Rational Drug Therapy in the Elderly
Robert L. Dickman
CLINICAL PEARLS
Continuously review your patient’s medications with an eye to stopping or reducing as many as possible.
Explore nonpharmacologic treatment for problems.
Simplify the regimen.
Start low, go slow.
Always consider over-the-counter and alternative medication while assessing your patient’s drug regimen.
Do not attribute all symptoms, such as fatigue and memory loss, to old age before considering that they may represent an adverse drug reaction.
Always balance long-term benefits against short-term problems when considering a specific pharmacologic agent.
Be aware of underuse of pharmacologic agents in the elderly.
Be mindful of prescription costs when selecting a drug regimen.
There is perhaps nothing that better characterizes a “geriatric” approach to patient care than the appropriate management of pharmacologic agents in this age-group. Indeed, most primary care clinicians find themselves continually reevaluating older patients’ medication lists, seeking to reduce dosages or eliminate medications altogether. It is the purpose of this chapter to acquaint the primary care physician with the basic pharmacodynamics and pharmacokinetics in the elderly to engender a rational approach to drug treatment in this age-group. In addition, we discuss the concepts of, and the reasons for, polypharmacy and adverse drug reactions. We also review a number of “problematic” medications commonly used by primary care clinicians in the outpatient setting that pose particular problems in this age-group.
Currently, people older than 65 constitute approximately 14% of the US population, but they use approximately 30% to 40% of all prescription and over-the-counter medications. Given our large “baby boomer” population, it is estimated that by the year 2035 a full 20% of the population will be older than 65, and the percentage of medication use will rise proportionally.1 Further, the fastest growing segment of our population is the over-85 age-group, whose use of medication is proportionally greater than that of other seniors. The average person older than 65 uses 4.5 prescription medications daily, whereas the average institutionalized patient uses 7 prescription medications daily. Put in economic terms, the annual prescription drug expenditure per senior was $559 in 1992 and $1,205 in 2000, and the average prescription cost increased by 49% during this period. This economic burden does not even begin to take into account the cost of adverse drug treatment, including hospitalization. It is estimated that 28% of all hospital admissions for this age-group are for drug-related problems
and that 70% of those are for adverse drug reactions.2 Given the sizable and growing prevalence of polypharmacy, it behooves all primary care clinicians who care for older persons to approach this aspect of care rationally and cautiously.
and that 70% of those are for adverse drug reactions.2 Given the sizable and growing prevalence of polypharmacy, it behooves all primary care clinicians who care for older persons to approach this aspect of care rationally and cautiously.
PHARMACOLOGIC CONSIDERATIONS
Pharmacokinetics is the aspect of pharmacology that considers all the factors that contribute to the amount of drug presented to a receptor site. These include absorption, distribution, metabolism, and excretion. There are a number of important pharmacokinetic changes in older persons that indicate prescribing habits in this age-group.
Despite a small increase in achlorhydria and a decrease in gastric motility and gastrointestinal (GI) blood flow in elderly persons, drug absorption from the GI tract is not affected in any significant way. There is little data available on the absorption of transdermal, transbuccal, or transbronchial medications and, in elderly patients, no reason to assume any significant changes in absorption from these routes.
Only a very small reduction in serum albumin level is found as age advances, and therefore, the binding of drugs to carrier proteins is usually not affected.3 In patients who are hypoalbuminemic for any reason (e.g., malnutrition), the amount of unbound bioactive drug may be greater, and therefore, a similar measure of total drug concentration (bound and unbound) might have a greater pharmacologic effect.
The plasma concentration of any medication will be affected by the total volume in which it is distributed. Because total body water decreases in the elderly, hydrophilic drugs such as warfarin, for dosages similar to those for younger people, will have higher plasma concentration when given to older people. Conversely, fat-soluble drugs such as benzodiazepines can accumulate in older people because of an increase in body fat, and therefore, these medications will have a much longer half-life in elderly patients.
Hepatic metabolism in the elderly and its effect on pharmacokinetics is not well understood. Drugs are metabolized in the liver in two phases. Phase I (oxidation and reduction) may be impaired in this group of patients, but phase II (conjugation) appears to be unaltered.3 Further, hepatic blood flow and liver size are reduced, which influences
“first-pass” effects of a number of medications. Therefore, drugs that depend on this hepatic flow, such as isosorbide and lidocaine, should be started at lower dosages.
“first-pass” effects of a number of medications. Therefore, drugs that depend on this hepatic flow, such as isosorbide and lidocaine, should be started at lower dosages.
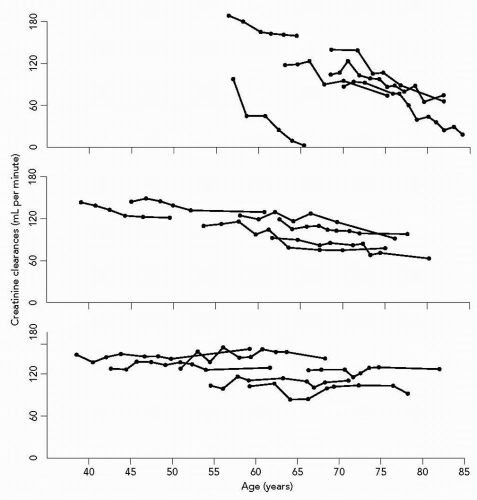
Changes in renal physiology in the elderly have by far the most profound effect on pharmacokinetics in this age-group. It is commonly thought that renal function declines by approximately 10% per decade after the age of 50 in “normal” elderly. These data, however, were based on older cross-sectional studies. Longitudinal studies of “normal aging” suggest that as many as 30% of octogenarians have preserved renal function (see Fig. 4.1).4 It is important, therefore, to have some knowledge of he patients’ renal function over time to accurately gauge the effect of renal function on drug use. Furthermore, because the total protein content may be decreased and muscle mass also diminished in this age-group, both the serum blood urea nitrogen (BUN) and creatinine levels may be lower than that indicated by the actual creatinine clearance. Although a specific formula may be employed to calculate creatinine clearance in the elderly, its use in the ambulatory setting is not practical. Suffice it to say that potentially nephrotoxic drugs (e.g., aminoglycosides) and those primarily excreted by the kidney (e.g., digoxin) should be used with extreme caution in this age-group.
Pharmacodynamic changes in the elderly are more difficult to quantify. Pharmacodynamics considers the effect of drugs on receptors. In many cases, similar serum levels of medications can have profoundly different effects in older versus younger patients. This was demonstrated in the classic study by Greenblatt et al.,5 which showed a more pronounced effect of a long-acting benzodiazepine in older versus younger patients with the same serum level of the drug. On the other hand, β-adrenergic receptor site sensitivity is reduced in the elderly, so more isoproterenol may be necessary to increase the heart rate in the elderly. Similarly, the depressive side effects of β-blockade in this population will also be reduced. In summary, both the pharmacokinetic and pharmacodynamic changes seen in the elderly must be kept in mind when prescribing for patients of this age-group. Particular consideration should always be given to changes in renal function and altered receptor sensitivity.
POLYPHARMACY
When considering special topics that characterize the care of the elderly, polypharmacy is usually at the top of the list. Every time a new geriatric patient is seen in the office, he or she is requested to bring all of his or her medication. These must include over-the-counter and herbal medicines and can sometimes require a shopping bag to transport! There are a variety of reasons for the multiple medications that many older patients use. First of all, such people have many complaints and diseases. Because more people are living into the eighties and nineties, there is simply more time for problems to develop. Conditions such as degenerative joint disease, osteoporosis, and atrial fibrillation are classic examples of problems, the prevalence of which increases with age.
Second, we have many more medications available for use today than we did 20 years ago. Angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARB), cholinesterase inhibitors, osteoporosis medications, and the newer nonsteroidal anti-inflammatory drugs (NSAIDs) are but a few that come to mind. Third, older patients often visit several doctors and communication between them is poor. Often, each physician will treat the particular organ dysfunction for which he or she is responsible with little regard for the other medications the patient may be taking.
Finally, there is yet another reason for polypharmacy in this population: Drug marketing and promotion. It is estimated that the pharmaceutical industry spends on average about $10,000 per doctor for marketing and promoting its products. Physicians are constantly being bombarded with new agents or new formulations of old agents, all of which are reputed to be superior and worthy of prescribing. Evaluating these “presentations,” particularly when they are accompanied by lavish dinners, or for that matter even simple office supplies, is particularly difficult. Similarly, patients themselves are witness to countless media advertisements, many of which seem to at least suggest that the products will make them young again. Therefore, direct consumer advertising helps promote the polypharmacy we all see every day in our offices.
ADVERSE DRUG REACTIONS
CASE ONE
Mr. C. is an 89-year-old man brought to the office by his daughter because of inability to care for himself. He was found by a social worker in his out-of-state home to be very confused, with severe weight loss and rotting food in the refrigerator. On arrival at the office, he is emaciated and disoriented. He has a past history of congestive heart failure and anxiety. His medications include digoxin (Lanoxin) 0.25 mg q.d., diazepam 5 mg b.i.d., furosemide 20 mg q.d., and potassium chloride (K-Tabs) 10 mEq q.d.
On physical examination his blood pressure is 100/50 and his pulse is 60. His heart shows a 2/6 systolic ejection murmur. His chest is clear and he has no edema. He scores 15 out of 30 on the Mini-Mental State Examination. There are no lateralizing neurologic signs. His laboratory data are remarkably normal but for a digoxin level of 3.5 μg/mL. His electrocardiogram shows sinus bradycardia with first-degree atrioventricular block. He is admitted to the hospital and given IV fluids; digoxin is withheld and diazepam is tapered. After 4 days, he “wakes up” and wonders what his daughter has done by taking away his house. He spends the next year traveling independently, visiting his children and grandchildren.
This actual case is a dramatic example of the degree to which adverse drug reactions and inappropriate prescribing can affect the quality of patients’ lives. On the other hand, countless cases of adverse drug reactions occur every day with less life-threatening events than this case, but which can be equally devastating. Adverse drug reactions occur much more frequently in older patients; some studies repeat a rate as high as 17% in this age-group.6 These can be characterized in a variety of ways. This case illustrates two of them. First, inappropriate prescribing of medications known to adversely affect the elderly is perhaps the most potentially devastating. Mr. C. received a long-acting benzodiazepine, which is rarely a drug of choice in the elderly (this will be discussed later in this chapter). Second, prescribing too large a dose of a particular medication can lead to a toxic reaction such as the one we saw in the case. In this example, digoxin (Lanoxin) (whose use in nontachycardic congestive heart failure could be questioned in the first place) at such high doses could (and almost always does) lead to toxicity. Furthermore, when monitoring the effects of digoxin (Lanoxin), drug levels alone will not be sufficient and clinical judgment is paramount.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree