Radiation therapy is an effective treatment for newly diagnosed prostate cancer, salvage treatment, or for palliation of advanced disease. Herein we briefly discuss the indications, results, and complications associated with brachytherapy and external beam radiotherapy, when used as monotherapy and in combination with each other or androgen deprivation.
Key points
- •
Choice of definitive radiation modality (eg, brachytherapy, external beam radiotherapy, use of concurrent androgen suppression) is tailored to the “risk” categorization using clinical characteristics.
- •
Postoperative prostate bed radiotherapy improves overall survival for patients with adverse pathologic features.
- •
Radiotherapy, either through x-ray or radiopharmaceutical, is a very effective palliative treatment for bony metastases.
Introduction
Prostate cancer is the most common cancer diagnosis in men after skin cancer, with more than 240,000 estimated cases in 2012. It is also the second leading cause of cancer death in men (28,000 estimated for 2012). Most prostate cancers are diagnosed at an early stage, allowing for the high rate of success with localized treatment. Between 30% and 45% of men receive radiation as their primary treatment for prostate cancer depending on their age at diagnosis.
Both external beam radiotherapy (EBRT) and brachytherapy can be used for the treatment of prostate cancer. The differences and roles of these 2 techniques rely on the physical properties of the radiation and its delivery method. In this article, we review the role of radiation in definitive management, salvage treatment, and palliation for prostate cancer. Although this review is by necessity a brief overview of the extensive literature regarding the use of radiation in prostate cancer management, we rely primarily on “gold standard” clinical trials as well as other reports that offer key findings.
Introduction
Prostate cancer is the most common cancer diagnosis in men after skin cancer, with more than 240,000 estimated cases in 2012. It is also the second leading cause of cancer death in men (28,000 estimated for 2012). Most prostate cancers are diagnosed at an early stage, allowing for the high rate of success with localized treatment. Between 30% and 45% of men receive radiation as their primary treatment for prostate cancer depending on their age at diagnosis.
Both external beam radiotherapy (EBRT) and brachytherapy can be used for the treatment of prostate cancer. The differences and roles of these 2 techniques rely on the physical properties of the radiation and its delivery method. In this article, we review the role of radiation in definitive management, salvage treatment, and palliation for prostate cancer. Although this review is by necessity a brief overview of the extensive literature regarding the use of radiation in prostate cancer management, we rely primarily on “gold standard” clinical trials as well as other reports that offer key findings.
Radiation as definitive management
Brachytherapy
“Brachy” is Greek for “short,” and brachytherapy is thus a general term for the placement of a radioactive source into or near a tumor. The radioactive sources chosen for brachytherapy typically have a very short effective dose range, allowing for normal tissue sparing. For prostate cancer, either permanent radioactive seeds are placed within the prostate to deliver their dose over weeks to months (“low dose rate” or LDR), or temporary hollow catheters are placed within the prostate allowing for movement of a single source through the catheters delivering the prescribed dose within minutes (“high dose rate” or HDR).
Brachytherapy as monotherapy is most effective in low-risk prostate cancer, commonly defined using National Comprehensive Cancer Network criteria ( Table 1 ). Other eligibility criteria include (1) prostate size smaller than 60 mL, (2) none to mild urinary obstructive symptoms (International Prostate Symptom Score of 18 or less), and (3) no history of previous pelvic radiotherapy or transurethral resection of the prostate.
| Low Risk | Intermediate Risk | High Risk |
|---|---|---|
| T1-T2a | T2b-c | T3-4 |
| GS ≤6 | GS 7 | GS 8–10 |
| PSA <10 ng/mL | PSA 10–20 ng/mL | PSA >20 ng/mL |
Sources
LDR sources in use include Iodine-125, Palladium-103, and Cesium-131. HDR brachytherapy uses Iridium-192. Half-life, energy characteristics, and prescription doses are described in Table 2 . The dose varies by source because the biologic response of prostate cancer cells and normal tissues varies based on the dose delivery rate.
| Source | Half-life, d | Energy, kV | Definitive Dose | Dose with 40–50 Gy EBRT |
|---|---|---|---|---|
| Iodine-125 (LDR) | 60 | 27 | 145 Gy | 110 Gy |
| Palladium-103 (LDR) | 17 | 23 | 125 Gy | 90–100 Gy |
| Cesium-131 (LDR) | 10 | 29 | 1115 Gy (LDR) | 85 Gy |
| Iridium-192 (HDR) | n/a | 380 | 10.5 Gy × 3 9.5 Gy × 4 | 15 Gy × 1 8.5–10.5 Gy × 2 7.5 Gy × 3 5 Gy × 4 |
Procedure
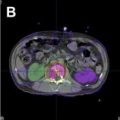
Brachytherapy planning, whether LDR or HDR, requires 3-dimensional (3-D) understanding of prostate size and shape, typically based on serial axial transrectal ultrasound images. Seed (or iridium source “dwell”) locations are designed to provide coverage of the prostate and 2 to 3 mm of extraprostatic tissue while partially sparing the urethra. Fig. 1 depicts a single axial level of an LDR plan with isodose curves depicting the predicted prostate coverage based on seed placement.
Once a plan has been approved as providing appropriate prostate coverage and minimizing urethral and rectal dose, the seeds (or catheters) are placed into the prostate under imaging guidance. This is performed under anesthesia in the lithotomy position, with placement needles entering through the perineum guided by transrectal ultrasound visualization. For LDR, seed placement can be observed in real time, and if necessary, later seeds adjusted as needed to improve prostate coverage. If HDR is being performed, once all catheters are in place, the plan is confirmed and adjusted based on the actual catheter location in the prostate. Then the Iridium-192 source is robotically advanced sequentially into each catheter, remaining at a given “dwell” position for the amount of time calculated in the plan. HDR treatment can be given as a single fraction or repeated fractions over 24 to 40 hours. Recovery is straightforward, although some men develop prostatic edema requiring Foley catheter placement for 24 to 72 hours. Posttreatment imaging is required of LDR treatment to document adequate seed position.
Results
Because implantation of the periprostatic tissue is difficult, brachytherapy is most efficacious in low-risk prostate cancer, although it has been used successfully in cancers more likely to have extraprostatic spread when combined with EBRT. The cumulative rates of biochemical recurrence, local failure, distant failure, and overall survival at 8 years were 8%, 6%, 1%, and 88% in a national cooperative group trial of LDR brachytherapy for low-risk prostate cancer. A Radiation Therapy Oncology Group trial of combination brachytherapy and external beam radiation for higher-risk patients has reported 8-year biochemical recurrence rates of 18%.
As stated previously, acute toxicity includes irritative symptoms of the bladder and rectum, which can be managed with alpha blockade, phenazopyridine, and topical hydrocortisone. Rarely, urinary retention can occur, requiring temporary Foley catheter placement. Late toxicity most commonly involves radiation proctitis and/or urethral stricture. Long-term follow-up of LDR brachytherapy studies described actuarial grade 2+ bladder and rectal late toxicity rates of 25% to 30% and 5% to 7% at 5 years. Rectal fistula development is a severe but extremely rare side effect of prostate radiotherapy (<1%) that is most likely when brachytherapy and external beam radiation are combined. One potential advantage of brachytherapy is that reported rates of erectile dysfunction (ED) are lower in brachytherapy, although this may be confounded by other inequalities between brachytherapy and external beam radiation.
EBRT
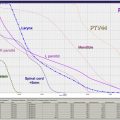
EBRT most commonly uses megavoltage (4–20 MV) photon therapy generated by linear accelerators, although it can also be delivered by protons generated by a particle accelerator ( Fig. 2 ). It is used as monotherapy for low-risk prostate cancer, in conjunction with androgen deprivation and/or brachytherapy for intermediate-risk and high-risk cancers, and after prostatectomy for patients with high-risk features or a detectable prostate-specific antigen (PSA).
Dose and schedule
For definitive management of prostate cancer, dose escalation to doses higher than 75 Gy has been found to improve biochemical control for all risk categories in multiple randomized trials and a large meta-analysis. These doses are delivered in 1.8-Gy to 2.0-Gy fractions delivered daily over 8 to 9 weeks.
More recently, hypofractionated regimens have been evaluated, with either moderate hypofractionation (4–5 weeks of daily treatment) or extreme hypofractionation, or stereotactic body radiotherapy, which consists of 4 to 7 treatments over 1 to 2 weeks. Older studies found mixed results, although they used standard fractionation doses lower than contemporary standards. A more recent randomized trial compared 80 Gy in 40 fractions over 8 weeks versus 62 Gy in 20 fractions over 5 weeks. Reported 5-year freedom from biochemical failure was 85% in the hypofractionated arm compared with 79% in the conventional arm ( P = .065); 3-year genitourinary (GU) and gastrointestinal (GI) toxicity were 16% and 17%, and not statistically different from the conventional fractionation arm. Other moderate hypofractionation trials are pending full results. Extreme hypofractionation cohort studies are promising, but the duration of follow-up is short. The reported rates of biochemical progression-free survival are 90% to 95% at 3 to 5 years.
Procedure
Intensity modulated radiotherapy (IMRT) is the photon delivery standard of care for definitive radiotherapy of prostate cancer. IMRT treatment plans vary the dose delivered within each treatment field, a characteristic that can be used to create concave treatment plans or escalate dose to certain areas within the target. Therefore IMRT’s advantage over 3-D conformal therapy is the ability to lower dose delivered to normal tissues, even while escalating dose to the prostate. IMRT requires high-quality imaging, computerized planning, and quality assurance testing. In addition, a strategy for target localization is necessary to address prostate motion, because IMRT dose drops sharply outside of the planned target area.
A planning computed tomography (CT) scan with the patient in the treatment position on a table simulating the treatment couch is required for prostate EBRT planning. Pelvic magnetic resonance (MR) images can be useful to guide prostate delineation. If used, fiducial markers are placed in the prostate by transrectal ultrasound guidance before imaging. These markers can be visualized immediately before each daily treatment. Other methods of prostate localization include transabdominal ultrasound imaging, implanted electromagnetic wireless transponders, and soft tissue on-board localization, which involves CT imaging of the prostate on the treatment equipment.
IMRT treatment planning requires delineation of the anatomic regions at risk for disease, an expanded volume that takes into account the potential for set-up and target motion, and avoidance of organs (ie, rectum, bladder, femoral heads, penile bulb, and bowel). Development of the plan involves optimizing 5 to 9 circumferentially placed beams to achieve the minimum and maximum doses prescribed to each structure. Quality assurance is then performed to ensure that the plan can be delivered accurately on the treatment machine.
Proton planning is similar to photons, except that most centers use 2 parallel opposed beams entering laterally. Dose coverage of the target and avoidance structures is again optimized through the treatment-planning software.
Monotherapy
EBRT is most commonly used in older men who wish to avoid or have contraindications to an invasive procedure. Dose-escalated EBRT can be quite effective for low-risk cancer with reported 10-year biochemical relapse-free survival of 80% to 90%. However, men with intermediate-risk or high-risk cancer experience 10-year biochemical relapse-free survival of approximately 65% and 25% respectively when treated with EBRT alone.
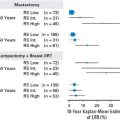
EBRT combined with androgen deprivation therapy
Because of the poor results of EBRT monotherapy in higher-risk prostate cancer, concurrent androgen deprivation therapy (ADT) is used to assist in both radiosensitization and treatment of micrometastatic disease. As shown in multiple randomized controlled trials ( Table 3 ), the addition of androgen deprivation to radiotherapy improves overall survival for both intermediate-risk and low-risk disease. Studies for intermediate disease have evaluated between 3 and 8 months, finding that ADT for at least 6 months provides survival benefit. For high-risk disease, studies have used between 6 months and lifelong ADT; one study comparing 6 months to 3 years found inferior survival with the short ADT arm. Some have reported increased cardiac morbidity with ADT, although other large randomized studies of EBRT with ADT have not corroborated this finding.
| N | Median FU, y | Length of ADT, mo | Results | |
|---|---|---|---|---|
| Intermediate Risk | ||||
| 86–10 | 456 | 12.5 | 0 vs 4 | 36% vs 23% (10-y DSM) |
| D’Amico | 206 | 7.6 | 0 vs 6 | 61% vs 74% (8-y OS) |
| 94–08 | 1979 | 9.1 | 0 vs 4 | 57% vs 62% (10-y OS) |
| High Risk | ||||
| 85–31 | 977 | 7.6 | 0 vs 24 | 39% vs 49% (10-y OS) |
| 92–02 | 1554 | 11.3 | 4 vs 28 | 40% vs 45% a (10-y OS) |
| EORTC 22863 | 415 | 9.1 | 0 vs 36 | 40% vs 58% (10-y OS) |
| EORTC 22961 | 970 | 6.4 | 6 vs 36 | 81% vs 85% (5-y OS) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree