SUMMARY
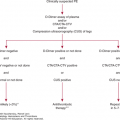
The three major pathophysiologic causes of thrombocytosis are (1) clonal, including essential (or primary) thrombocythemia and other myeloproliferative neoplasms; (2) familial, including rare cases of nonclonal myeloproliferation resulting from thrombopoietin and thrombopoietin receptor mutations; and (3) reactive, in which thrombocytosis occurs secondary to a variety of acute and chronic clinical conditions. This chapter deals with the latter causes of thrombocytosis.
The upper limit of the normal platelet count in most clinical laboratories is between 350,000/μL (350 × 109/L) and 450,000/μL (450 × 109/L). In a sample of 10,000 healthy individuals 18 to 65 years of age, 1 percent had platelet counts greater than 400,000/μL. Only in eight of these 99 individuals was thrombocytosis confirmed 6 months to 1 year later.1 Nevertheless, it is clear that thrombocytosis is a feature of several important disorders, including cancer, and that even a high normal platelet count is associated with morbidity and mortality. In a longitudinal study of healthy Norwegian men, a platelet count in the top quartile of the normal range (from 275 × 109/L to 350 × 109/L) was associated with a twofold increase in cardiovascular mortality over a 12-year follow-up.2 Whether the platelet count per se or an underlying inflammatory condition resulting in both thrombocytosis and accelerated atherogenesis is responsible for these observations is not certain. The causes of thrombocytosis in which the platelet count exceeds the upper limit can be broadly categorized as (1) clonal, including essential thrombocythemia and other myeloproliferative neoplasms, (2) familial, and (3) reactive, or secondary. This chapter focuses on the causes and molecular mechanisms that underlie reactive, or secondary, thrombocytosis.
The regulation of platelet production is discussed extensively in Chap. 1, but a brief discussion here provides the appropriate background for discussion of reactive thrombocytosis. Thrombopoietin (TPO), the ligand for the megakaryocytic growth factor receptor c-Mpl, is the major humoral regulator of megakaryocyte survival, growth, and development, although, curiously, it does not stimulate the final step in thrombopoiesis: platelet release from megakaryocyte proplatelet processes. Although TPO supports the entire continuum of megakaryocyte development from stem cell to mature megakaryocyte,3 other cytokines including interleukin (IL)-6,4 IL-3,5,6 IL-11,7 leukemia inhibitory factor (LIF),8,9 fibroblast growth factor (FGF)-4,10 stromal cell-derived factor (SDF)-1,10,11 interferon (IFN)-γ,12 and granulocyte-macrophage colony-stimulating factor (GM-CSF)13 also affect thrombopoiesis, both in vitro and in vivo. Many of these cytokines act in synergy with other cytokines, including TPO.11,12,14
Acronyms and Abbreviations:
EPO, erythropoietin; ESA, erythropoiesis-stimulating agent; FGF, fibroblast growth factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; IFN, interferon; IL, interleukin; JAK, Janus kinase; LIF, leukemia inhibitory factor; MHC, major histocompatibility complex; NF, nuclear factor; SDF, stromal cell-derived factor; STAT, signal transducer and activator of transcription; TPO, thrombopoietin.
The regulation of thrombopoiesis occurs primarily by humoral mechanisms, with the levels of TPO inversely related to platelet counts.15,16 In contrast, other cytokines shown to affect megakaryopoiesis in vitro do not vary with platelet levels.17 Despite these important insights, the regulation of TPO blood levels is complex and incompletely understood. The liver produces approximately half of all the hormone that circulates, based on platelet production in liver-specific knockout mice.18 However, platelet levels do not affect hepatic TPO production; instead, platelets themselves have an important role in regulating plasma levels, as their receptors for TPO (c-mpl) remove it from plasma.19 Thus, as the platelet count drops, increased free plasma TPO levels stimulate megakaryopoiesis; conversely, as the platelet count rises, depletion of free plasma TPO decreases platelet production. This modulatory mechanism results in the steady-state level of platelet production. However, marrow stromal cells also produce TPO20 and are responsive to platelet products, which serve to down-modulate expression of the hormone.21 A third mechanism by which platelets regulate TPO levels occurs through the Ashwell-Morell hepatocyte receptor, whereby their binding of senescent platelets leads to stimulation of hepatocyte signaling pathways and subsequent expression of TPO.22
Inflammation is the most common cause of secondary thrombocytosis. In one survey, thrombocytosis was believed secondary to one or more inflammatory conditions in nearly 80 percent of all patients with an elevated platelet count. Table 9–1 lists the clinical conditions associated with reactive thrombocytosis. The most common diagnoses in such patients are inflammatory bowel disease and rheumatoid arthritis,23 although most conditions in which the erythrocyte sedimentation rate or C-reactive protein is elevated have been reported to cause secondary thrombocytosis. Although several cytokines and lymphokines are elevated in the blood of such patients, the most compelling evidence suggests that IL-6 and IFN-γ are responsible for the thrombocytosis seen in zatients with inflammation.
|
IL-6 was cloned by several groups of investigators using a number of distinct assays, including antiviral activity, myeloma cell growth, hepatocyte growth, and immunoglobulin secretion.24 The recombinant protein was later found to affect megakaryocyte growth and differentiation, both in vitro and in vivo.4,25,26 The IL-6 gene is present on the short arm of human chromosome 7; encodes a 26-kDa polypeptide produced in almost all tissues from T cells, fibroblasts, macrophages, and stromal cells; and is a key regulator of the inflammatory response.27,28
IL-6 production is dependent on the presence of IL-1 and tumor necrosis factor (TNF)-α, cytokines produced by lymphocytes and monocytes in response to phagocytosis of microorganisms, the binding of immune complexes, and several other innate immune stimuli. IL-6 production is regulated primarily by transcriptional enhancement; regulatory elements responsible for IL-6 promoter activation include nuclear factor-κB (NFκB), adapter protein (AP)-1, CCAAT/enhancer binding protein (C/EBP) α, and C/EBPβ.
Although not critical for steady-state thrombopoiesis, as the combined genetic elimination of c-mpl and the signaling component of the IL-6 receptor (gp130) produces no more severe thrombocytopenia than elimination of c-mpl alone,29 IL-6 contributes to inflammatory thrombopoiesis, primarily by stimulating the hepatic production of TPO.30 Most studies report that patients with inflammation display an increased level of TPO,31,32 but TPO is not the only cytokine responsible for this effect,33 especially when corrected for the thrombocytosis, which would normally act to reduce levels of the hormone. Stimulation of hepatocytes with IL-6 results in enhanced production of TPO mRNA and protein.34,35
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree