C1. Red cell disorders in the neonate and childhood
Anaemia at birth
Obstetric accident
• The umbilical artery constricts shortly after birth, preventing blood flowing from the infant to the mother; however, the umbilical vein remains dilated, permitting blood to flow in the direction of gravity. The cord should be clamped while the infant is held within 30 cm above or below the level of the mother. If the infant is held too high, blood will flow back into the placenta, resulting in anaemia in the infant. If the infant is held too low, blood will flow from the placenta to the infant, resulting in an unacceptably high haemoglobin level in the infant.
• Accidental incision of the placenta at caesarian section can result in a massive fetal haemorrhage.
Occult haemorrhage prior to birth
• Fetomaternal haemorrhage may occur at any stage of pregnancy, particularly when there is a need to perform invasive procedures. It may also occur during labour and delivery. The presence of fetal cells in the mothers’ blood may be demonstrated by performing a Kleihauer test. Refer to Fig A4-9.
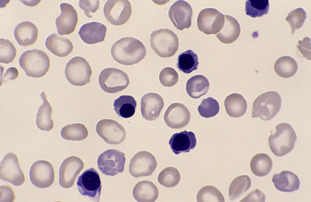
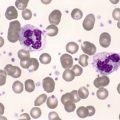
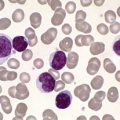
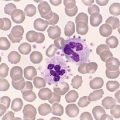
• Twin-to-twin haemorrhage occurs in monozygotic multiple pregnancies, where there is a single placenta. The polycythaemic twin has a haemoglobin level as high as 300 g/L. It develops the hyperviscosity syndrome and has a high bilirubin. The anaemic twin may have a haemoglobin level as low as 35 g/L; it is pale and weak and has cardiac failure. Should the twin-to-twin haemorrhage be a gradual one, there will be a significant difference in birthweight between the twins. Refer to Figure C1-2 and Figure C1-3.
 |
| Figure C1-2 |
• An intracranial haemorrhage can occur in very-low-weight premature infants. Anaemia at birth or a sudden drop in the red cell count and haemoglobin during the first few days of life are the initial clinical signs of an intracranial haemorrhage.
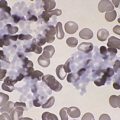
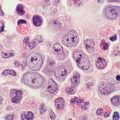
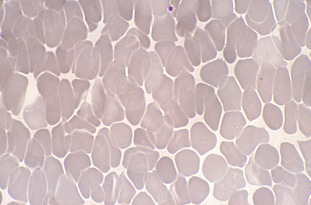
Erythrocytosis at birth
A number of clinical conditions can lead to erythrocytosis at birth. These include hydrops, birth asphyxia, respiratory distress syndrome, pulmonary hypertension and meconium aspiration. The peripheral blood film in these conditions shows increased numbers of nucleated red cells and thrombocytopenia. The nucleated red cell count can often be as high as 500 to 800 nucleated red blood cells (NRBCs) per 100 white blood cells (WBCs). The haemoglobin and red cell count are usually normal. The reticulocyte count is mildly elevated and the DAT is negative. In cases of meconium aspiration, the neutrophils show toxic changes and a left shift.
A similar blood picture, together with thrombocytopenia, may be secondary to an intrauterine infection. The mechanism of this thrombocytopenia is not fully understood. Megakaryocyte numbers are normal or increased. In such cases, a TORCH (Toxoplasma, Others, Rubella, Cytomegalovirus, Herpes simplex) screen should be performed on both the infant and the mother. This group of congenital infections, together with syphilis, can cause neonatal thrombocytopenia. Refer to Fig C1-4.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree