Figure 1.1
Incision placement
Figure 1.2
The background radioactivity count level can be obtained by placing the gamma probe over the thyroid isthmus
Figure 1.3
Making the incision
Figure 1.4
Dividing the platysma
Figure 1.5
Dividing the strap muscles in the midline
Figure 1.6
Identifying the abnormal parathyroid gland with the gamma probe
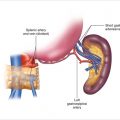
Figure 1.7
Isolating the vascular pedicle
Figure 1.8
Measuring ex vivo radioactive counts from the resected parathyroid gland
Figure 1.9
Injecting local anesthetic in the wound
Figure 1.10
Subcuticular closure
1.3 Discussion
Radioguided parathyroidectomy is another potential tool at the disposal of parathyroid surgeons. Because all hospitals often use the technology for sentinel node biopsies, radioguided parathyroidectomy is available to most surgeons. Although we use the Neoprobe® for our procedures, we have had experience with other hand-held probes, and all were sensitive for the detection of hypercellular parathyroids. We and others have previously shown that radioguided techniques are useful in patients with primary, secondary, or tertiary hyperparathyroidism. Furthermore, radioguided parathyroidectomy is effective in many special circumstances.
1.3.1 Sestamibi-Negative Patients
The gamma probe is able to detect high radioactive counts from all enlarged, hyperfunctioning parathyroid glands, including those that do not appear on imaging studies. Parathyroid localization studies such as sestamibi-SPECT, cervical ultrasound, and CT scans will fail to localize an abnormal parathyroid gland in up to 20% of patients with primary hyperparathyroidism. These glands tend to be smaller. Because the gamma probe can be positioned very close to the parathyroid, it can detect radioactive counts with great sensitivity. Abnormal parathyroid glands missed on imaging studies will still take up sestamibi at higher levels than surrounding tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree