Highlights
- •
Randomized trials show PSA screening decreases prostate cancer-mortality.
- •
Adjunct tests and focus on high-risk patients will improve prostate cancer screening.
- •
A closer look at divergence in PSA screening trials yields similar results.
Abstract
Background
The role of prostate-specific antigen (PSA) testing in prostate cancer (PCa) screening has evolved over recent decades with multiple randomized controlled trials (RCTs) spurring guideline changes. At present, controversy exists due to the indolent nature of many prostate cancers and associated risks of overdiagnosis and overtreatment. This review examines major RCTs evaluating PSA screening to inform clinical practices.
Methods and Materials
We summarize findings from primary RCTs investigating PSA screening’s impact on PCa mortality and incidence: the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, the European Randomized Study of Screening for Prostate Cancer (ERSPC), and the Cluster Randomized Trial of PSA Testing for Prostate Cancer (CAP).
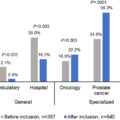
Results
The PLCO Trial randomized men to annual PSA and DRE screening or usual care, reporting no significant difference in PCa mortality between groups at 17 years (RR 0.93, [95% CI: 0.81-1.08]), yet significantly increased detection and concomitant decreased detection in Gleason 6 (RR 1.17, [95% CI: 1.11-1.23]) and 8-10 disease (RR 0.89, [95% CI: 0.80-0.99]) in the screening group, respectively. The ESPRC Trial randomized men across seven European countries to PSA screening every 2-4 years or usual care, noting a 20% reduction in PCa mortality at 9 years (RR 0.81, [95% CI: 0.65-0.98]) and significant decrease in metastatic disease at 12 years (RR 0.70, [95% CI: 0.60-0.82]). The CAP Trial assessed a single PSA screening test’s impact on PCa mortality yielding no significant difference in PCa mortality at 10 years (RR 0.96, [95% CI: 0.85-1.08]). Limitations amongst studies included high contamination between study arms and low compliance with study protocols.
Conclusions
While the CAP and initial PLCO trials showed no significant reduction in PCa mortality, the ERSPC demonstrated a 21% reduction at 13 years, with further benefits at extended follow-up. Differences in outcomes are attributed to variations in trial design, contamination, adherence rates, and PSA thresholds. Future studies are needed focus on optimizing screening intervals, targeting high-risk populations, and incorporating non-invasive diagnostic tools to improve screening efficacy and reduce associated harms.
Randomized trials of PSA screening
The landscape of prostate cancer (PCa) screening with prostate-specific antigen (PSA) testing has drastically evolved over recent decades, with several landmark trials impacting current guidelines as populations have aged and screening tools improved. At present, the PSA blood test continues to serve as the initial screening test for prostate cancer in the United States, due largely to its availability and affordability, as well as level I evidence from randomized controlled trials (RCTs) that regular-PSA screening reduces the risk of developing metastatic disease and reduces PCa-specific mortality [ , ]. Routine utilization of this screening test, however, has not been without notable controversy over the past 2 decades.
Given that PCa is an often slow-growing disease and detection has been associated with lead time bias, the benefits of screening and diagnosis must be considered in light of the risks of overdiagnosis and concomitant overtreatment. Large RCTs have yielded conflicting outcomes, spurring continuous debate and prompting further exploration into the nuances of PCa-screening strategies to shape clinical practice patterns and assess subsequent implications. Difficulty remains in identifying the patient populations in whom early detection leads to improved survival, while mitigating downstream harms of prostate biopsy, overdiagnosis and overtreatment. We herein present an evidence-based summary of the primary RCTs evaluating PSA as an independent screening tool for prostate cancer ( Table 1 ).
| PLCO | ERSPC | Goteborg-1 | CAP | ||
|---|---|---|---|---|---|
| Study Specifics | Population | 76,693 men aged 55–74 | 162,243 men aged 55–69 | 20,000 men aged 55–64 | 419,582 men aged 50–69 |
| Protocol | PSA annually for 6 years, DRE annually for 4 years | PSA every 4 years | PSA every 2 years | Single PSA during study period | |
| Biopsy Trigger PSA (ng/mL) | ≥4 | ≥3 | ≥2.5-3 | ≥3 | |
| Outcomes | NNS | a | 570 at 16 years | 221 at 22 years | a |
| PCa-Mortality (RR) | 1.13 (0.75, 1.70) | 0.80 (0.65–0.98) | 0.56 (0.39–0.82) | 0.96 (0.85–1.08) | |
| Follow-up (years) | Initial study | 7–10 | 9 | 14 | 10 |
| Extended analysis | 17 | 16 | 22 | a | |
| Criticisms | High degree of dilution (screening group) and contamination (control group) | Protocol heterogeneity across sites | High rates of opportunistic testing | High rates of opportunistic testing | |
| Low compliance rate with biopsy | Variable adherence | Variable adherence | |||
Prostate, lung, colorectal, and ovarian (PLCO) cancer screening trial
Study design
The United States (U.S.) PLCO Trial randomized men to receive either annual screening (PSA testing for 6 years and digital rectal exam [DRE] for 4 years) or usual care, as offered by individual providers, to determine the effectiveness of screening with PSA and DRE on PCa mortality [ ]. A total of 76,693 men ages 55 to 74 at 10 U.S. study centers between 1993 and 2001 were recruited. A PSA ≥4.0 ng/mL was considered to be positive prompting a recommendation for diagnostic evaluation to both the participants and their clinicians.
Findings
At 7 years of follow-up, the incidence of prostate cancer was higher in the screening group compared to the control group (RR 1.22, [95% CI: 1.16–1.29]). Overall, similarly low rates of PCa-specific deaths occurred in both the screening and control groups at 2.0 vs. 1.7 per 10,000 person-years (RR 1.13, [95% CI: 0.75–1.70]), respectively.
At almost 17 years of follow-up, there was no statistically significant difference in PCa mortality between the 2 groups with PCa mortality rates of 5.5 and 5.9 per 10,000 person-years (RR 0.93, [95% CI: 0.81–1.08]) in the screening vs. control groups, respectively [ ]. However, a significant increase in detection of Gleason 2 to 6 disease (RR 1.17, [95% CI: 1.11–1.23]) and concomitant decrease in Gleason 8- to 10 disease (RR 0.89, [95% CI: 0.80–0.99]) was identified in the screening arm compared to usual care [ ]. Of the men who underwent at least 1 PSA screening test, 10.4% had at least 1 false positive result. Overall, 12.6% of all men in the study underwent 1 or more prostate biopsies with an overall complication rate of 2.0%, and 67.7% of all biopsies were negative [ ]. A recent secondary analysis of this initial dataset revealed that a PSA level between 0.5 to 0.99 ng/mL and between 1.0 and 1.9 ng/mL in men aged 55 to 60 were associated with 1.5% and 5.4% incidence of clinically significant PCa at 13 years, respectively [ ].
Strengths and limitations
The PLCO trial has been described as an evaluation of organized versus opportunistic screening [ ] because a high degree of contamination—i.e., PSA-testing in the control group—was noted, with very high percentages of men estimated to have undergone any PSA testing throughout the trial period (86% and 99% in the control and intervention arms, respectively) [ , ]. This diluted the power of the trial to detect a statistically significant difference in PCa mortality. In addition, rates of PSA and DRE screening in the control arm increased from 40% to 52% and from 41% to 46% between years 1 and 6, respectively. Furthermore, recommendations for prostate biopsy were not mandated by the study protocol but were at the discretion of the physician and patient. The compliance rate with biopsy was only 40.2% in the first 7-year period and 30.1% in the subsequent study period after a positive screen, which further skews interpretation of the PCa incidence rates reported. The relatively lower percentage of patients who ultimately underwent a biopsy may have also been compounded by a study-defined PSA threshold of ≥4.0 ng/mL, which is higher than that utilized in other screening trials. However, accounting for contamination and increased PCa incidence due to screening and diagnostic work-up, analytic and microsimulation models later confirmed a 27% to 32% relative risk reduction in PCa mortality in PLCO [ ].
Finally, the PLCO study revealed more Black men were diagnosed with aggressive/metastatic PCa compared to White men. However, no association was found between race/ethnicity and PCa mortality. It should be noted that the trial enrolled a very limited percentage of African American men (4.5%), so the trial was likely underpowered for subgroup analyses, representing a limitation of this study’s relatively homogenous patient population [ ].
European randomized study of screening for prostate cancer (ERSPC)
Study design
The ERSPC trial randomized men across 7 European countries to a screening intervention arm compared to no screening to determine the effect of PSA screening on prostate cancer mortality. Those in the screening intervention group were offered PSA testing once every 4 years (every 2 years in Sweden) compared to no screening in the control group, with a PSA threshold prompting biopsy ∼3.0 ng/mL. A total of 182,000 men aged 50 to 74 were initially recruited, with 162,243 men aged 55 to 69 (core age group) included in the final analysis [ ].
Findings
At a median of 9 years of follow-up, PSA-based screening in the intervention arm reduced PCa mortality by 20% (RR 0.81, [95% CI: 0.65–0.98], P = 0.04). At the same time, the intervention arm had a higher rate of overdiagnosis of low-grade disease (72.2% vs. 54.8% Gleason 6 patients in the screening and control groups, respectively), with PCa incidence rates of 8.2% vs. 4.8% in the screening and control groups, respectively. In an intention-to-screen (ITS) analysis, the number needed to screen (NNS) was 1,410 men and 48 additional PCa cases needed to be diagnosed (NND) to prevent 1 man from dying from PCa. When analyzed per protocol, NNS decreased to 1068.
At 13 years of follow-up, PCa mortality remained divergent between the groups at 4.3 vs. 5.4 per 10,000 person-years (RR 0.79, [95% CI: 0.69–0.91)] in the screening versus control groups, respectively. NNS decreased to 781 men screened and 27 men diagnosed to prevent 1 PCa-death, with those numbers further decreasing to 570 and 18 at 16 years, respectively, with a larger absolute benefit in PCa mortality reduction with decreased overdiagnosis [ , ]. No reduction in PCa mortality was observed among men aged 70 to 74 at baseline. The incidence of metastatic disease (mPCa) was significantly lower among men assigned to the screening arm at 12 years of follow-up (RR 0.70, [95% CI: 0.60–0.82]) with NNS 323 and NND 12 to prevent 1 case of metastasis. Overall, 17.8% of men screened at least once received at least 1 false-positive PSA result, with 27.7% of screened men undergoing prostate biopsy, among whom 75.8% did not result in a PCa diagnosis [ ].
In a subsequent follow-up study by Heijnsdijk et al. analyzing the ERSPC 13-year follow-up data in a microsimulation model, a total of 73 life-years gained was reported if annual PSA screening was performed for all men 55 to 69 years of age. However, they also reported a reduction to 56 quality-adjusted life-years (QALYs) due to postdiagnosis consequences (primarily long-term side-effects from curative treatment) and 43% of cancers overdiagnosed (primarily low risk disease) [ ].
When evaluating outcomes based on ERSPC countries separately, the Finnish cohort reported a lower incidence of advanced PCa in the screening arm opposed to the control (HR 0.73, [95% CI: 0.64–0.82]), albeit no statistically significant reduction in PCa mortality (HR 0.85, [95% CI: 0.69–1.04]) [ ]. Similar findings were echoed in Spain at 15 years of follow-up; however, analysis was limited by a relatively smaller sample size and ( n = 4,276) and low overall PCa related mortality rates (0.23%) [ ]. After adjusting for contamination with 19.4% of the control group undergoing screening throughout the study period in the Rotterdam section, the benefit in mortality reduction further increased to 51% [ ].
Strengths and limitations
The ERSPC trial was a well-powered study with extended follow-up reporting a reduction in PCa-mortality, as well as in development of metastases, with implementation of routine PSA screening. Differential treatment between trial cohorts has been posited to introduce bias towards the screening arm raising concerns with internal validity, yet a more recent study reports a minimal difference of 4.2% between the arms, concluding this impact to be negligible [ , ]. However, the trial is limited by heterogeneity across the study centers in recruitment methods, screening protocols, and PSA thresholds prompting biopsy. Although the most common trigger PSA was ≥3.0 ng/mL, wide intra- and inter-site variation throughout the study period was observed.
Goteborg-1
Study design
Goteborg-1, the Swedish arm of the ERSPC trial, recruited 20,000 men aged 50-64 at baseline who were randomized to evaluate the impact of PSA screening every 2 years in the intervention group versus no screening in the control group, with trigger for biopsy prompted at a PSA value between 2.5 and 3 ng/mL. Men in the screening group were invited for biennial PSA screening up to an upper age limit of ∼70 years (range 67–71).
Findings
This study reported a favorable impact of PSA screening, with screening reducing PCa- mortality by almost half over a 14-year period. However, overdiagnosis rates remained high, with an NNS of 293 men and an NND of 12 [ ]. At 22 years of follow-up, the rate ratio for PCa mortality was 0.56 (95% CI: 0.39–0.82), favoring the screening group. A 41% reduction in PCa-mortality was reported with NNS and NND decreasing to 221 and 9, respectively [ ]. Prognostic factors associated with increased risk of PCa death were nonattendance to PSA-screening, starting screening after age 60, and stopping screening at age 70. Opportunistic screening in the control group over time did not have any effect on PCa mortality and led to more overdiagnosis [ ].
Strengths and limitations
The population-based study design initially randomized participants with subsequent invitation for participation, lending for a more representative study with appropriate generalizability.
Cluster randomized trial of PSA testing for prostate cancer (CAP)
Study design
The CAP Trial was designed to evaluate the impact of a single PSA screening test on PCa mortality [ ]. Overall, 419,582 men ages 50 and 69 from 573 primary care practices across the United Kingdom (UK) were enrolled between 2001 and 2009. The intervention group was invited to undergo a single PSA test at some point during the study period, whereas those in the control group received standard of care. A positive PSA level triggering a recommendation for a biopsy was set at ≥3 ng/mL.
Findings
Among the intervention arm, 40% ultimately attended the PSA testing clinic and 36% received a PSA test. Among those who received a PSA in the intervention arm, 11% had a PSA between 3 and 19.9 ng/mL, and 85% of this cohort ultimately underwent a prostate biopsy. Incidence of PCa was higher in the intervention vs. control groups (4.3% vs. 3.6%, RR 1.19 [95% CI: 1.14–1.25], respectively) [ ]. At a median follow-up of 10 years, no significant difference in PCa mortality was identified (RR 0.96, [95% CI: 0.85–1.08]).
Strengths and limitations
A major limitation of this study was the low rate of adherence to invitation to the intervention arm along with potential contamination due to opportunistic screening in the control arms, further diluting the impact of screening on PCa mortality [ ]. Unlike PLCO and ERSPC (including Goteborg-1), which relied on a dynamic, regular screening protocol (every 1–4 years), the intervention in CAP was a single PSA test. Parallel study designs have been attempted, including a screening study conducted in Stockholm, commencing in 1988 [ ]. Such single PSA-screening may reveal many cases of prostate cancer diagnosed at advanced stage (prevalence screen). For PSA screening to reduce PCa mortality, effective protocols have been based on repeat testing at regular intervals.
Conclusions
Although there was no evidence of a benefit on prostate cancer mortality with PSA-testing in the initial analyses from the CAP and PLCO trials, (outside of the PLCO reanalysis using analytical simulation), the ERSPC trial yielded favorable outcomes, with a 21% reduction in PCa-mortality at 13 years of follow-up due to screening. Differential outcomes in study findings may have been attributed to several factors including: power and sample size, high rates of contamination due to exposure to PSA screening in the control arm of PLCO trial, low adherence to invitation to screening in the CAP trial, age groups, PSA threshold cut offs, reported follow-up time and high adherence to screening and biopsy in the ERSPC trial [ ]. Furthermore, a subsequent analysis reported that rates of PCa-mortality were similar between the PLCO and ERSPC intervention groups at 25% to 32% once differences in implementation and settings were accounted for [ ].
Given the low risk of mortality due to prostate cancer in men diagnosed with localized disease, overall high incidence and prevalence, and potential for long lead time bias, study power and extended follow-up continue to be critical to existing and future studies to better assess characterization of screening protocols. Evaluating the role of PSA screening in specific populations (e.g., younger or older men; improved characterization of higher risk patients including African American men, and those with family history) as well as identifying the optimal time intervals (i.e. repeating PSA 6 weeks after initial elevated result instead of proceeding directly to prostate biopsy), and adding adjunctive noninvasive tools remain next steps to identify men most likely to benefit from early detection and intervention. Although not part of the focus of this particular review, it should also be noted that additional tools for screening—i.e.: magnetic resonance imaging (MRI) and blood and urine biomarkers—are now omnipresent in the armamentarium of screening tools. As such, future paradigms incorporating these modalities may better select men with clinically significant PCa (csPCA) for biopsy, simultaneously improving the benefit and reducing the harms of screening. Though existing trials, limited by imperfect and rigid screening protocols, ultimately identified an overall benefit to screening, more nuanced strategies incorporating targeting of higher risk groups, finetuning prebiopsy pathways, and utilizing secondary noninvasive diagnostics can only improve future results. As the management of prostate cancer continues to evolve with improved screening and treatment strategies, the findings of the PLCO, ESRPC, and CAP trials provide crucial stepping stones to better adapt practice patterns and implications.
CRediT authorship contribution statement
Priya Dave: Data curation, Writing – original draft. Sigrid V. Carlsson: Writing – review & editing. Kara Watts: Conceptualization, Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding Sources: This work was supported in part by a National Institutes of Health/National Cancer Institute Cancer Center Support Grant ( P30-CA008748 ) to Memorial Sloan Kettering Cancer Center.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree