Highlights
- •
Stented radical cystectomies had higher major complications ( P = 0.04);
- •
Stentless radical cystectomy was noninferior in UIAS rate;
- •
Stentless radical cystectomy was noninferior in UIAL rate;
- •
Stentless radical cystectomy was noninferior in UTI rate.
ABSTRACT
Purpose
To systematically compare the evidence about surgical outcomes, postoperative complications, and sequelae of Radical cystectomy with urinary diversion with or without stent placement.
Material and Methods
A literature search was performed through PubMed, Scopus®, and Web of Science up to December 2023 in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement. The study protocol was registered in PROSPERO (CRD 42023492384), and the research question was formulated according to the PICOs model. Three comparative studies were identified, 2 randomized and 1 prospective coming from a randomized cohort.
Results
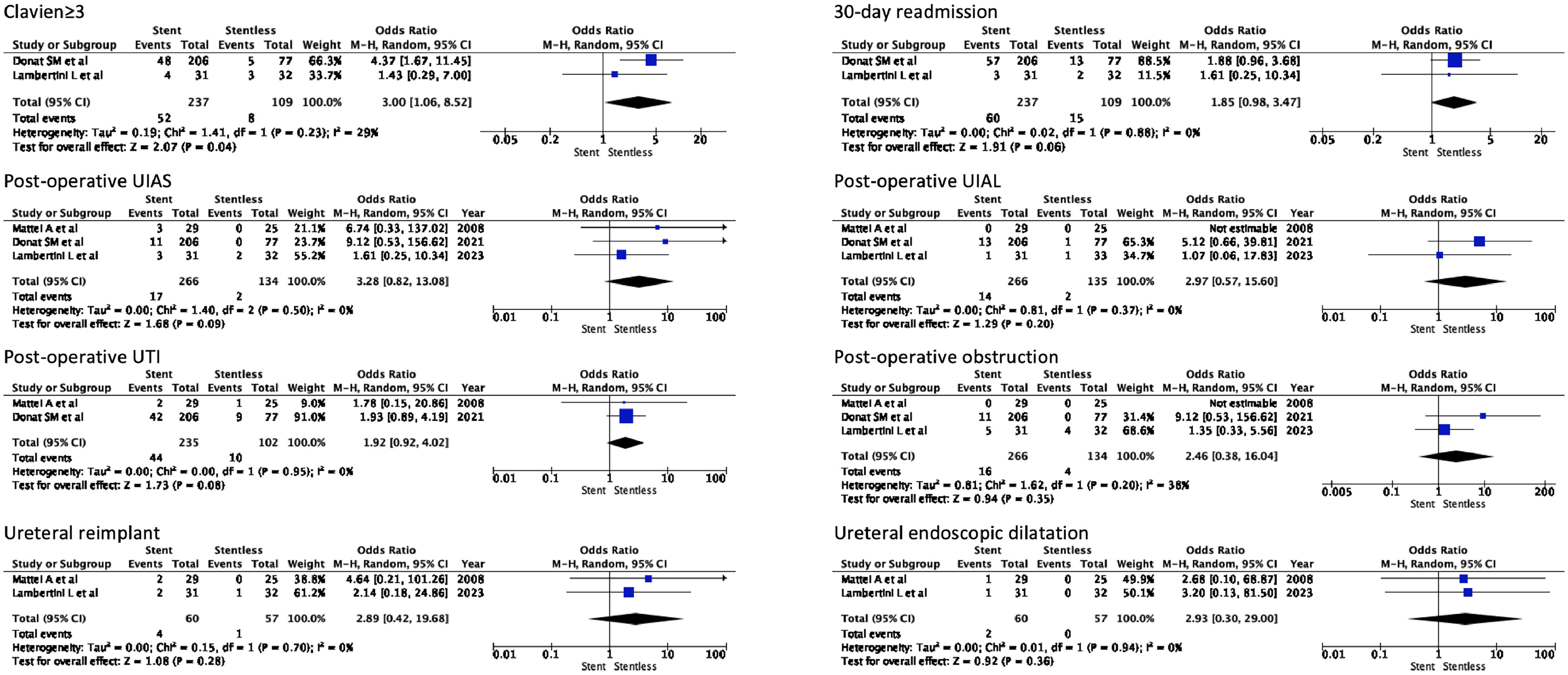
The stent group showed higher odds of postoperative major complications (OR 3.00 – 95%CI 1.06; 8.52; P = 0.04) than the stentless group. There was no statistically significant difference between the 2 groups regarding 30-day readmission ( P = 0.06), postoperative uretero-ileal anastomotis stricture (UIAS) ( P = 0.09), postoperative uretero-ileal anastomotis leak (UIAL) ( P = 0.20), postoperative urinary tract infections (UTIs) ( P = 0.08), and postoperative ureteral obstruction ( P = 0.35). No statistically significant difference between the 2 groups was found regarding UIAS management in terms of ureteral reimplantation ( P = 0.28) or dilatation ( P = 0.36).
Conclusions
Our pooled data analysis shows no statistically significant difference between stentless and stented urinary diversion after radical cystectomy. Stentless could be a reasonable choice when performing diversion during radical cystectomy.
1
Introduction
Radical cystectomy with urinary diversion (RCUD) remains the standard of care for the treatment of very high-risk non—muscle-invasive or muscle-invasive BC [ ]. Both open and minimally invasive approaches can be employed for RCUD. Both systematic reviews [ , ] and randomized controlled trials demonstrated the oncological noninferiority of robotic RCUD [ ]. Moreover, the robot-assisted approach even appears to translate into a statistically significant survival and over 90 days out of the hospital. However, uncertainty remains regarding these findings [ ].
RCUD remains a challenging and demanding procedure that can result in immediate postoperative complications or long-term sequelae, primarily associated with the reconstructive surgical phase. One of the most common sequelae is uretero-ileal anastomosis stricture (UIAS), with an 8%–10% rate, which may result from urine leakage or ureteral vascular impairment [ ]. To mitigate this complication, ureteral stents are usually adopted [ ]. However, as robotic become more widespread, stentless procedures have been shown to be feasible and are gaining popularity [ ].
The evidence regarding the use or omission of stents during RCUD is mainly derived from low-quality, small sample size, nonrandomized, noncomparative studies [ ].
This systematic review and meta-analysis aimed to show the safety of stentless RCUD in relation to postoperative major complications, UIAS and leak (UIAL), and urinary tract infections (UTIs).
2
Material and Methods
2.1
Literature search strategy
The literature search and assessment were independently conducted by 3 authors (D.B.-L.T.- S.C.) through PubMed, Scopus®, and Web of Science up to December 2023.
After establishing the study protocol registered in PROSPERO (CRD 42023492384), the research question was formulated according to the PICOs model: patients with bladder cancer (P) undergoing RCUD with ureteral stent (I) versus without ureteral stent (C) to evaluate major complications, UIAS, UIAL, UTIs, and ureteral obstruction (meant as an acute rise in creatinine, or decreased urine output, or flank pain associated to imaging direct signs of obstruction) (O).
The following string was adopted for comprehensive research:
((((((stent)OR(ureteralstent)OR(ureteralcatheter)OR(stentless))AND(radicalcystectomy))AND(urinarydiver-sion))OR(ilealconduit))OR(neobladder))AND((compli-cation)OR(morbidity)OR(leak)OR(stricture)OR(obstruction)OR(stenosis))AND(bladdercancer)))))).
2.2
Studies selection
The Preferred Reporting Items for Systematic Review and Meta-analysis Statement (PRISMA Statement-www.prisma-statement.org) was followed. After discarding the duplicates, the title, and abstracts were reviewed to limit the assessment to studies that closely aligned with the inclusion criteria. These selected studies then underwent full-text evaluation to confirm their suitability for the meta-analysis. Any discrepancies or uncertainties were solved by consensus by consulting a third experienced reviewer (A.V.). Noncomparative, retrospective, non-English articles, conference abstracts, letters to the Editor, notes, comments, and book chapters were excluded from consideration.
2.3
Publication bias assessment
The Risk of Bias version 2 (RoB version 2) [ ] was used for the risk of bias assessment. One author (F.D.) conducted the evaluation independently, using RoB2 for RCTs and nonrandomized prospective trials. Each domain identified a low, unclear, and high risk of bias. In instances of an unclear risk, confirmation was sought by consulting an experienced author (R.B.).
2.4
Data extraction and analysis
The baseline characteristics [age, gender (male), body mass index (BMI), history of smoking, Charlson Comorbidity Index (CCI) age-adjusted, history of abdominal surgery, and neoadjuvant chemotherapy] and surgical outcomes [estimated blood loss (EBL), operative time (OT), length of stay (LOS), major complications (Clavien ≥3), 30 day readmission, postoperative UIAS, postoperative UIAL, and postoperative urinary tract infection] were extracted.
As only means and standard deviations are permissible for meta-analysis a mathematical model was used to convert either median (range) or median [interquartile range (IQR)] to mean (standard deviation [SD]) [ , ]. The weighted mean difference (WMD) was used as a summary measure for continuous variables, whereas the odds ratio (OR) with 95% confidence interval (CI) was chosen for the dichotomous ones. The Chi 2 test esteemed the heterogeneity among the studies, whereas the I 2 described the percentage of the variability in effect estimates. According to Cochrane Library, the heterogeneity was considered as follows:
- •
0% to 40%: might not be important;
- •
30% to 60%: may represent moderate heterogeneity;
- •
50% to 90%: may represent substantial heterogeneity;
- •
75% to 100%: considerable heterogeneity.
A random-effect meta-analysis was performed to incorporate heterogeneity among the studies. All statistical analyses were performed using Review Manager ([RevMan] [Computer program]. Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
3
Results
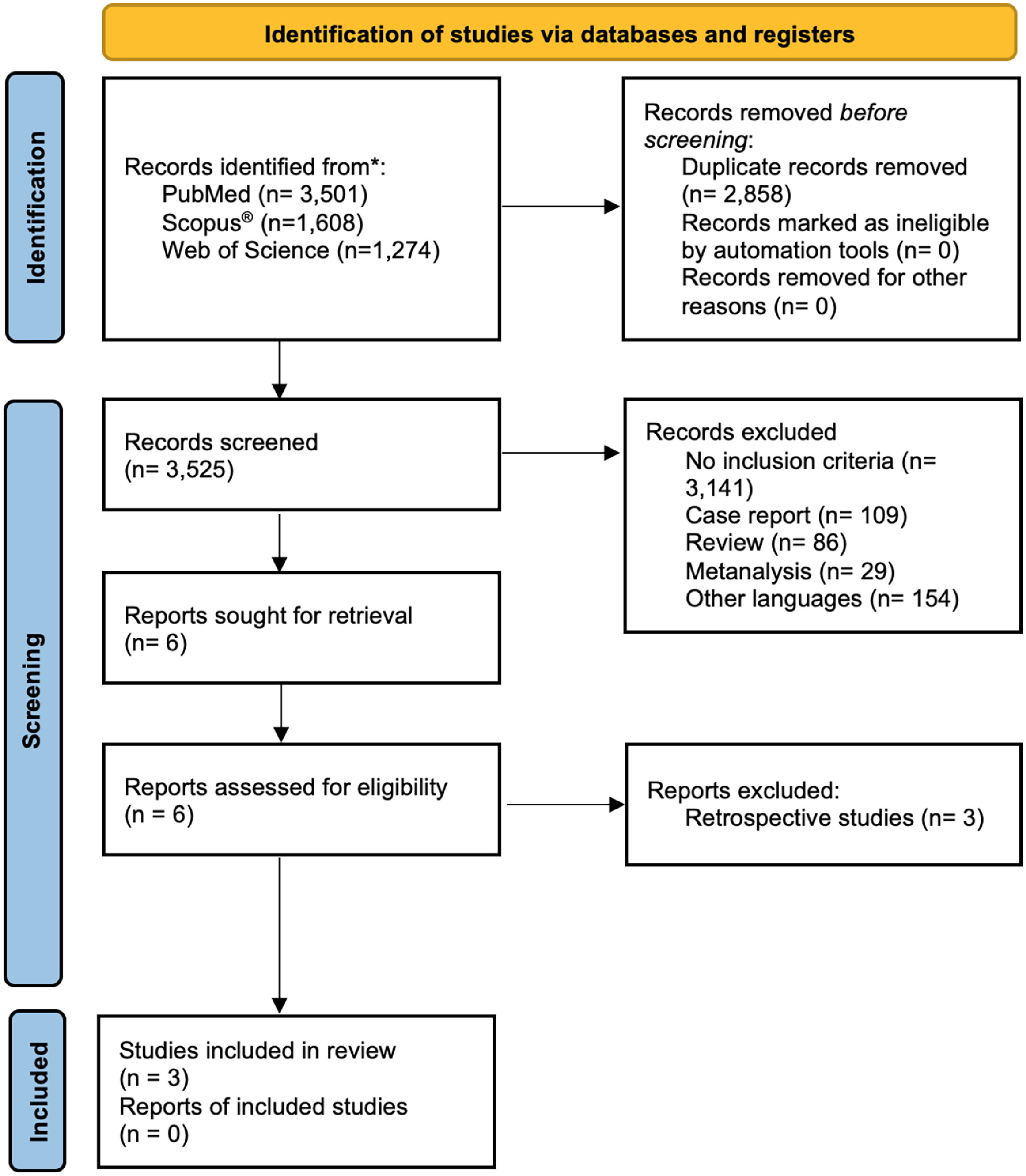
Overall, 6,384 studies were retrieved after querying online datasets. Among these, 6,377 were discarded for various reasons ( Fig. 1 ), whereas 6 showed suitability for the final analysis [ , ]. Following full-text assessment, 3 studies were eligible for final meta-analysis [ , , ], while the other 3 [ ] were excluded due to their retrospective nature. Among the included ones, 2 were RCT [ , ], and 1 prospective study originated from a RCT [ ] ( Supplementary Table 1 – Fig. 1 ).
3.1
Baseline features
The patients in the stent group were younger (WMD -2.85 years, 95%CI -5.21; 0.49, P = 0.02), but less likely to undergo neoadjuvant chemotherapy (OR 0.59, 95%CI 0.37; 0.95, P = 0.03). No statistically significant differences were found in terms of gender (male), BMI, history of smoking, CCI age-adjusted, and history of abdominal surgery. Excluding BMI (I 2 = 73%) and CCI age-adjusted (I 2 = 88), heterogeneity among studies for the other variables was low. All baseline features are summarized in Supplementary Table 2 .
3.2
Surgical outcomes
There was no statistically significant difference between the stent and the stentless group in terms of EBL (100.34 ml, 95%CI -62.98; 263.66, P = 0.23), OT (-1.81 min, 95%CI -77.71; 74.10, P = 0.96), and LOS (1.15 days, 95%CI -0.94; 3.24, P = 0.28). A high level of heterogeneity was found for each outcome measure.
3.3
Postoperative complications and sequelae
The stent group showed higher odds of postoperative major complications (OR 3.00, 95%CI 1.06; 8.52; P = 0.04) than the stentless group. There was no statistically significant difference between the 2 groups regarding 30-day readmission ( P = 0.06), postoperative UIAS ( P = 0.09), postoperative UIAL ( P = 0.20), postoperative urinary tract infection ( P = 0.08), and postoperative ureteral obstruction ( P = 0.35). No statistically significant difference between the 2 groups was found regarding UIAS management in terms of ureteral reimplantation ( P = 0.28) or dilatation ( P = 0.36). A low level of heterogeneity was registered for all the outcome measures ( Fig. 2 ).