This article reviews the history of clinical trials in surgery using breast cancer surgery and rectal cancer surgery as examples. Trials in breast cancer have transformed the surgical management of this disease. Rectal cancer surgery has also changed greatly, but much of this evolution occurred outside the setting of clinical trials. This article highlights the strengths and limitations of surgical trials and suggests that future studies should include pretrial credentialing as a requirement for surgeon participation. More work needs to be done to bridge the gap from trial results to implementation of new techniques in clinical practice.
- •
Clinical trials take a long time to mature and they often slow practice innovation, can be contradictory, and are resource intense, requiring a long time and heavy financial commitment.
- •
Breast cancer trials have guided surgeons to allow for less radical surgery, the separation of the management of the primary tumor from that of the regional disease in the axilla, and they have expanded the role of adjuvant therapies.
- •
Many surgical advances in rectal cancer occurred before the acceptance and availability of clinical trials.
Introduction
Providing a summary on clinic trials in surgical oncology is challenging for several reasons. First, the reader is likely to be familiar with the content of concluded trials. Readers have probably changed their practices based on the trials discussed later. Second, a list of currently open trials would provide an uninteresting review and would likely be outdated by the time of printing. The clinical trial has become the accepted gold standard and the basis for numerous evidence-based guidelines that shape clinical practice, so how can an article add value when the readers already have a rich experience with clinical trials in surgical oncology and they can electronically access lists of relevant trials? We say that, to achieve the goal of adding value, we must explore the past to predict the future.
What impact have clinical trials made as individual contributions to knowledge and as a collective influence on how change in surgery is approached? Most who have worked in health care for 10 to 20 years have seen incremental but pervasive changes in how clinicians practice, from emphasis on the individual practitioner’s experience and perspective to the more global and specific approach fueled by Cochrane Reviews, meta-analyses, and clinical trials. Practice guidelines and accreditation standards, as with most advances in medicine, can be seen as a mixed blessing. They bring undesirable conformity, closing a period in which the individual practitioner had more freedom to work individually with patients, but guidelines based on evidence offer the potential for reducing liabilities and improving the safety and quality of practices (if guidelines are practiced uniformly). We say that the value added in reviewing this topic is the opportunity to examine lessons learned from the experiences with clinical trials that have fueled practice-changing evidence. How did this transformation in practice happen, what role did clinical trials play in the past, and what role are they likely to play in the future? What were the intended and unintended consequences of clinical trials? In addition, this article also addresses the vulnerabilities of practicing based on clinical trial evidence and how these vulnerabilities might be addressed in the future.
Clinical trials: are they relevant in surgery?
The first perception that should be dispelled is that clinical trials do not play a significant role in surgery and that surgeons have not played a significant role in clinical trials. This perception may be true if one simply quantitates the percentage of surgical practice that is driven by clinical trials results. A study by Howes and colleagues in the United Kingdom in 1997 suggested that, in medicine, clinical trial evidence was integrated into 50% of clinical practice, whereas in surgery only 24% of the practice was based on evidence. From a quantitative standpoint, clinical trial evidence in surgery is not as pervasive as for medicine. There is likely always to be some discrepancy between medicine and surgery with respect to the extent of evidence, because medications all require the approval of the US Food and Drug Administrations (FDA), so substantial data must be gathered for each new drug and for each disease-specific indication. No such scrutiny and oversight is required for surgery. All new devices must undergo FDA approval for their stated objective (eg, tissue destruction, stapling, laparoscopic visualization). However, once a device is approved based on evidence that it can perform such functions, it can move swiftly from one site or discipline to another (eg, from an application in bowel to an application in lung). The evidence that is required by law for surgical advances is minimal, and there are few national drivers for surgical research.
Further complicating the situation is that, to examine surgery requires measurement and monitoring of the technical aspects of surgical procedures. This highly expensive endeavor is beyond what government agencies can afford or achieve. Despite this, there is a rich legacy of surgeon-driven science. It was arguably surgeons in the surgical group National Surgical Adjuvant Breast and Bowel Project (NSABP) who greatly changed the practice of breast cancer care. The first part of this article details the lessons learned from breast cancer trials with a summation of both progress made and limitations experienced.
Breast cancer trials: a radical impact on practice
This first story follows a series of breast cancer trials that challenged the radical mastectomy and transformed the practice of breast cancer care. The story starts with Halsted, who described the radical mastectomy in the 1890s. This technique persisted into the 1970s, in large part because surgery was the only therapy available. Consequently, resection of the breast and adjacent axillary tissues and/or adherent structures such as the chest wall made sense for patients with breast cancer given the limited options and the lethality of the disease. Any residual disease, visible or microscopic, was known to result in certain recurrence and likely death. As the story evolved over several decades, it was in the context of the safety and rigor of clinical trials, that this radical approach could be challenged in favor of less extensive surgery and with the adoption of other local-regional and systemic therapies.
To the best of our ability to ascertain, the first studies to challenge the standard but radical nature of the Halsted mastectomy were initiated in London in the 1960s. These early studies may have introduced the concept of breast conservation, but they showed increased mortality for breast-conserving therapy. These initial suboptimal results rendered it difficult to proceed with additional trials on the same subject. Despite this obstacle, a Milan trial, designed to compare outcomes from the Halsted radical mastectomy with quadrantectomy, was approved and began to accrue patients in 1969. Results were published in 1981 and established the safety of breast-conserving therapy.
Several lessons were learned in this early experience. First, clinical trials take a long time to mature and so they slow the process of practice innovation, particularly when the stakes and the degree of uncertainty are high. Second, trials can be contradictory, a problem that continues to be true even today. For those 2 reasons, it is common for most practice-changing trials to be repeated at least once. Just like an experiment in a laboratory, repetition is important for confirming results and creating confidence in the finding. When trial results are not concordant, it is usually because of imperfect understanding of the clinical trials or difference in design. A series of carefully designed trials sequentially migrated the care of the patient with breast cancer from radical mastectomy to the era of breast-conserving therapy and the introduction of radiation and chemotherapy (described later in the article).
In the United States, Fisher and colleagues from 1971 to 1974 randomized 1079 women with clinically node-negative breast cancer to radical mastectomy, total mastectomy, and total mastectomy with nodal radiation therapy. They found no difference in overall survival, disease-free survival, recurrence-free survival, or distant metastasis. They also randomized 586 node-positive patients to radical mastectomy versus total mastectomy with radiation therapy and found no difference in survival. These results remained true after 25 years of follow-up, as did the results of 20-year follow-up in the Veronisi Italian study. This finding led to the conclusion that there was no survival benefit to radical mastectomy, and the radical standard was abandoned in favor of a new, less invasive procedure. The safety net of testing less invasive procedures in breast cancer was the emerging role of radiation therapy. From this point forward, radiation played a more prominent role in the care of the patient with breast cancer.
The next clinical question postulated was whether total mastectomy could be replaced with a less invasive alternative, lumpectomy. Fisher and colleagues randomized patients with operable cancers that were less than 4 cm in size to lumpectomy plus axillary dissection, lumpectomy plus axillary dissection and radiation therapy, and radical mastectomy. They found a lower local recurrence in the group of patients with lumpectomy plus radiation therapy compared with lumpectomy alone (14 vs 39%). There was no difference in overall survival, disease-free survival, and distant metastasis across all groups.
These 3 studies (Milan study, NSABP B-04, and B-06) led to the acceptance of breast-conserving therapy plus radiation therapy as a method of treatment. In addition, total mastectomy or lumpectomy plus radiation therapy were preferred to radical mastectomy.
After accepting breast-conserving therapy as a viable option for management of the primary tumor, multiple international studies showed that radiation therapy in addition to the lumpectomy or quadrantectomy resulted in improved local control. It was again shown that radiation therapy did not offer any survival advantage compared with surgery alone. This finding confirms that radiation, like surgery, is a local-regional therapy. There has never been evidence that radiation therapy could replace surgery altogether, even in cases of complete clinical response after neoadjuvant chemoradiation therapy.
Another line of investigation focused on whether combining one local-regional therapy and a systemic therapy (hormonal therapy with tamoxifen) could be superior to 2 local-regional therapies (surgery and radiation therapy). The NSABP B-21 trial studied whether tamoxifen could be as effective as radiation therapy at controlling ipsilateral disease after lumpectomy in tumors less than 1cm in size. This trial randomized 1009 women after lumpectomy and axillary lymph node dissection (ALND) to tamoxifen alone, radiation therapy plus tamoxifen, or radiation therapy plus placebo. The addition of radiation therapy to lumpectomy was better (local recurrence 9%) than tamoxifen alone (local recurrence 16%) at controlling local ipsilateral disease, and the addition of both tamoxifen and radiation therapy was the best ( local recurrence 3%), regardless of the patient’s hormone receptor status. This finding led to the conclusion that tamoxifen and radiation therapy should be considered even in tumors of less than 1 cm. A similar study by Fyles and colleagues showed similar results: tamoxifen plus radiation therapy improved local and regional control with no difference in overall or disease-free survival. The Cancer and Leukemia Group B (CALGB) group randomized 636 patients older than 70 years with T1N0 estrogen receptor–positive tumors to lumpectomy with tamoxifen only or lumpectomy with tamoxifen and radiation therapy. Local recurrence with tamoxifen alone was 4% versus 1% in the group that received tamoxifen and radiation therapy (statistically significant). There was no difference in overall survival. The investigators concluded that tamoxifen alone after breast-conserving therapy in women more than 70 years old with small estrogen receptor–positive tumors may be considered for a radiation-sparing treatment. With the effort to reduce the use of radiation therapy, systemic therapy has been introduced as a new standard in patients with early-stage disease.
Given the additive benefits of systemic therapy, the logical next step was to add chemotherapy regimens with demonstrated survival benefits in stage IV patients. The NSABP B-20 trial randomized 2306 women to chemotherapy plus tamoxifen versus tamoxifen alone, and the addition of chemotherapy resulted in improved disease-free survival, overall survival, and local recurrence. Therefore, both hormonal therapy and chemotherapy should be considered. A similar study was done in postmenopausal women. This study also showed a trend toward improved overall and disease-free survival for patients receiving both tamoxifen and chemotherapy.
The surgical approach to the primary tumor had been maximally reduced to achieve the greatest degree of breast conservation. However, little progress had been made toward reducing other morbidity, such as lymphedema from axillary dissection. Once systemic therapy was affecting survival, it became possible to consider reducing the radical nature of the surgical management of lymph nodes. A first step toward decreasing the radical nature of breast cancer staging (sentinel lymph node biopsy [SLNB]) was promoted by Krag and colleagues as part of the NSABP B-32 study. They randomized 5611 women with clinically node-negative disease into SLNB followed by immediate ALND versus SLNB alone (ALND only performed if a positive lymph node was found on SLNB). The technical success rate of the SLNB was 97%, with a mean number of 2.1 lymph nodes removed. The SLN-positive rate was also 26% in both groups. When the SLN was negative, the ALND was also negative in 96% for an overall accuracy of 95%. The overall false-negative rate was 10%. In the 26% of SLN-positive patients who went on to ALND, 61% had no further positive disease. The conclusion of the study was that the SLN accuracy rate is high. The Sentinella Italian study had a similar design. The local recurrence rate in the ALND group was 1% versus 5% in the SLNB group (axillary recurrence in 0 vs 1 patient). The SLNB group had less lymphedema, mobility restrictions, and numbness. Additional studies were done confirming less lymphedema and numbness in the SLNB group. The Milan study randomized more than 1000 patients to SLNB alone versus SLNB with immediate ALND and found axillary failures in 0.0004% of the SLNB group versus 0% in the ALND group, with no difference in overall survival or distant metastasis.
Following these studies, SLNB replaced ALND as the technique of choice to stage the disease. To further expand the role of reducing the extent of surgery, patients who were found to have 1 or 2 positive axillary nodes on the SLNB were randomized to completion ALND or no further surgery in the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial. The investigators found no difference in overall or disease-free survival between the groups, suggesting that ALND may be spared in some women with limited nodal disease.
As experience with breast cancer trials grew, there came a realization that breast cancer is a systemic disease and that the risk of systemic failure was more threatening than the risk of local failure. This mentality likely fueled the transition from postoperative adjuvant chemotherapy to neoadjuvant trials. The NSABP B-18 trial randomized 1523 women with T1-T3, N0-N1 tumors to preoperative chemotherapy (doxorubicin and cyclophosphamide [AC]) in patients with operable disease versus postoperative chemotherapy (AC). There was a high clinical response rate in the neoadjuvant group and 9% of patients had a pathologic complete response. There was also nodal downstaging as well as a higher rate of breast-conserving therapy in this group. There was no difference in survival between the preoperative and postoperative chemotherapy groups, but an improvement in survival was seen in the group with a pathologic complete response. The 16-year update to this study concluded that neoadjuvant chemotherapy is comparable with adjuvant AC and may allow breast-conserving therapy for patients who would otherwise require mastectomy. Additional trials examined the role of neoadjuvant aromatase inhibitor therapy in postmenopausal women to increase the incidence of breast-conserving therapy. In the ACOSOG Z1031 trial, 51% of those deemed candidates for mastectomy only at presentation were able to undergo breast-conserving therapy after neoadjuvant therapy. Neoadjuvant also allows a window to judge response to chemotherapy and/or hormonal therapy before the tumor is removed, which may have implications for postoperative adjuvant therapy.
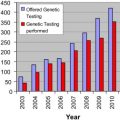
Trials are also being used to validate multigene assays for risk assessment. The Oncotype DX is a diagnostic panel of 21 genes. It has been shown to accurately predict the likelihood of distant recurrence in women with node-negative, estrogen receptor–positive tumors in a subgroup of 668 patients from the NSABP B-14 trial.
A summary of biologic and therapeutic lessons learned from breast cancer trials described the progression from the Halsted radical mastectomy to breast-conserving therapy in most women diagnosed in the modern era. The randomized controlled trials (RCTs) have allowed the separation of management of the primary tumor in the breast from the management of the regional disease in the axilla, preparing for SLNB as a means of staging, which led to decreased morbidity and less radical surgery. In addition, the RCTs expanded the role of adjuvant therapies for the treatment of breast cancer. Radiation therapy is now considered essential in most patients, but it is becoming apparent that it may be safely avoided in the future in select patients (women more than 70 years old with small tumors). The role of neoadjuvant and adjuvant chemotherapies has expanded greatly in the last few decades. In the recent past, RCTs in breast cancer also introduced the concepts of gene sequencing and biomarkers that will help to individualize treatments for each patient. In addition, trials require a long time and large financial commitment from the participating surgeon, and all trials with significant positive or negative findings are generally repeated to confirm the results, often in a different geographic region.
Breast cancer: the limitations of clinical trials
As mentioned earlier, trials inform a minority of clinical surgical practices (roughly 25%). Trials are expensive and time consuming. To properly address a clinical question through a clinical trial costs tens of millions of dollars. The larger the study and the more complicated the trial, the more costly it will be. At a minimum, cancer trials cost on the order of $6000 per patient for enrollment. When diagnostic or therapeutic components that are not standard of care are added, then these costs must be covered by research funding. Sources of funding from government agencies are limited because of competition across many health care sectors. Sources of funding for surgical trials from industry are not as abundant as those in medical fields. Pharmaceutical companies support drug development and clinical testing for FDA filing on a routine basis. Surgeons often have fewer options and must seek creative solutions, although these are available.
Two other limitations deserve to be mentioned. The first is a long period of time from trial results to practice to semination, and the second is the severe discrepancy between the number of patients tested in trials and the number treated in practice. Limitations may be interrelated and so are discussed together.
The lag time from trial reporting to full practice implementation is 17 years. Reasons for this extreme lag time are not completely elucidated. Further, it is not known whether this lag time is beneficial or detrimental, or even whether it is uniform across different studies and practices. It is assumed that the lag time is detrimental, which may be true for therapies that are life saving, low risk, and easy to administer. It is logical that a delay in implementation would be detrimental under these conditions. However, this might not be a reliable assumption where there is a marginal gain from a newly introduced therapy. A marginal gain could be lost if there are only moderate benefits to be gained, and there is potential for real risks because of a lack of experience with the new therapy. For example, after the introduction of laparoscopic cholecystectomy, the rates of common bile duct injuries and lawsuits increased significantly because of the rapid adoption of the procedure. The laparoscopic cholecystectomy was adopted into practice before any formal testing and postgraduate training were available. A marginal benefit could be readily lost if a new practice is widely adopted by practitioners in the absence of standard safety measures inherent in clinical trials.
Clinical trials have several safety measures to protect the patient and practitioners from excessive and unnecessary risk. This safety net starts with narrow eligibility criteria so that sick, frail, at-risk patients are not included in trials. These eligibility criteria are often neglected when the results are reported and practices start to implement new recommendations. Further safety measures and procedures for monitoring and managing toxicities are well defined in trials and help guide clinicians participating in trials. Data safety monitoring boards supervise the trial to be certain the collective experience is following a safe procedure. Could the newness of the procedure or medication, coupled with the absence of these safety mechanisms, be the reason for slow adoption of such therapies and practice? Any drug or procedure that is not familiar to the practitioner should be approached with caution. Future efforts to specifically address critical transitions from trials to practice could benefit all parties.
Further deterrence for early adoption could relate to major discrepancies between the 3% of patients who participate in trials and the remaining 97% who might or might not benefit from the therapy recommended by the trial results. Trial reporting is often considered the final step in the research process and is left to the pharmaceutical company or the principal investigator to disseminate the news and help with implementation of the new standard. The hand-off to practitioners is poor at best. Nuances in the trial design, eligibility, and findings are often difficult to sort through without the explicit aid of the study team. There is no official support for the study team or for the structured dissemination of the findings into practice after the trial is reported. Little is known about the potential for unintended consequences from the introduction of new standards into practice. Before rushing to reduce the 17-year dissemination lag, tools are needed to measure and monitor this process.
Rectal cancer trials
With abundant lessons learned in breast cancer, we considered whether the same lessons could apply to another field of investigation. We chose to review rectal cancer because of the similarities in who funds these cancer trials (eg, National Cancer Institute and pharmaceutical companies) and how they are typically conducted. They are dissimilar based on the many anatomic, physiologic, and biologic differences between the 2 diseases. The story of rectal cancer trials starts later than breast cancer trials and after major changes in surgical techniques (ie, sphincter preservation) had evolved.
Before the nineteenth century, rectal cancer was considered incurable. Attempts to resect rectal tumors resulted in perioperative death or certain early recurrence. With advances in anesthesia and asepsis in the late 1800s, surgery rapidly moved to become a potentially curative therapy for rectal cancer. Radical abdominal perineal resections (APR) for rectal cancer were described by Miles in 1908; APR remains one of the standard, curative approaches to rectal cancer care. The challenge for the APR as an oncologic therapy is the radical transformation it imposes on patients. Sphincter-saving operations were then proposed for tumors of the upper rectum in the 1940s by Claude Dixon at the Mayo Clinic after he showed no difference in survival at 5 years between patients with tumors 16 to 20 cm from the dentate line and tumors 6 to 10 cm from the dentate. This work was followed by technical advancements and the development of surgical staplers as well as evidence of cure rates, leading to the expansion of sphincter-sparing surgery to include middle and lower rectal tumors. These radical changes from APR for all patients to sphincter-sparing surgery for most occurred outside clinical trials.
These sphincter-sparing procedures were adopted widely over time and studied only retrospectively. As new procedures became technically possible (eg, staplers allowed the possibility of sphincter-sparing low anterior resection), questions arose, such as what constituted adequate margins. Reports from observational studies initially supported a 5-cm distal bowel margin, but subsequent studies (nonrandomized) suggested that the traditional 5-cm requirement was not necessary and mucosal margins of between 1 and 2 cm were acceptable. Each time incremental advances in surgical technique were achieved, oncologic outcomes were disputed, and new practices gradually emerged. Advances were supported by the publishing of institutional series. By the 1970s, the field was evolving to include not only surgery but to also include options to participate in experimental protocols that involved the administration of adjuvant radiation therapy.
Because of the poor survival rates in patients with local-regional disease who were treated with surgery alone, investigators questioned whether the addition of radiation therapy could improve the results. Sentinel radiation trials found that postoperative external beam radiation decreased local recurrence rates compared with surgery alone. The NSABP R-01 trial randomized 555 patients with Dukes B and C tumors from 1977 to 1986 into 3 arms following surgery: observation, chemotherapy only (5-fluorouracil, semustine, and vincristine), or radiation therapy only (46–47 Gy). There was an improvement in the local recurrence rate in the radiation therapy arm (25% vs 16%, P = .06) but no difference in overall or disease-free survival. The chemotherapy arm showed an improvement in overall and disease-free survival. In the Medical Research Council Rectal Cancer Working Party study, 469 British and Irish patients were randomized to surgery alone or surgery followed by radiation therapy (42 Gy) from 1984 to 1989. There was no difference in overall survival ( P = .17) or disease-free survival ( P = .18), but there was a benefit with regard to local recurrence (34% vs 21%, hazard ratio0.54, P = .001). Side effects were well-tolerated and late events were rare. Many similar trials were performed, including NSABP R-02, Denmark study, and the Gastrointestinal Tumor Study Group, and all confirmed that postoperative adjuvant radiation contributes to local-regional control.
A meta-analysis of 22 randomized trials (n = 8507 patients) comparing any radiation for rectal cancer (before or after surgery) with surgery alone and found no difference in overall survival (62% vs 63%, P = .06) but a statistically significant reduction in local recurrence rates with radiation therapy.
The parallel clinical question was whether the addition of chemotherapy to radiation would add survival benefit. Krook and colleagues randomized 204 patients from 1980 to 1986 to postoperative radiation therapy (50.4 Gy) versus postoperative chemoradiation therapy (9 weeks of 5-fluorouracil and methyl-CCNU followed by 50.4-Gy radiation therapy with concurrent 5-fluorouracil, followed by an additional 9 weeks of 5-fluorouracil and CCNU). The 5-year overall recurrence in the radiation therapy alone group was 63% versus 41% in the chemoradiation therapy group. Local recurrence (25% vs 13%) and distant metastasis rates (46% vs 29%) were also improved with the addition of chemotherapy, as was overall survival. This study confirmed that chemotherapy combined with radiation therapy was superior to radiation therapy alone. This finding led to a new standard of care that persists today: radiation therapy should be given concurrently with chemotherapy. The National Institutes of Health consensus conference in 1990 recommended postoperative chemoradiation therapy as the standard of care for patients with T3 and T4 tumors as well as for those with nodal disease. Patients with stage I and II disease were observed.
If postoperative chemoradiation was improving survival, investigators next asked whether neoadjuvant radiation could further improve outcomes. The next set of clinical trials was varied in design because some compared neoadjuvant radiation with surgery alone and others compared neoadjuvant therapy with postoperative radiation therapy. Some trials examined short-course radiation and others used standard-course radiation therapy. The European Organization for Research and Treatment of Cancer randomized 466 patients to surgery alone versus preoperative radiation therapy. They found no survival difference but improved local recurrence rates (30% vs 15%). The Stockholm I trial randomized 849 patients to preoperative short-course radiation therapy versus surgery alone from 1980 to 1987. The local recurrence rate and time to failure was better in the neoadjuvant group but, again, no benefit in overall survival was established. An additional finding was a higher postoperative mortality in the group that received preoperative radiation therapy (8% vs 2%).
The Stockholm II trial randomized 557 patients to short-course radiation therapy plus surgery versus surgery alone. In this study, the radiation therapy group benefited in local recurrence, distant metastasis, and overall survival. The Swedish Rectal Cancer Trial also randomized 1168 patients to preoperative short-course radiation therapy versus surgery alone. At the 13-year follow-up, there was an improved overall survival (38% vs 30%) as well as local recurrence rate (9% vs 26%). Follow-up results from this trial showed that morbidity was higher in the neoadjuvant radiation group, specifically the rate of small bowel obstruction. The United Kingdom study, from 1998 to 2005, randomized 1350 patients to preoperative short-course radiation therapy versus postoperative chemoradiation therapy (5-fluorouracil and leucovorin). They found an improved local recurrence rate in the preoperative radiation therapy group (4 vs 11%). The disease-free survival was also higher in the group receiving neoadjuvant radiation therapy (77 vs 71%); no difference was seen in overall survival.
A German trial randomized 823 patients from 1995 to 2002 to preoperative versus postoperative long-course radiation therapy plus 5-fluorouracil. They found no difference in overall or disease-free survival but a local recurrence rate (6% vs 13%) that benefited from neoadjuvant therapy. There was less acute and late toxicity in the preoperative group (but fewer patients in the postoperative group received complete radiation therapy; 54% vs 92%). Many other studies showed similar results with decreased local recurrence rates in groups who received preoperative radiation therapy. Camma and colleagues performed a meta-analysis of all randomized trials that compared preoperative radiation therapy plus surgery and surgery alone; neoadjuvant radiation therapy resulted in improved 5-year overall survival and cancer-specific survival as well as lowered local recurrence rates, but the magnitude of the benefit was small. The summative results of these trials led to the conclusion that neoadjuvant radiation therapy is superior to surgery alone and superior to postoperative radiation therapy.
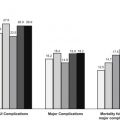
A unique byproduct from these trials was the recognition that local recurrence rates were variable among the studies. This finding led investigators to focus more on the role of surgical technique, specifically the management of the perirectal lymphatic packet (ie, mesorectum). The Dutch trial was the first to require surgeons to perform standardized surgery (total mesorectal excision [TME]) in all trial patients. Patients were randomized to preoperative short-course radiation therapy plus TME versus TME alone. The local recurrence rate at 2 years was 2.4% versus 8.2%, favoring radiation therapy, but no difference was seen in overall survival. The long-term follow-up at 5 years showed the same results with local recurrence rates: 11% versus 6% favoring radiation therapy and no difference in overall survival. The 10-year follow-up results were similar.
As for breast cancer trials, efforts transitioned from local-regional treatments to more systemic treatment. The next clinical question was therefore whether the addition of chemotherapy to the neoadjuvant radiation therapy regimen would add benefit. Bosset and colleagues randomized 1011 patients to preoperative radiation therapy alone, preoperative radiation plus 5-fluorouracil, preoperative radiation therapy plus postoperative 5-fluorouracil, or preoperative radiation plus postoperative 5-fluorouracil. There was a benefit to local control with 5-fluorouracil chemotherapy given at any time point compared with radiation therapy alone. No survival benefit was seen. The Polish study randomized 312 patients to short-course neoadjuvant radiation therapy only versus long-course neoadjuvant radiation therapy plus 5-fluorouracil. There was no difference in disease-free or overall survival, sphincter preservation, or complications. There were more early toxicities in the chemoradiation therapy group.
A French study group randomized 733 patients to preoperative radiation therapy alone versus preoperative radiation therapy with 5-fluorouracil. No difference was seen in overall survival or sphincter preservation, but there was an improvement in the local recurrence rate in the chemoradiation therapy group (8% vs 16%). However, this improvement was balanced by higher toxicity in this group.
A systematic review of 5 RCTs comparing preoperative chemoradiation therapy versus preoperative radiation therapy alone confirmed higher pathologic complete response rates in the chemoradiation therapy group, but this was balanced by higher toxicity.
Following these trials, the algorithm for treating rectal cancer changed further to offer neoadjuvant chemoradiation therapy to patients with bulky T3 tumors, all T4 tumors, and all with suspected nodal disease. Postoperative radiation therapy is reserved for patients who have one of these findings unexpectedly at the time of surgery.
Many RCTs have attempted to determine the value of adjuvant 5-fluorouracil–based chemotherapy following surgery for rectal cancer, but there is unclear benefit in the current available literature (4 total randomized trials). The consensus from the systematic review combining these 4 trials is that additional trials are needed to answer this question.
Although many of the surgical advances in rectal cancer care occurred before the acceptance and availability of clinical trial methodology, the same was not true for the introduction of laparoscopic techniques. When the minimally invasive surgical approach to abdominal disorders became a technical reality, it radically changed the management of the gallbladder. As it was considered for the colon application, it was resisted in oncologic cases. The frequent reporting of port-site recurrences slowed the advancement of laparoscopic surgery for colon cancer until international trials showed the same oncologic outcomes for laparoscopic as for open surgery. Once laparoscopic colectomy for cancer was proved safe and effective, it prompted similar studies in rectal cancer. Many centers considered the possibility of laparoscopic surgery following the same oncologic principles accepted in open rectal cancer surgery. The Conventional Versus Laparoscopic-Assisted Surgery in Patients with Colorectal Cancer (CLASICC) trial included patients with benign and malignant rectal disease (48% had rectal cancers). Laparoscopy shortened the length of hospital stay but resulted in a higher rate of positive circumferential resection margins (12% vs 6%) and worse sexual function in male patients. There were no significant differences in local recurrence, 3-year disease-free survival, and overall survival.
Lujan and colleagues conducted a single-institution study and reported results from their randomized trial that compared open and laparoscopic surgery for rectal cancer in 204 patients. They found no difference in local recurrence, disease-free survival, or overall survival and no difference in involvement of the circumferential resection margins. Additional trials are ongoing to further explore the role of laparoscopy in rectal cancer surgery. ACOSOG Z6051 is a noninferiority trial with endpoints that include number of patients with circumferential resection margins less than 1 mm, distal margin greater than 2 cm, and completeness of TME. Similar trials are in progress in other countries (UK CLASICC, COLOR II, Japan Clinical Oncology Group [JCOG] 0404). Results of these trials are not yet available, and open rectal cancer surgery remains the standard.
Attempts to decrease the radical nature of surgery in patients with early rectal cancer have included local excision techniques (transanal excision and transanal endoscopic microsurgery [TEM]). Many series have been reported but few trials have tested the safety and oncologic benefit of local excision. The study by Lezoche and colleagues randomized 70 patients with T2N0 rectal tumors to TEM versus laparoscopic TME (both groups received neoadjuvant radiation therapy and 5-fluorouracil). With a median follow-up of 84 months, there were no differences in local recurrence rates, rates of distant metastases, or survival outcomes. This study was underpowered to detect small differences in these outcomes. Winde and colleagues randomized 50 patients to anterior resection versus transanal endoscopic microsurgery; there were similar local recurrence and survival rates and decreased morbidity in the TEM group.
However, long-term prospective studies from Memorial Sloan Kettering and the University of Minnesota have shown worse outcomes for the local excision groups when they were followed over time. Additional data from the National Cancer Database suggest that, although the use of local excision techniques has increased greatly, the risk of local recurrence at 5 years was 12.5% for T1 tumors and 22.1% for T2 tumors. An ongoing multi-institutional study, ACOSOG Z6041, follows patients with T2N0 low rectal tumors who were given radiation therapy and capecitabine and oxaliplatin before surgery followed by local excision. If the pathology confirms T0 to T2 disease, the patient is observed and, if T3 or positive margins remain, the patient undergoes further treatment. It remains to be determined whether local excision should be considered for rectal cancers, but the treatment algorithm in the 2010s may include local excision in select patients with T1N0 disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree