Hematopoietic cell transplantation is a complex and highly specialized medical procedure offered by selected centers with the requisite expertise and resources. Timely referral to a transplant center is among the most important determinants of successful outcomes. Patients, providers, and payors consider several factors in selecting a transplant center, such as center outcomes and accreditation, patient health insurance coverage, geographic location and accessibility, availability of ancillary and support services, and coordination of care after discharge from the transplant center. Ongoing evaluation and research is needed to advise optimal care models for timely referral to a transplant center and transition of care from the transplant center back to the referring physician.
Key points
- •
Transplant center referrals are a complex, multistep process that involves patients, physicians, and payors.
- •
Timely referral of the patient requires education of the referring physician.
- •
Transplant indications continue to evolve with improved transplant outcome and emergence of better nontransplant therapies.
- •
Care of transplant patients after discharge from the transplant center needs to be considered during initial referral along with other factors.
Introduction
Hematopoietic cell transplantation (HCT) is a complex and highly specialized medical procedure limited to institutions that can dedicate the required resources, personnel, and infrastructure toward a transplant program. It is offered by approximately 170 to 180 transplant centers in the United States. Many states have only one institution that conducts this procedure and some states do not have an active transplant program. Most HCT programs are located in academic tertiary care medical centers. Hence, patients who may be candidates for transplantation frequently have to be referred by their treating hematologist and/or oncologist to a transplant center. The transplant referral process is multistep with many variables that are often not systematically studied. These factors can be classified as physician-, patient-, and payor-based. This article reviews the process of referral to a transplant center and discusses perspectives that patients, referring physicians, and payors may consider when determining which center to select for transplantation. This article is written from the viewpoint of the US health care system. Although referral practices for HCT vary considerably among countries because of the differences in health care system organization and delivery, the general principles discussed in this review are still relevant.
Introduction
Hematopoietic cell transplantation (HCT) is a complex and highly specialized medical procedure limited to institutions that can dedicate the required resources, personnel, and infrastructure toward a transplant program. It is offered by approximately 170 to 180 transplant centers in the United States. Many states have only one institution that conducts this procedure and some states do not have an active transplant program. Most HCT programs are located in academic tertiary care medical centers. Hence, patients who may be candidates for transplantation frequently have to be referred by their treating hematologist and/or oncologist to a transplant center. The transplant referral process is multistep with many variables that are often not systematically studied. These factors can be classified as physician-, patient-, and payor-based. This article reviews the process of referral to a transplant center and discusses perspectives that patients, referring physicians, and payors may consider when determining which center to select for transplantation. This article is written from the viewpoint of the US health care system. Although referral practices for HCT vary considerably among countries because of the differences in health care system organization and delivery, the general principles discussed in this review are still relevant.
Care models for transplant center referral
The mechanism for referral usually depends on where a patient receives therapy for his or her underlying disease and can occur under one of the following scenarios:
- •
For most patients, the transplant referral is initiated by a hematologist-oncologist practicing at a site other than the transplant center (eg, community or another academic institution). Patients are often referred to a transplant center that is located within the same geographic region. This may be a geographic feature, but more often than not, referring physicians in the “catchment” area of a tertiary center have an established working relationship with hematologists and transplant physicians at the tertiary center.
- •
Most transplant centers have a robust hematologic malignancy program and thus some patients receive a within-institution referral. They are treated by a hematologist-oncologist who practices at the same institution but is often not a member of the transplant team. Patients are referred to the transplant program within that institution if they are potential candidates for transplantation.
- •
Some institutions are organized in a manner such that the same physician provides primary management of the underlying disease and then takes care of the transplant portion of the treatment. There is no formal referral in this case. However, personnel who constitute the rest of the transplant team are frequently different, even within the same institution, and some element of transition of care does occur for the patient.
- •
Health care payors often determine the transplant center of choice based on “in-network” and “out of network” privileges.
- •
Finally, the patient may self-refer himself or herself to a transplant center or may do so at the behest of a caregiver or family member.
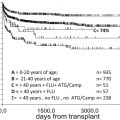
Most of the transplant referrals are initiated by physicians. Pidala and colleagues conducted a survey of practice variation in physician referrals for allogeneic stem cell transplantation (SCT). Despite recent advances in SCT, and the abundance of data showing improved outcomes for older age, there was a significant bias against referring older patients for SCT (age 60 vs age 30; odds ratio, 8.3; 95% confidence interval, 5.9–11.7; P <.0001). Thus, continued education of the referring physician regarding the evolving outcomes of SCT remains an important unmet need. As nontransplant options, albeit noncurative, increase, the role of SCT needs to be continually reassessed. As expected, lack of health care coverage was a deterrent to referral (no coverage vs coverage; odds ratio, 6.9; 95% confidence interval, 5.2–9.1). With the implementation of the Affordable Care Act, it is likely that more patients who currently do not have health care coverage can access life-saving procedures like SCT.
Payors often determine the choice of the transplant center based on “in-network” and “out of network” status of the transplant centers. The “in-network” centers are often in geographic proximity of the patient and maintain excellent outcomes, but on multiple occasions patients have to travel significant distances to go to an “in-network” center. These “forced” referrals are often disruptive to patients and their caregivers.
Some patients are self-referred and “shop-around” for transplant centers with specific expertise in the underlying disease or in search of specific clinical trials. In these instances, it is important to ensure that interim therapy is not compromised while a determination of the transplant center is being made.
Timing of transplant referral
Among transplant recipients, HCT earlier in the disease course is associated with better outcomes compared with transplantation for late-stage relapsed or active disease. Hence, for patients in whom HCT may be potentially considered as a part of the overall treatment plan, it is critical that referral to a transplantation center occurs sooner in the disease course. The logistics of organizing a transplant can take time (eg, identifying a donor, arranging caregivers, additional treatment, and financial clearance), and hence early consultation is appropriate even though some patients may not need a transplant. Box 1 summarizes the general guidelines for the appropriate timing to refer patients to a transplant center that have been developed by the National Marrow Donor Program and the American Society for Blood and Marrow Transplantation. These guidelines need to be continually reassessed as nontransplant therapy changes. The referring physician may have a bias toward “late” transplantation especially in diseases where there are several second- or third-line therapy options, even though they may be noncurative. The absence of prospective randomized controlled trials regarding the benefit of transplant over nontransplant therapy in most disease indications makes decision making complex and contentious. The risk-benefit assessments of early transplant versus nontransplant options are best done in collaboration with the transplant physician. The patient should ideally receive an unbiased balanced opinion of the outcome of early transplant versus delaying the transplant for a subsequent progression. These decisions are often taken in the context of team meetings and should ideally also be attended by nontransplant physicians.
Acute myeloid leukemia
- •
Early after initial diagnosis, all patients including
- ○
First complete remission, except favorable-risk leukemia
- ○
Antecedent hematologic disease (eg, myelodysplastic syndrome)
- ○
Treatment-related leukemia
- ○
Primary induction failure or relapse
- ○
Presence of minimal residual disease after initial or subsequent therapy, if not evaluated previously
- ○
Acute lymphoblastic leukemia
- •
Early after initial diagnosis, all patients including
- ○
First complete remission
- ○
Primary induction failure or relapse
- ○
Presence of minimal residual disease after initial or subsequent therapy, if not evaluated previously
- ○
Myelodysplastic syndromes
- •
Any intermediate or high International Prognostic Scoring System score myelodysplastic syndrome
- •
Any myelodysplastic syndrome with poor prognostic features, including
- ○
Treatment-related myelodysplastic syndrome
- ○
Refractory cytopenia
- ○
Adverse cytogenetics
- ○
Transfusion dependence
- ○
Chronic myeloid leukemia
- •
Inadequate hematologic or cytogenetic response after trial of tyrosine kinase inhibitor
- •
Disease progression
- •
Intolerance to tyrosine kinase inhibitor
- •
Accelerated phase
- •
Blast crisis
Chronic lymphocytic leukemia
- •
High-risk cytogenetics or molecular features (eg, del[11q] or del[17p], unmutated Ig VH)
- •
Short initial remission
- •
Poor initial response
- •
Fludarabine resistant
- •
Richter transformation
Follicular non-Hodgkin lymphoma
- •
Poor response to initial treatment
- •
Initial remission duration of less than 12 months
- •
First relapse
- •
Transformation to diffuse large B-cell lymphoma
Diffuse large B-cell lymphoma
- •
At first or subsequent relapse
- •
First complete remission with high or high-intermediate International Prognostic Index risk
- •
No complete remission with initial treatment
- •
Second or subsequent remission
Mantle cell lymphoma
- •
After initiation of therapy
Other high-risk lymphomas
- •
After initiation of therapy
Hodgkin lymphoma
- •
Primary induction failure or relapse
- •
Second or subsequent remission
Multiple myeloma
- •
All patients after initiation of primary therapy
- •
At first progression
Severe aplastic anemia
- •
At diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree