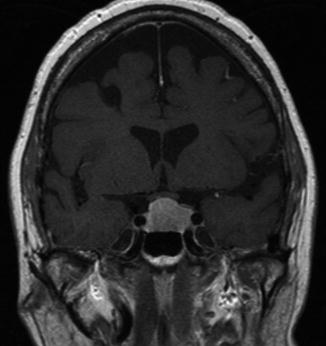
Fig. 9.1
Goldman visual fields showing severe bitemporal hemianopia from chiasmal compression, worse on the right
Visual field deficits relating to a prefixed chiasm are rare and would result in a homonymous field defect which is seen in about 4.2 % of patients with pituitary adenomas.
What questions will you ask regarding ocular motility?
Disorders of ocular motility in pituitary tumours are relatively rare and are reported at between 1 and 6 %. The third (oculomotor) nerve is usually affected, causing diplopia and drooping of the eyelid.
Which other tumours and pathologies could cause visual defects in this region?
Meningioma, craniopharyngioma, hypothalamic tumour (glioma, astrocytoma)
Optic nerve glioma, chordoma, germinoma, dermoid, metastasis
Inflammatory pathology such as Langerhan’s cell histiocytosis, sarcoid, and lymphocytic hypophysitis
Which blood tests, radiological tests, and other tests should now be performed after an initial assessment?
Pituitary region tumours sufficiently large to cause a visual deficit usually require some consideration of surgery, with the notable exception of those tumours secreting prolactin. It is important to establish the serum prolactin level early in the assessment as a prolactinoma is eminently treatable medically without the risks of surgery. The prolactin level should be interpreted with the size of the tumour.
What is the stalk effect?
Secretion of prolactin by the pituitary gland is inhibited tonically by dopamine which is transferred to the anterior pituitary down the pituitary stalk from the hypothalamus in the hypophyseal portal system.
The stalk effect is seen when the serum prolactin level is elevated beyond normal to a level of not more than 4,000 mU/L. It is thought to be due to the tumour causing pressure on or distorting the pituitary stalk and inhibiting the secretion or transport of the inhibitory factor dopamine to the pituitary (Fig. 9.2).
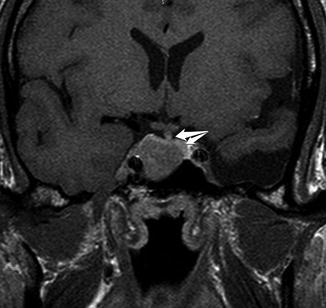
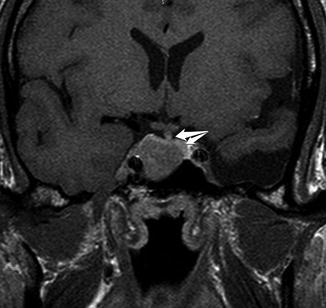
Fig. 9.2
A T1 MRI scan showing a pituitary adenoma distorting the distal pituitary stalk and gland (white arrows)
What other hormone assessments are necessary before considering surgery?
It is important to establish if the patient has hypothyroidism before anaesthesia and a free T4 level should be measured. Patients about to have surgery should have empirical glucocorticoid replacements, and the adrenal axis should be assessed post-operatively. The gonadal hormones and growth hormone can be assessed post-operatively. Patients with pituitary adenomas are very unlikely to have diabetes insipidus pre-operatively. Were this to occur, one should entertain an alternative diagnosis, such as a craniopharyngioma or a dysgerminoma.
What scans should be arranged?
A targeted MRI with T1 sequences pre and post contrast, in the coronal, sagittal and axial planes should be requested (Figs. 9.3 and 9.4). If the patient has a pacemaker. a CT scan with contrast should be requested.