDU or ITU teams.
Bronchodilators There is no clear evidence showing benefit of bronchodilators, but we recommend their use in patients with evidence of wheezing or a history of asthma in order to optimise airway patency. Corticosteroids have been shown to decrease the length of hospitalization with ACS, but have been associated with an increase re-admission rate because of rebound sickle pain. We do not use steroids routinely for ACS management.
Broad spectrum antibiotics should be prescribed at least until blood and sputum samples are shown to be negative. The local policy for treatment of a severe community acquired pneumonia should be followed, and this should include a macrolide antibiotic to cover atypical organisms. Treatment for the H1N1 subtype of influenza should also be considered.
Transfusion (See Chap. 18)
Blood transfusion can be lifesaving in severe ACS. Stabilization or improvement in respiratory status is often rapid, and it is important to avoid delay once the decision has been made to transfuse. The therapeutic effect is believed to be due to improved oxygen carriage, reduced sickling and relief of vaso-occlusion through dilution of sickled red cells in the microcirculation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






