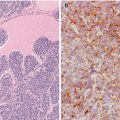
Fig. 2.1
Hobnail (micropapillary) variant of papillary thyroid carcinoma. This variant typically shows a variable combination of papillary (a), micropapillary (b) and follicular growth pattern (c). Both the papillae and the follicles are lined by hobnail cells with dark chromatin. Isolated nuclei with nuclear clarification and pseudoinclusions can also be seen (arrows). In some cases, the cytoplasm is abundant and eosinophilic (c)
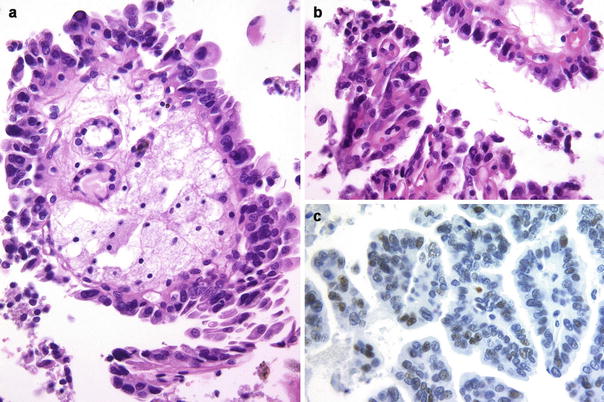
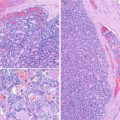
Fig. 2.2
Hobnail (micropapillary) variant of papillary thyroid carcinoma. In this variant, hobnail cells are usually associated with a micropapillary pattern of growth evidencing a loss of polarity and cohesiveness (a, b). In contrast to what occurs in classic papillary carcinoma, nuclear p53 immunoexpression is usually found in this variant (c)
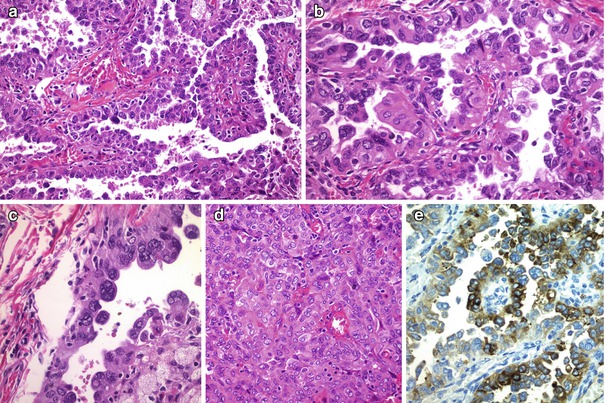
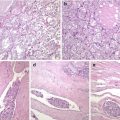
Fig. 2.3
Hobnail (micropapillary) variant of papillary thyroid carcinoma. This case showed in addition to papillary areas with typical hobnail cells (a, b), tumour cells with nuclear pleomorphism (c) and solid growth pattern areas (d). Tumour cells showed positivity for thyroglobulin (e) (Courtesy of Olga Prieto Gómez, Pontevedra, Spain)
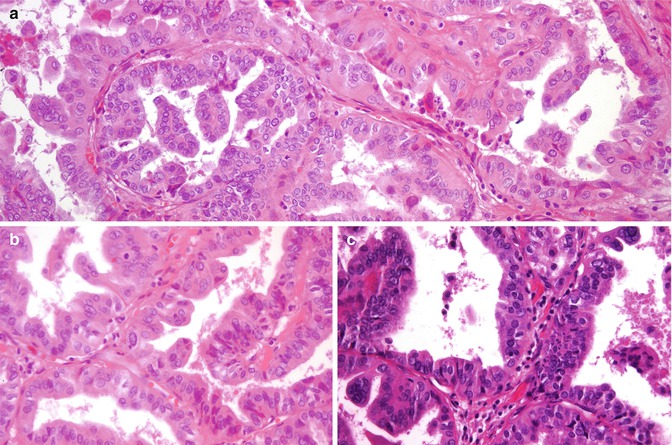
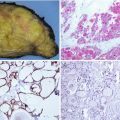
Fig. 2.4
Hobnail (micropapillary) variant of papillary thyroid carcinoma. In the three microscopic photographs of this same case of hobnail variant of PTC, micropapillary pattern of growth coexist with tall/columnar pattern, tumour cells showing tall, dense eosinophilic (oncocytic) cytoplasm with mild (tall cell like) or prominent nuclear stratification (columnar cell like) (a–c)
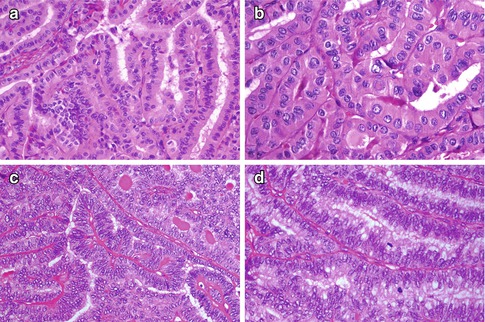
Fig. 2.5
Tall and columnar cell variants of papillary thyroid carcinoma. Hobnail variant of papillary thyroid carcinoma (PTC) can be mixed with other aggressive histologic variants such as tall cell and columnar cell variants in varying proportions. However, by definition, tall cell variant of PTC is made by cells that are two to three times taller than wide and which show abundant eosinophilic cytoplasm (oncocytic) (a, b). Typical nuclear features of papillary carcinoma are present, and nuclear pseudoinclusions are usually easily found (b). Since tall cell areas are frequently present in otherwise classic PTC, at least 30% of all tumour cells are reasonably required for the diagnosis of tall cell variant of PTC. Columnar cell variant of PTC is composed of columnar cells with marked pseudostratification that, at variance with the tall cell variant, lack typical nuclear features of PTC (c, d). The neoplastic cells show occasional clear cytoplasm reminiscent of an endometrioid adenocarcinoma (d), and coexistence of round tubular follicles with prominent nuclear pseudostratification may mimic an intestinal adenocarcinoma. Tall and columnar cell variants of PTC are both positive for thyroglobulin but lack hobnail features and micropapillary growth pattern
Mitotic figures are more frequent than in conventional PTC [3–6, 9, 10]. The Ki-67 index is about 5–10% [3, 7, 8]. Foci of necrosis were detected in about 5% of cases and lymphovascular invasion is seen in more than half of the cases. Some papillae may have stalks composed of loose myxoid stroma or may contain lymphocytes or foamy macrophages (Fig. 2.2). Psammoma bodies are rarely seen. Thyroiditis and nodular hyperplasia in the remaining thyroid tissue have been described in some cases. Coexistence of small foci of undifferentiated carcinoma has been reported in two cases, and tumour progression from HV of PTC to undifferentiated carcinoma either in the tumour recurrence or in metastases can also been seen [4] (Fig. 2.6). Although hobnail features are more commonly observed in association with poorly differentiated thyroid carcinoma (PDTC) (22%) than with PTC [5] (1.3%), differential diagnosis between HV of PTC and PDTC should be made according to the Turin criteria [15] (see Chap. 4). Interestingly, numerous small papillary formations partially covered with hobnail cells are typically seen in the diffuse sclerosing variant of PTC, but in this variant, the papillae are located within intrathyroidal cleft-like spaces, associated with extensive squamous metaplasia, large number of psammoma bodies, lymphocytic thyroiditis and prominent fibrosis [1] (Fig. 2.7). Hobnail-like features may also occur as degenerative changes in cystic areas, but in this setting, the lesions do not display an infiltrative component and lack typical nuclear features of PTC.
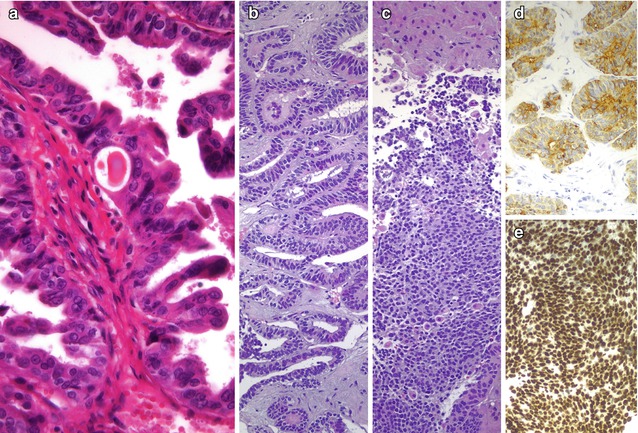
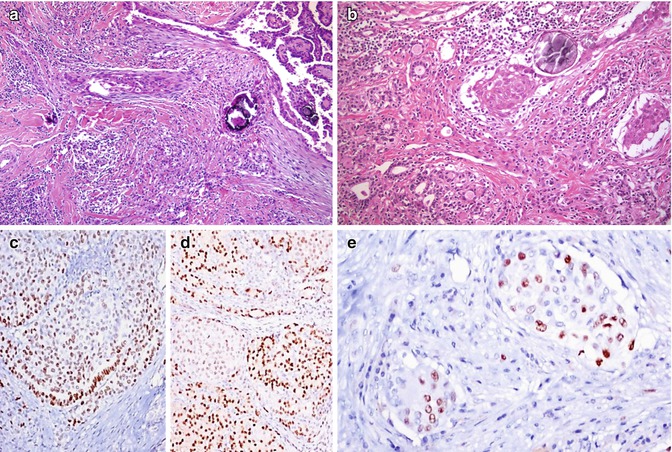
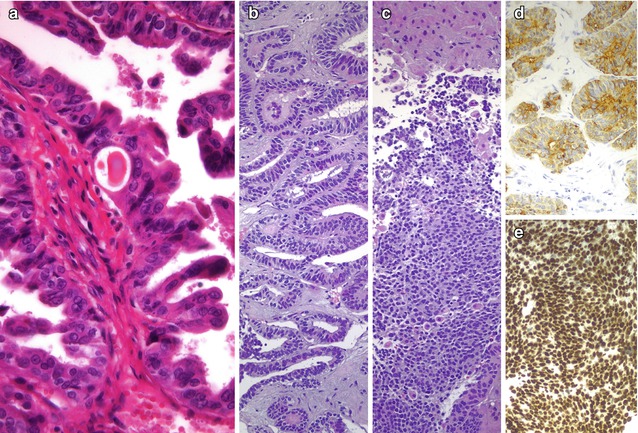
Fig. 2.6
Hobnail (micropapillary) variant of papillary thyroid carcinoma. In this case with typical morphology of hobnail variant in the primary thyroid tumour (a), liver metastasis showed two neoplastic components: columnar cell papillary thyroid carcinoma areas (b), positive for thyroglobulin (d), merging with solid areas composed of undifferentiated round cells (c) with negativity for thyroglobulin but showing positivity for thyroid transcription factor (TTF-1) (e). See [9] for additional details
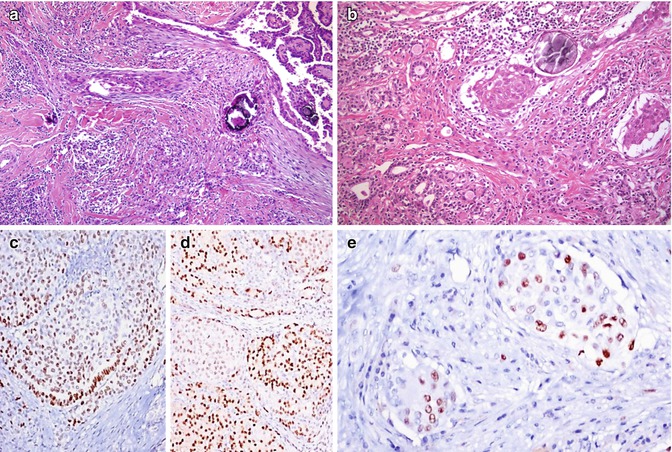
Fig. 2.7
Diffuse sclerosing variant of papillary thyroid carcinoma. In this variant there is diffuse involvement of one lobe or of the entire gland characterized by dense sclerosis, numerous psammoma bodies , papillary structures, prominent squamous metaplasia and background changes of chronic lymphocytic thyroiditis (a, b). Papillary formations partially lined by hobnail cells are typically seen (a). Tumour cells are positive for TTF1 (c), PAX8 (d) and p63 (e)
Tumour cells are immunoreactive for thyroglobulin (Fig. 2.3), thyroid transcription factor-1 (TTF-1), TTF2 (FOXE1), paired box-8 (PAX8), cytokeratins (CK) (CK AE1/3, CK 7, CK 19), epithelial membrane antigen (EMA) , Hector Battifora mesothelial cell-1 (HBME-1) , galectin-3 , cyclin D1 , p27KIP1 and PTEN [3, 4, 6–10, 13]. Interestingly, in some cases, displaying positivity for thyroglobulin in the primary tumour and lymph node metastases, there may be total or partial negativity in distant metastases [3, 8, 13] (Fig. 2.6). Tumour cells are negative for CK 20, thyroperoxidase , calcitonin , chromogranin A and synaptophysin . Strikingly, intense and diffuse nuclear p53 expression is detected in most cases [3, 6–8, 10, 13, 16] (Fig. 2.2).
Fine needle aspiration biopsy (FNAB) is an effective method for diagnosing PTC, including HV cases [4, 8, 10–12]. In HV of PTC, the FNAB samples are typically highly cellular with little colloid and a bloody background. The tumour cells are organized in papillary-like, micropapillary and/or discohesive cell clusters in variable proportions. The characteristic isolated cells are of small to medium size showing eccentric nuclei teardrop cytoplasm (hobnail appearance), the so-called comet-like cells (Fig. 2.8). Syncytial cell clusters with apically placed nuclei may also appear. Typical pseudoinclusions or multiple soap-bubble-like intranuclear inclusions are commonly detected. Variable degrees of nuclear atypia, grooves, nuclear stratification and atypical mitoses can also be seen [4, 10, 11] (Fig. 2.9). Immunohistochemical positivity for thyroglobulin, TTF-1, HBME-1, E-cadherin and p53 can be detected in cytological samples [10].
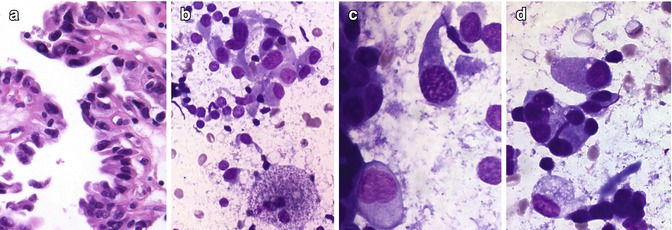
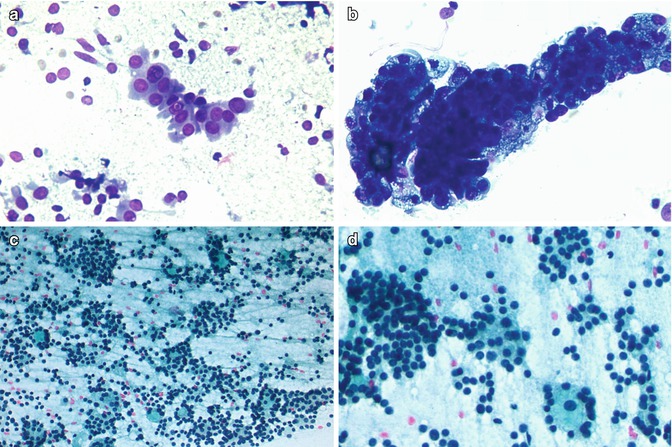
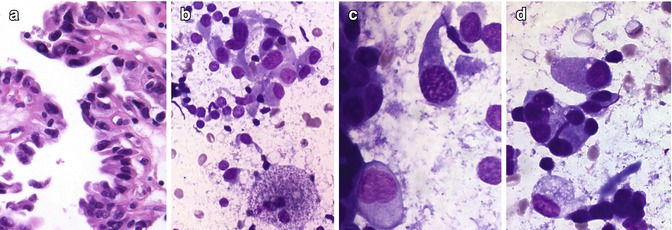
Fig. 2.8
Cytological specimens from hobnail variant of papillary thyroid carcinoma. Hobnail variant of PTC showing discohesive cells with loss of polarity and large nuclei (a). In this variant, samples from fine needle aspiration biopsy characteristically show isolated cells with eccentric nuclei teardrop cytoplasm (hobnail appearance), the so-called comet-like cells (b–d)
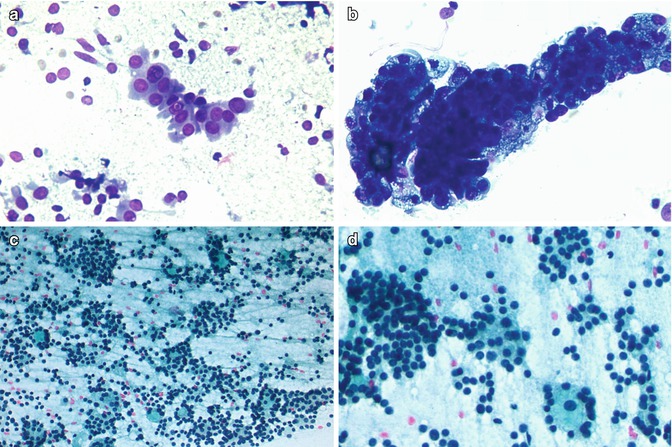
Fig. 2.9
Cytological samples from hobnail variant of papillary thyroid carcinoma. In these samples from the case showed in Fig. 2.3, columnar cells with nuclear pseudoinclusions (a, Diff-Quik stain) and bubbled cytoplasm (b, Diff-Quik stain) are seen. A poorly differentiated component, composed by aggregates of small cells with dark nuclei, is also detected ((c, d), Papanicolaou stain)
In addition to the frequent immunohistochemical positivity for p53 protein, BRAF V600E mutation has been detected in about 70% cases of HV of PTC using both cytological or tissue samples [4, 5, 7, 8, 10, 11, 13]. Concurrent BRAF V600E and TERT promoter mutations were found in one case with undifferentiated carcinoma areas in distant metastases [8], but no TERT promoter mutations were identified in a series of ten cases of common HV of PTC [4]. RET/PTC1, but not RET/PTC3 rearrangements, have been detected in less than 20% of HV cases [7, 8, 13].
Diffuse Sclerosing Variant of Papillary Thyroid Carcinoma
The diffuse sclerosing variant of PTC is more frequent in female, young patients [1]. It is a PTC variant that diffusely involves one or both thyroid lobes, clinically mimicking Hashimoto thyroiditis [1, 2]. This variant is characterized by dense sclerotic stroma involving nests of solid, squamoid, spindled and papillary arranged cells (Fig. 2.7). The cells express focally thyroglobulin, TTF-1, PAX8 and p63 (Fig. 2.7). Abundant psammoma bodies , lymphocytic infiltration and extensive lymph vessel invasion are also present. Lymph node and lung metastases are frequent and may be difficult to diagnose since they may be thyroglobulin (often) and TTF-1 (more rarely) negative. The disease-free survival rate is lower than that of patients with conventional PTC.
Spindle Cell Variant of Papillary Thyroid Carcinoma
Spindle cell transformation or metaplasia has been so far demonstrated in the context of epithelial benign and malignant conditions [1, 2, 17]. Rare cases of PTC show areas of spindle cell differentiation that may represent more than 80% of the tumour [1, 17]. Microscopically, spindle tumour cells are arranged in bundles, frequently showing nuclear grooves and occasional, less frequent, pseudoinclusions (Fig. 2.10). Follicular structures are usually seen in the periphery of the tumour. The spindle cells are actually epithelial in nature and follicular cell originated, as evidenced by their positivity, sometimes focal, for pan-keratins and thyroglobulin, TTF-1 and PAX8 (Fig. 2.10). The differential diagnosis of this tumour includes reactive processes and a variety of primary thyroid tumours and metastatic neoplasms (see spindle cell tumours in Chap. 6). In contrast to reactive changes occurring post FNAB, true spindle cell foci of PTC are not associated with haemorrhage, new capillary blood vessels or hemosiderin-laden macrophages. Distinguishing features from anaplastic carcinoma include the fact that the PTC spindle cells are bland without mitotic activity, pleomorphism and necrosis. Because spindle cell variant of PTC behaves similarly to PTC lacking such features, it is important to separate this variant of PTC from aggressive spindle cell malignant neoplasms (see Chap. 6).
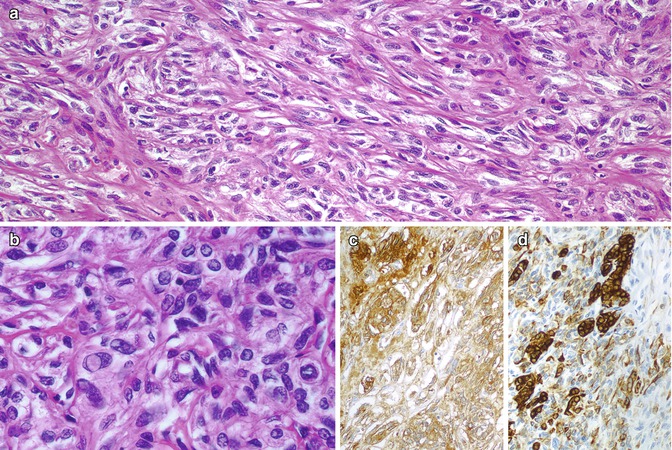
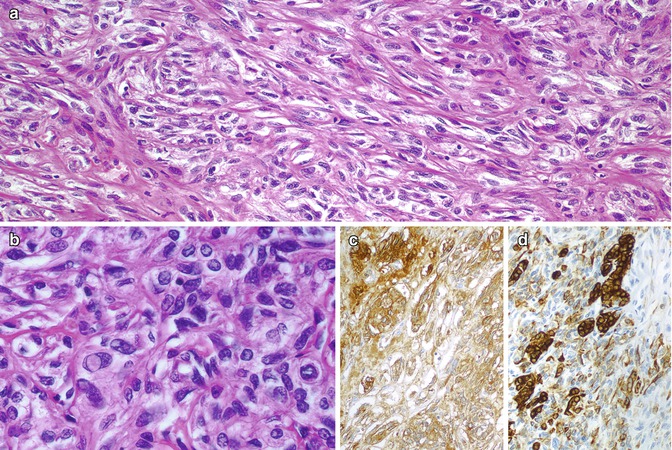
Fig. 2.10
Spindle cell variant of papillary thyroid carcinoma. This variant is mainly composed of spindle cells arranged in bundles having a mesenchymal-like appearance (a). The nuclei of the spindle cells are large, oval and grooved and displayed pseudoinclusions (a, b). Tumour cells are immunopositive for thyroglobulin (c) and keratins (clone AE1/AE3) (d)
Spindle Cell Papillary Carcinoma with Fasciitis-Like Stroma/Fibromatosis
In rare cases , the stroma of PTC is so abundant and cellular as to resemble nodular fasciitis, fibromatosis and other proliferative myofibroblastic processes [1, 2]. PTC with fasciitis-like stroma, also designated as PTC with fibromatosis-like stroma, is a biphasic tumour composed by a stromal benign component and PTC neoplastic foci [1]. The stromal component may predominate obscuring the presence of PTC foci. The stromal cells are spindled, bland looking and arranged in fascicles in a more or less collagen-rich background. This component, thought to be representative of a myofibroblastic population, expresses nuclear beta-catenin and cytoplasmic smooth muscle actin and does not express cytokeratins nor TTF-1 [18]. The PTC foci disclose the typical nuclear features and the respective immunohistochemical profile. The recognition of this malignant component, with the eventual aid of cytokeratins staining to highlight the epithelial cells, will allow the differential diagnosis with other stromal-rich lesions of the thyroid, namely, end-stage/fibrous variant of Hashimoto thyroiditis , IgG4-associated/Riedel thyroiditis , multifocal fibrosing thyroiditis and solitary fibrous tumour (see Chap. 6). The distinction between PTC with fasciitis-like stroma and paucicellular variant of anaplastic carcinoma is not difficult since the latter presents as (very) large tumour with atypical, often bizarre, cells throughout its extension (see Chap. 6). The overall and recurrence-free survival for patients with PTC with fasciitis-like stroma/fibromatosis may be lower than for other PTC variants.
The case illustrated in Fig. 2.11 is a PTC with fasciitis-like stroma diagnosed in a 68-year-old female patient submitted to total thyroidectomy due to nodular adenomatous goitre. The macroscopic examination disclosed a poorly circumscribed nodule in the isthmus with microscopic predominance of a cellular bland stroma component with occasional lymphoid aggregates and scarce PTC foci.
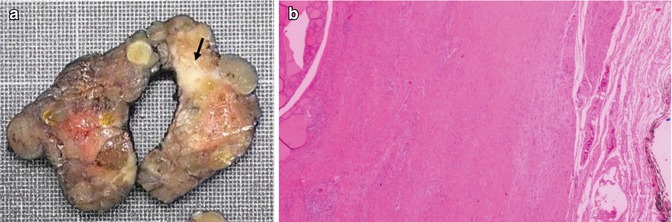
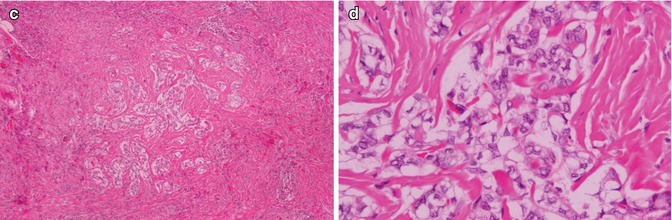
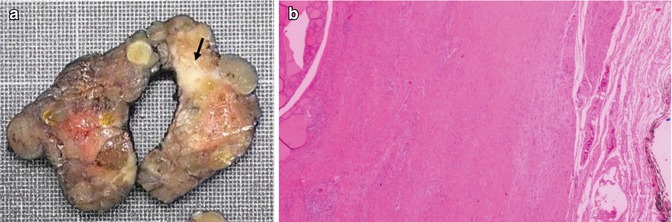
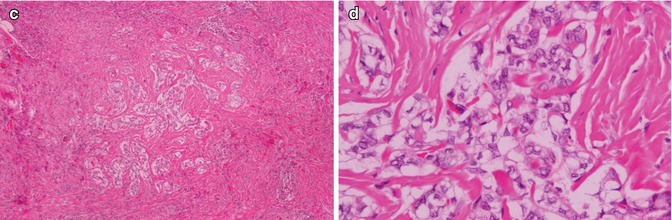
Fig. 2.11
Spindle cell papillary carcinoma with fasciitis-like stroma. Macroscopic features of the tumour (arrow) (a). There is abundant sclerotic stroma without atypical nuclei (b). Scattered foci of epithelial cells are arranged in trabeculae or small follicles (c). Papillary thyroid carcinoma nuclear features can be seen in the epithelial foci (d) (Courtesy of Eva Sigstad and Krystyna Kotanska-Grøholt, Oslo, Norway)
Angiomatoid Variant of Papillary Thyroid Carcinoma
The angiomatoid variant of PTC that develops in the context of Hashimoto thyroiditis can be confused with a vascular tumour if the characteristic nuclear features of PTC in the cells lining the vascular-like spaces are not searched at high magnification [19]. Such vascular-like spaces can display a prominent anastomosing pattern; are lined by TTF-1, PAX-8 and thyroglobulin positive; are cuboidal to flat cells; and are surrounded by a collagenous to myxoid stroma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree