Duct carcinoma in situ (DCIS) is a common but non–life-threatening breast cancer. Four large prospective randomized trials comparing radiation therapy (RT) with none after breast-conservation surgery have all concluded that the use of RT reduces the risk of a local recurrence (LR) in the ipsilateral breast by at least 50%. More information is needed to assess the role of antiestrogen therapy when RT is not given. When markers are validated to predict which patients will have an invasive LR versus another DCIS or no LR, it is hoped that the discussion with the patient will clarify the situation further.
Key points
- •
Assessing the pathology details.
- •
Age and presentation of the patient.
- •
Assessing the patient’s expectations from possible radiation therapy.
Introduction
Duct carcinoma in situ (DCIS) is an early form of breast cancer, which is commonly diagnosed in Western countries with robust screening mammography programs. Of new breast cancers detected through screening, DCIS diagnoses make up 20% to 25% of the total cases.
Women with DCIS have 2 surgical options, simple mastectomy or breast-conservation surgery (BCS). This article focuses on the issue of who benefits from radiation therapy (RT) after BCS. Four large prospective trials have been completed, comparing RT with observation after BCS. The results of the trials are consistent: RT after BCS reduces the risk of an ipsilateral breast cancer recurrence by 50% or more.
So why does the controversy continue about the role of RT in DCIS management? First, the randomized trials also show excellent survival rates, with no differences noted with or without the RT. A University of Michigan study of patients and close family members reported that the benefit of RT in these circumstances is perceived as less important than for invasive carcinomas, which carries both a local control and breast cancer survival benefit from RT.
Second, many physicians also favor the use of no RT in certain subsets of women with DCIS; the several versions of the Van Nuys Prognostic Indices published by Silverstein and colleagues received widespread acclaim. Several studies, both of the registry and the prospective randomized trial design, have opened over the last decade, focused on identifying women who may not benefit from the addition of RT for their DCIS, because their risk of local recurrence (LR) is so low.
Of LR in DCIS studies, about one-half are recurrence of DCIS and one-half are invasive ductal carcinoma. Predictors of which patients are destined to develop the invasive recurrences would enhance decision making regarding the role of RT, but thus far remain the subject of ongoing research.
Introduction
Duct carcinoma in situ (DCIS) is an early form of breast cancer, which is commonly diagnosed in Western countries with robust screening mammography programs. Of new breast cancers detected through screening, DCIS diagnoses make up 20% to 25% of the total cases.
Women with DCIS have 2 surgical options, simple mastectomy or breast-conservation surgery (BCS). This article focuses on the issue of who benefits from radiation therapy (RT) after BCS. Four large prospective trials have been completed, comparing RT with observation after BCS. The results of the trials are consistent: RT after BCS reduces the risk of an ipsilateral breast cancer recurrence by 50% or more.
So why does the controversy continue about the role of RT in DCIS management? First, the randomized trials also show excellent survival rates, with no differences noted with or without the RT. A University of Michigan study of patients and close family members reported that the benefit of RT in these circumstances is perceived as less important than for invasive carcinomas, which carries both a local control and breast cancer survival benefit from RT.
Second, many physicians also favor the use of no RT in certain subsets of women with DCIS; the several versions of the Van Nuys Prognostic Indices published by Silverstein and colleagues received widespread acclaim. Several studies, both of the registry and the prospective randomized trial design, have opened over the last decade, focused on identifying women who may not benefit from the addition of RT for their DCIS, because their risk of local recurrence (LR) is so low.
Of LR in DCIS studies, about one-half are recurrence of DCIS and one-half are invasive ductal carcinoma. Predictors of which patients are destined to develop the invasive recurrences would enhance decision making regarding the role of RT, but thus far remain the subject of ongoing research.
The asymptomatic patient
Most women with DCIS present without any symptoms. The disease is identified either through a screening study such as a mammogram, or as an incidental finding for a biopsy performed for another indication. Some of these women may be at a relatively low risk for LR. Although the addition of radiation lowers the risk of local failure in all subsets of DCIS, some patient subsets, identified by disease characteristics, age at presentation, and other factors, may start out with a relatively low risk for local failure, and may be considered for no RT, because the absolute benefit is so small.
Grade, Size, and Other Disease Factors
Two groups of pathologists were the first to suggest that low-grade DCIS could be treated by excision alone. Both Betsill and Rosen at Memorial Sloan-Kettering Cancer Center (MSKCC) and Page at Vanderbilt retrospectively identified pathology specimens from women that had been signed out as benign but on re-review showed low-grade DCIS. The women had no planned treatment, just the biopsy, and both studies were designed to track down the patients and study the natural history of low-grade DCIS. Page updated the results of the 28 women in his study, with a median interval of 24 years in those who did not develop breast cancer. Fig. 1 shows those results; the risk of developing invasive breast cancer in those women was 9.10 times greater than women in the general population. Page and colleagues discuss offering these women treatment with a wide excision only, processed with the careful attention to details that modern pathology laboratories use. The results of both studies were similar, and contributed to the controversy concerning which patients need RT.
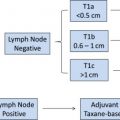
Silverstein and colleagues published their first version of the Van Nuys Prognostic Index in 1996; this scoring system incorporated grade, presence of necrosis, tumor size, and margin width to calculate a score predicting which patients with a diagnosis of DCIS would be at highest risk for recurrence and thus should benefit from whole-breast RT after BCS ( Fig. 2 ). The score was developed from and then tested in the same group of patients, those operated on by Dr Silverstein’s group in Van Nuys, California. RT was used in some but not all cases. In our own pathology material at MSKCC, we attempted to apply the Van Nuys score to recent cases, but had issues primarily because size is not easily calculated in many DCIS cases. But Silverstein’s work was useful as a starting place to define which subsets of DCIS can be identified that may be at very low risk for LR.
Although none of the 4 large prospective trials comparing RT with no RT specifically was designed around the details of pathology subtypes, several of the trials retrospectively looked at pathology and LR. Pathology review of 623 of 814 patients in the NSABP (National Surgical Adjuvant Breast and Bowel Project) B-17 trial was completed for the characteristics shown in Table 1 . The investigators concluded that many of the factors were related, and further multivariant analysis showed that comedo necrosis was the “significant predictor for ipsilateral breast” LR. But the investigators observed a benefit for RT in each risk group, including the lowest-risk groups.
| Variable | Lumpectomy | Lumpectomy and Radiotherapy | All Patients |
|---|---|---|---|
| Randomized | 405 | 413 | 818 |
| Ineligible | 6 | 12 | 18 |
| No follow-up | 2 | 2 | 4 |
| Patients included in analysis | 403 | 411 | 814 |
The similar European Organisation for Research and Treatment of Cancer (EORTC) DCIS trial also performed a central pathology review of most of the women enrolled in the trial. Table 2 shows the hazard ratios in the various pathology subsets, with well-differentiated histology, clinging or micropapillary architecture, and free margins all associated with the lowest risk of local failure. The randomized treatment arm (ie, RT versus no RT) also was highly significantly associated with risk of LR. The investigators stated that although RT benefited all subsets, in the well-differentiated DCIS with clinging or micropapillary growth, the LR at 10 years was less than 10%, and thus the absolute benefit for the RT was small.
| Variable | Hazard Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age (y) | |||
| >40 | 1 | ||
| ≤40 | 1.89 | 1.12–3.19 | .026 |
| Method of detection | |||
| Radiograph finding only | 1 | ||
| Clinical symptoms | 1.55 | 1.11–2.16 | .012 |
| Histologic type | |||
| Well | 1 | ||
| Intermediate | 1.85 | 1.18–2.90 | .024 |
| Poor | 1.61 | 0.93–2.79 | |
| Architecture | |||
| Clinging/micropapillary | 1 | ||
| Cribriform | 2.39 | 1.41–4.03 | .002 |
| Solid/comedo | 2.25 | 1.21–4.18 | |
| Margins | |||
| Free | 1 | ||
| Not free | 1.84 | 1.32–2.56 | .0005 |
| Treatment | |||
| Local excision + radiotherapy | 1 | ||
| Local excision | 1.82 | 1.33–2.49 | .0002 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree