Introduction
Vocal cord paralysis (VCP) is one of the most important complications of thyroid surgery because hoarseness, shortened phonation time, and aspiration derived from VCP significantly reduce the quality of life (QOL) of patients. VCP occasionally occurs for unknown reasons even when the recurrent laryngeal nerve (RLN) is not at risk anatomically. In such cases, VCP may be transient and recover within several months. By contrast, if the RLN was resected surgically because of carcinoma invasion or an accident, VCP will persist. Two points are important for preventing the deterioration of patient QOL. One is to make an effort to avoid injury to the RLN and the other is to appropriately perform reconstruction after RLN resection.
The RLN cannot be preserved in patients with preoperative VCP due to carcinoma invasion. However, surgeons should make an effort to preserve the RLN as much as possible if patients have functioning vocal cords preoperatively. To perform the appropriate surgical management, the RLN on both the peripheral and central sides of the site of the tumor extension must be accurately identified. When a portion of the RLN is surgically resected, the surgeons should reconstruct the nerve without causing deterioration of patient QOL. In this chapter, we describe the intraoperative management of the RLN with thyroid carcinoma invasion.
Intraoperative Management of the RLN With Thyroid Carcinoma Invasion
SHAVING OFF AND PARTIAL LAYER RESECTION
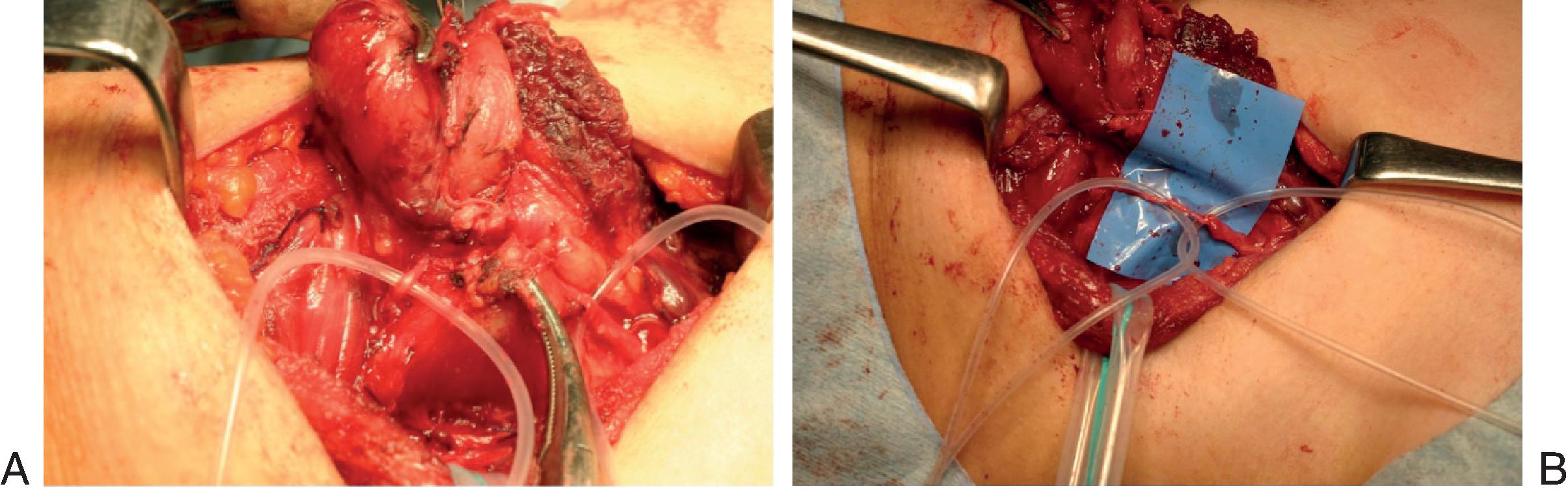
Even in patients with differentiated thyroid carcinoma who have functioning vocal cords preoperatively, the RLN may be found to be involved during thyroid surgery. In such cases, the RLN could be preserved by shaving off the tumor. Nishida et al. reported that the patients who underwent this procedure to preserve the RLN rarely had local recurrence. Our experience agrees with their report. After extensive dissection, the preserved nerve may become thinner than its original size. We denominated this surgical technique as “partial layer resection” if the thickness of the preserved nerve is less than half of its original size ( Fig. 7.1 ). Kihara et al. reviewed the postoperative vocal cord function of 18 patients who underwent this procedure. Of these patients, 2 had functioning vocal cords, 13 had transient VCP followed by full recovery of vocal cord function, and the remaining 3 had permanent VCP, indicating that 15 (83%) of the 18 patients succeeded in having functioning vocal cords postoperatively. Histologic examination of the normal portion of the resected RLN demonstrated that 78% to 82% of the nerve cross-section was composed of perineural connective tissue. This anatomy explains the excellent outcomes after the partial layer resection of the RLN. Even though the preserved nerve becomes thinner than its original size, partial layer resection is worth trying to preserve the nerve and the vocal cord function of patients who had functioning vocal cords preoperatively.
RECONSTRUCTION AFTER RESECTION OF A PORTION OF THE RLN
Background and Mechanism
When a unilateral RLN is resected, the ipsilateral vocal cord becomes paralytic and atrophic, and is usually fixed at a paramedian position. Symptoms are hoarseness, short phonation and aspiration, and decreasing patient QOL. Aspiration can cause pneumonia, which may be life-threatening, especially in elderly patients.
In the personal series of Akira Miyauchi at Kuma Hospital ( Table 7.1 ), of the 721 patients with thyroid carcinoma who underwent an initial surgery between 1998 and 2008, 31 (4.3%) had VCP preoperatively. Thirty of these patients required resection of a portion of the RLN with carcinoma invasion during thyroid surgery. The remaining 690 patients had no VCP on preoperative fiberscopic examination. However, 16 (2.2%) of them required RLN resection due to carcinoma invasion at the time of surgery. In total, 47 patients, accounting for 6.4% of the patients in this series, required RLN resection.
| Preoperative VCP | |||
|---|---|---|---|
| No | Yes | Total | |
| No. of Patients | 690 (95.7%) | 31 (4.3%) | 721 (100.0%) |
| Patients With RLN Resection | 16 (2.2%) | 30 (4.2%) | 46 (6.4%) |
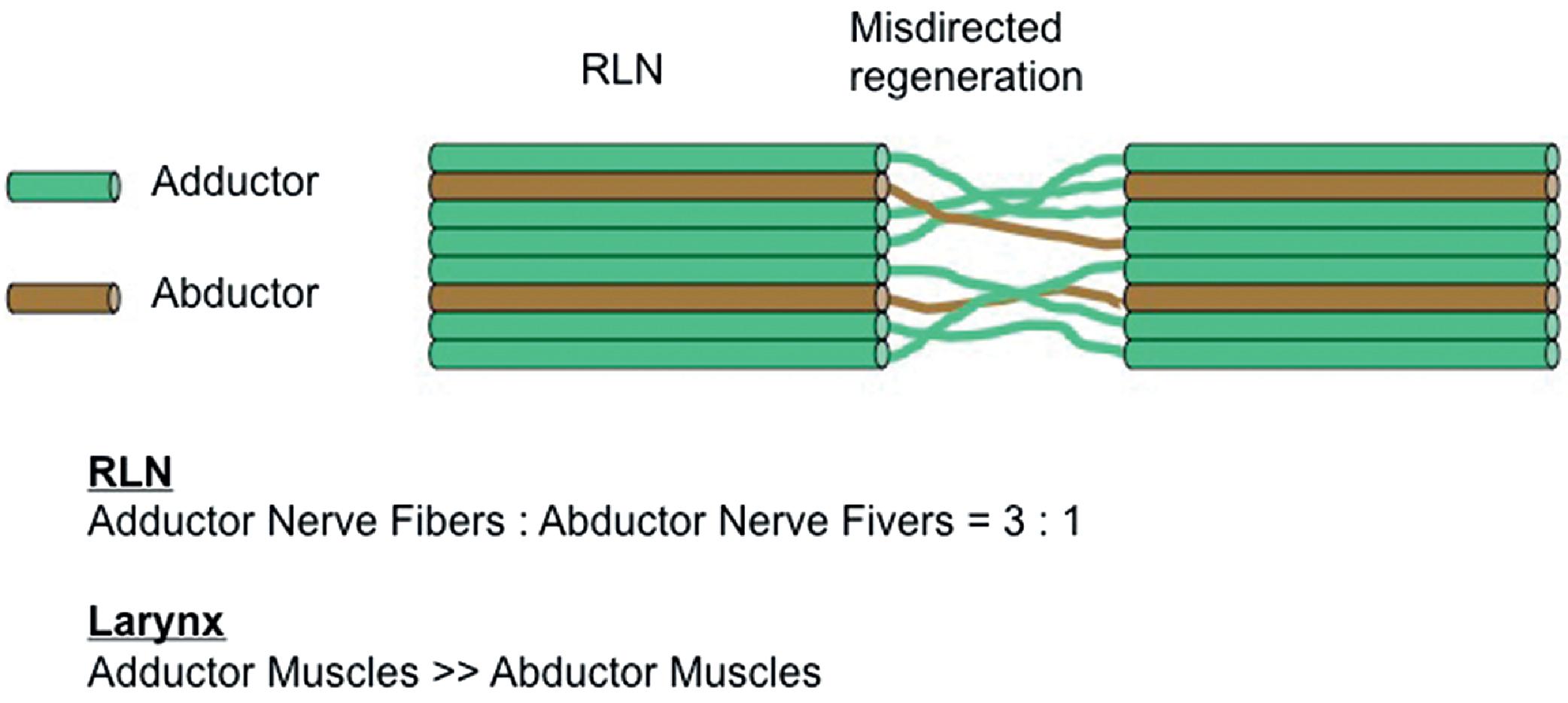
Historically, direct anastomosis of the nerve ends of the transected RLN was performed more than 100 years ago. The first investigators reported that vocal cords on the side of the anastomosis restored their movements after the repair. However, other groups clarified that vocal cord movement was not recovered after anastomosis. Therefore, unfortunately, direct anastomosis of transected RLNs was abandoned for many years. In 1982, Ezaki et al. performed direct end-to-end anastomosis of the transected RLN in seven patients and reported that their voices recovered significantly thereafter, although their vocal cords remained fixed at the median position. According to their explanation of this event, the RLN includes adductor and abductor nerve fibers with no spatial segregation ( Fig. 7.2 ). Even if anastomosis was performed under microscopic surgery, anastomosis of all the fibers precisely is impossible, resulting in a misdirected regeneration among the nerve fibers. Therefore, at the time of inspiration and phonation, the adductor and abductor muscles contract simultaneously. The number of adductor nerve fibers is three times that of the abductor nerve fibers in the RLN, and in the larynx, the adductor muscles are much stronger than the abductor muscles. Therefore, the vocal cord on the side of the nerve anastomosis is fixed in the median position during the inspiration and phonation. This phenomenon is better expressed as synkinesis of the adductor and abductor muscles rather than paralysis. Owing to the reinnervation to its intrinsic muscles, the vocal cord restores tension during phonation, resulting in improvement of phonation.
Several Surgical Procedures for RLN Reconstruction
For reconstruction of the RLN, four surgical procedures can be used, namely direct anastomosis (DA), free nerve grafting (FNG), ansa cervicalis-RLN anastomosis (ARA), and vagus-RLN anastomosis (VRA; Fig. 7.3 ).







