Highlights
- •
Micropapillary Urothelial Carcinoma (MPUC) is associated with poor oncologic outcomes.
- •
Unknown whether greater fraction of MPUC component is prognostically relevant.
- •
Largest ever pathologic review and quantification of MPUC component on TUR samples.
- •
Continuous MPUC % and MPUC ≥ 30% are associated with increased pN+ disease at RC.
- •
Standardized reporting of fraction of MPUC in TUR specimens can aid in treatment selection.
Abstract
Introduction/Background
Micropapillary variant urothelial carcinoma (MPUC) is associated with increased risk of treatment failure with intravesical therapy likely due to the increased risk of occult lymph node (LN) metastasis at radical cystectomy (RC). To date, limited data exists as to whether percent MPUC present within transurethral resection (TUR) samples impacts LN positivity at RC. Our objective is to evaluate the association of percentage MP variant on TUR on incidence of lymph node metastasis and survival outcomes.
Methods
A total of 67 patients with MPUC on TUR were identified from a prospectively maintained database of patients undergoing RC at our institution between 2007 and 2022. TUR samples were rereviewed by an expert GU pathologist with over ten years of experience. Presence and percent MP component, LVI, CIS, grade, and clinical stage were evaluated. Pathologic outcomes were collected from subsequent RC specimens, and recurrence free (RFS) and overall survival (OS) were estimated via the Kaplan–Meier method. Associations between percent MP and lymph node metastasis, RFS, and OS were assessed with univariate and multivariable logistic regression and Cox survival analyses as appropriate.
Results
Thirty four of 67 (51%) patients underwent RC for cT1 disease, the remainder harbored ≥cT2 disease. 19 of 33 (58%) patients with ≥cT2 disease received neoadjuvant chemotherapy (NAC). Mean percent MPUC was 35% in cT1 patients and 28% in cT2 patients ( P = 0.25). On univariate analysis, both MPUC ≥ 30% (Odds Ratio (OR) 3.38, P = 0.02) and clinical ≥T2 (OR 2.88, P = 0.04) were significant predictors of nodal metastasis at RC. On multivariable analysis, MPUC% (OR 1.02, P = 0.036) or MPUC% ≥ 30% (OR 4.01, P = 0.013) and clinical T stage ≥2 (OR 3.73, P = 0.018) were significant predictors of pathologic node positive disease. The lowest rate of LN metastasis was found in patients with cT1 disease and MPUC <30% (3/16, 18.7%), versus the highest in ≥cT2 disease and MP ≥ 30% (12/16, 75%).
Conclusions
Percent MPUC component on TUR is associated with increased risk of occult lymph node metastasis at RC. Routine pathologic evaluation of percent MP component has the potential to help select patients with MPUC that might be reasonable candidates for intravesical therapy.
1
Introduction
Micropapillary urothelial carcinoma (MPUC) is a rare variant of bladder cancer demonstrating aggressive behavior. MPUC is significantly more likely to present at a locally advanced stage and demonstrates a high incidence of occult nodal metastasis in clinical tumor stage 1 (cT1) disease when compared with nonvariant urothelial carcinoma (UC) [ ]. Because of this highly aggressive behavior, management of nonmuscle invasive MPUC presents a dilemma for Urologists aiming to balance oncologic control while minimizing treatment morbidity. Some studies have demonstrated superior oncologic outcomes for early radical cystectomy (RC) in clinical T1 MPUC as compared with intravesical bacillus Calmette–Guerin (BCG) therapy [ ]. Other studies have demonstrated acceptable oncologic outcomes with intravesical BCG in MPUC patients [ , ]. Despite ongoing discourse, the most recent clinical guidelines published by the American Urologic Association, National Comprehensive Cancer Network (NCCN), and the European Association of Urology all recommend early RC as either the preferred or equivalent treatment strategy for patients with cT1 MPUC [ ].
Management decision making for patients with cT1 nonmuscle invasive bladder cancer (NMIBC) seeks a proper balance between avoiding both overtreatment (with significant quality of life impact) and undertreatment (with resulting recurrence and/or progression). While the risk of disease progression with induction BCG for nonvariant UC is low [ ], a greater portion of cT1 MPUC patients would be expected to fail this therapy given the approximately 25% incidence of occult nodal metastasis in cT1 disease [ ]. Biomarkers are needed to better risk stratify cT1 MPUC to identify optimal candidates for a bladder-sparing treatment approach.
The degree of micropapillary architecture present within a tumor specimen has been recognized as a potential prognostic marker within other solid organ malignancies [ ]. Data in bladder cancer are limited, with a prior study of 36 patients with MPUC finding no association between the extent of micropapillary component and oncologic outcomes [ ]. Our objective is to identify whether the percent MP component within transurethral resection (TUR) samples is associated with occult nodal metastasis at RC and oncologic outcomes in patients with MPUC.
2
Methods
2.1
Study design and study population
We retrospectively analyzed a prospectively maintained database of all patients undergoing RC at our institution between 2007 and 2022. Patients with clinical stage T1 or higher MPUC, with appropriate preoperative staging imaging, that subsequently underwent subsequent RC were included. Patients were excluded if they had evidence of distant metastatic disease at time of diagnosis, or if pathology slides were unavailable for evaluation. All TUR samples containing reported MPUC were re-reviewed by an expert GU pathologist with over ten years of experience (RA) for the presence and quantity of MPUC, histologic grade, clinical stage, and presence of lymphovascular invasion (LVI) or carcinoma in situ (CIS). Quantity of MPUC was calculated as a percent (1–100) of the total urothelial carcinoma present.
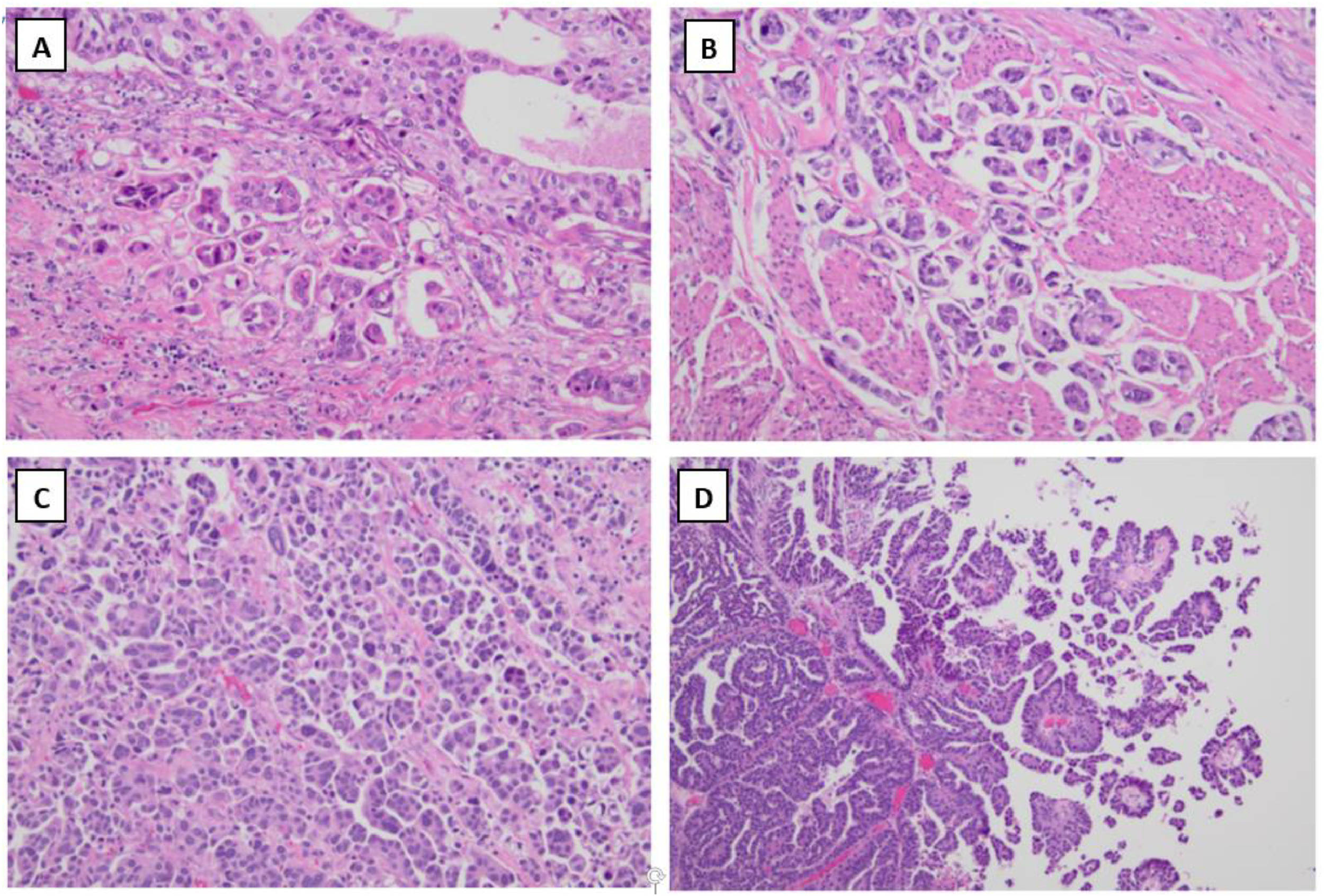
Histologically, MPUC is defined by the presence of small clusters of tumor cells without fibrovascular cores, often surrounded by lacunae (mimicking vascular invasion) ( Fig. 1 A–B). Multiple clusters within the same lacuna can often be present ( Fig. 1 C). The tumor cells also tend to have peripherally oriented nuclei with occasional cytoplasmic vacuoles. Unlike MPUC, high-grade papillary urothelial carcinoma demonstrates complex papillary architecture, composed of papillae with fibrovascular core lined by atypical and pleomorphic nuclei ( Fig. 1 D).
2.2
Study outcomes
The primary goal of the study was to evaluate for association between quantity of MPUC and pathological outcomes at RC and overall survival (OS). Primary pathologic outcomes of interest included locally advanced disease at time of RC (defined as ≥ pathologic T stage 3 (pT3)), and pathologically node positive disease (pN+). OS was calculated from the date of RC to the date of death or the date of last clinical contact for patients who remained alive at last follow up. Secondary outcomes included the rates of upstaging at RC, and recurrence free survival (RFS).
2.3
Statistical analysis
Clinical, demographic, and oncologic parameters were evaluated as potential predictors for the above-mentioned outcomes. Univariate associations were evaluated using chi-squared test for categorical measures and t-test for continuous measures. Proportions of patients with pN+ and pT3+ stage were calculated. The Kaplan–Meier method was used to estimate unadjusted RFS and OS probability. For the binary outcomes of pT3+ and pN+, we fit univariate and multivariable logistic regression models and values for odds ratios (OR) and confidence intervals (95% CI) were reported. Univariate and multivariable Cox proportional hazard models were fit to assess for association between MP quantity and RFS and OS with hazard ratio (HR) and 95% CI reported. Quantity of MPUC was evaluated as a continuous variable, where necessary a restricted cubic spline with 3 knots were applied to model nonlinear association, and dichotomized around the cohort median value of 30% (<30% vs. ≥ 30%) to allow for ease of interpretation. Partial effect of MPUC in a multivariable Cox model was assessed with other covariates help at the mean values. All statistical tests were 2-sided with significance set at 0.05, and statistical analysis was performed with R version 4.2.1 (r-project.org).
3
Results
A total of 70 patients were identified who underwent RC following a TUR that contained MPUC on the original pathology report. Upon pathologic re-review, a total of 67 of 70 (95.7%) were confirmed to contain MPUC. 13 of 67 (19.4%) patients with MPUC also had other variants histology, including 6 lipid-rich, 3 glandular, 3 squamous, and 1 plasmacytoid. Refer to Table 1 for baseline clinical and demographic characteristics of the cohort. The 34 (50.6%) patients underwent RC for cT1, the remainder harbored ≥cT2 disease (31 with cT2, 2 with cT4a). Three patients met size criteria for clinical node positive disease on cross sectional imaging prior to RC. One was cN2 and 2 were cN1. 19 of 33 (57.6%) patients with ≥cT2 disease received neoadjuvant chemotherapy (NAC) prior to RC. Mean quantity MPUC was 34.7% in cT1 patients and 27.6% in cT2 patients ( P = 0.25). At radical cystectomy, 23 patients (34%) had ≥pT3 disease, and 28 (42%) harbored pN+ disease. Twenty-six patients (39%) were upstaged at RC, including 10 of 34 (29%) with initial cT1 disease and 16 of 33 (49%) with ≥cT2 disease.
| Variable | No./mean | %/SD |
|---|---|---|
| Total Patients | 67 | 100% |
| Male | 56 | 83.6% |
| Age (years) | 74.2 | 9.6 |
| Clinical T Stage | ||
| cT1 | 34 | 50.7% |
| cT2+ | 33 | 49.3% |
| MPUC quantity (%) | 31 | 25 |
| CIS | 21 | 31.3% |
| LVI | 15 | 22.4% |
| Additional variant histology | 14 | 20.9% |
| Neoadjuvant therapy | 21 | 31.3% |
| Gemcitabine + cisplatin | 14 | 20.9% |
| MVAC | 3 | 4.5% |
| Other/trial | 4 | 6.0% |
| Pathologic T stage | ||
| pTX (intravascular only) | 1 | 1.5% |
| pT0 (ypT0 = 4) | 8 | 11.9% |
| pTis (ypTis = 1) | 10 | 14.9% |
| pT1 (ypT1 = 2) | 9 | 13.4% |
| pT2 (ypT2 = 6) | 16 | 23.9% |
| pT3 (ypT3 = 7) | 17 | 25.4% |
| pT4 (ypT4 = 1) | 6 | 9.0% |
| Total pT3+ | 23 | 34.3% |
| Pathologic N stage | ||
| pN0 | 39 | 58.2% |
| pN1 | 6 | 9.0% |
| pN2 | 18 | 26.9% |
| pN3 | 4 | 6.0% |
| Total pN+ | 28 | 41.8% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree