Activity type
Considerations
Reagent preparation
1.
Perform in cleanest environment
2.
Store working stock solutions in single-use aliquots
3.
Quality control each new set of reagents before use in clinical testing; use low copy number sample for sensitivity evaluation
4.
Preparation of master mixes reduces variability and errors
Specimen collection
1.
Establish acceptable tolerance limits for each specimen type to be tested (e.g., storage temperature, transport time, anticoagulant)
2.
Distribute protocols for proper specimen handling to all potential users
3.
Capture clinical and analytical information on requisition
Specimen processing
1.
Specimen must be received and stored in preamplification (clean) laboratory
2.
Develop guidelines to ensure against specimen mixup and to preserve integrity of target sequence
Analysis of specimen
a. Extraction procedure
1.
Evaluate extraction procedures for presence of inhibitors and factors that decrease yield of target
2.
Internal control added to the sample at the time of extraction to determine false-negative reactions due to inhibitors or determine this rate by some other means. If an internal control is not to be evaluated with each patient sample, then the rate of false-negative reactions should be stated on the report in a disclaimer in case of negative results
b. Assay setup, amplification, and detection
1.
Optimize concentration of primers, magnesium chloride (MgCl2), deoxynucleotide triphosphates (dNTPs); volume; cycling conditions and detection system
2.
Develop guidelines to minimize possibility of contamination by template nucleic acid or amplicon (see sections on quality control)
3.
Control specimens must be processed in the same manner as patient specimens
4.
Develop guidelines to set up assay to avoid cross-contamination of specimens and controls
Interpretation and report
1.
Develop guidelines for interpretation and report
2.
Interpretation should be performed by at least two individuals independently
3.
Develop guidelines for report distribution
Preanalytical Phase
As part of the preanalytical phase, special attention should be given to specimen collection, transport, and storage, because specimen handling often affects the results. Test results that could influence treatment decisions should reflect the patient status and not specimen mishandling [4, 9].
Some of the preanalytical challenges pose by this new technology is that multiple medical disciplines (surgery, oncology, or pathology) may request the molecular test to define treatment strategy for each patient. Most institutions now have tumor boards where test utilization and treatment decisions are discussed. It is important to ensure that the test request is made appropriately, and that every patient that needs a test is offered the test in a timely manner. This is one of the most difficult aspects of managing a molecular pathology laboratory. A way to manage these challenges might be providing automatic reflex testing by pathologists based on the diagnosis and tissue availability within the pathology department, particularly if the number of patients that require testing continues to grow in volume and complexity.
The molecular pathology laboratory has to be able to handle multiple sample types. This raises a number of challenges when the needs for molecular analysis are included within a diagnostic pathway. Laboratory issues specific for hematopoietic neoplasms and solid tumor testing include the need for fresh or frozen tissue for RNA-based testing, the use of microdissection to reduce nonmalignant cell population in the specimens, and the need to work with small tissue specimens such as needle biopsies. The majority of diagnostic biopsies are small and are rapidly fixed when placed in buffered formalin, but larger surgical specimens require controlled fixation. It is probably optimal for the fixation process to be controlled by the pathology laboratory. Cytology samples should be hanlded with the same care. In some centers pathologists are involved in performing fine needle aspirations, which aids in handling of the sample. Cytology fixation is usually done in an alcoholic fixative, which preserves nucleic acids relatively intact. This renders the samples suitable for most molecular analyses.
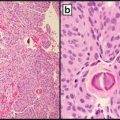
As tissue samples go through macroscopic examination and cut up stage, blocks are taken and placed in bar coded plastic cassettes for processing. Vacuum and microwave processors are temperature controlled devices that ensure excellent penetration of graded alcohols and xylene substitutes, allowing paraffin embedding. There are many challenges typically for molecular pathology diagnostics of solid tumors. The vast majority of the DNA and RNA to be analyzed is retrieved from routine formalin-fixed, paraffin-embedded tissue, which leads to suboptimal DNA quality for the required assays due to fixation and histo processing procedures. For the design of molecular test it should be taken into account that suboptimal DNA samples allow only amplification of small sized PCR amplicons (100–200 bp). In addition, the DNA isolated from dissected tissue fragments composed of mixed populations of normal and neoplastic cells reducing the mutant allele frequency, and frequently only a limited amount of tissues is available containing a low percentage of neoplastic cells, therefore, the test developed must be able to accurately detect low levels of mutations. The use of previously frozen tissue as well a decalcified tissue is not advisable as recovery of amplifiable DNA or RNA is severely diminished. Histopathological diagnosis is made from sections of paraffin blocks at 4–6 μm. It is imperative for molecular testing to take strict precautions to prevent cross contamination between samples. It is best practice to replace the blades regularly and even between cases. Additionally, disposable plasticware should be used to transfer sections to glass slides. A critical element of the success of he molecular testing of the tissue samples is for a pathologist to mark the area of the section containing neoplasia on the H and E slide at the time of the diagnosis for macrodissection or microdissection, if used. It might be necessary to mark multiple areas of the neoplasia for manual microdissection to account for tissue heterogeneity of neoplastic cell content within large tumors. Furthermore, the histopathologist should estimate the percentage of neoplastic cells present in the sample selected for DNA/RNA extraction and this should be present in the pathology report. This estimation can be important in determining success or failure of subsequent testing as it may define the lower limit of detection and the minimum percentage of neoplastic cells that needs to be present for many tests.
Widely dispersed neoplastic cells within a specimen is notorious example in which a low percentage of tumor cells in the specimen can produce false negative results. Presence of necrosis in the tissue for examination should be noted and avoided if possible for molecular testing.
Analytical Phase
Assay Design and Development
A well thought out process for assay design and development is critical to ensure the success of a new test development and implementation. Once specific analytes, assay techniques, and specimen types have been identified, the assay design and development can begin. The first task is to optimize each step of the analytical process, which includes nucleic acid extraction, target amplification, detection, quantification, and result interpretation. Several review and research articles provide detailed descriptions of the key parameters that may influence the performance of different in vitro nucleic acid methodologies, including standard PCR, both uniplex and multiplex. After optimization of the assay, it is necessary to evaluate and document preanalytical variables that might have an impact on the performance characteristics of the assay. Common preanalytical variables are specimen type, transport, storage and handling, as well as interfering substances such us lipids, hemoglobin, and bilirubin.
Establishment of molecular diagnostic tests, particularly amplification assays, requires development of controls for each step of the testing process, including reagent preparation, specimen collection, specimen aliquoting, and performing the actual assay. A careful selection of control reagents is vital for the correct interpretation of test results. Several types of controls are used throughout the execution of an assay to ensure appropriate performance. For qualitative tests, negative and positive controls are required by CLIA ’88 regulations and must be processed in every clinical test run. Failure to obtain the correct result for any of the controls invalidates the entire test and requires retesting of all samples. Whenever possible, positive and negative control reagents should closely resemble a patient specimen. Furthermore, a positive control should represent a clinically relevant level of the nucleic acid target sequence in a background of negative nucleic acid target sequence. The negative control should contain “background” nucleic acid sequences expected to be present in the patient’s sample. In addition to the negative and positive controls, a blank control should be included with every assay, which contains all the components of the reaction mixture except nucleic acid. In addition to these controls, in some instances it is imperative to include an internal control to check for the presence of inhibitors in the individual patient samples. If the latter control is not used, then when a negative result is obtained, it is not clear whether the absence of amplicon is due to the absence of the target sequence in the patient specimen or to the presence of substances that inhibited the amplification reaction. To avoid this situation, amplification of an internal positive control sequence is recommended. The internal positive control can be an endogenous nucleic acid sequence that is unrelated to the target sequence of the clinical assay but is constitutively present in the sample. Alternatively, it may represent a sequence that is spiked into the clinical sample at some step in the testing process. The former endogenous internal positive control generally requires a separate set of primers and may require a separate reaction. The spiked control is generally a sequence that shares the same primer sequence that is used for the clinical target and is usually amplified in the same reaction tube as the clinical sample. As is the case with the external clinical positive control, the internal control should be used at a concentration that is relevant to the clinical testing process. The internal positive controls are also valuable to assess the presence of amplifiable nucleic acid and the absence of inhibitors, as well as to assess that the amplification and detection reactions are performed according to the specifications.
The use of a series of positive controls at different concentrations of target sequence can be helpful in monitoring the assay for changes in sensitivity over time. In addition, inclusion of a positive control where the concentration of target sequence is below the detection threshold of the assay can be useful for detecting low levels of amplicon.
A common approach to developing internal controls is to create synthetic materials, such as in vitro synthesized plasmids or fragments of DNA, that can be spiked into the specimen before testing. In addition, this internal control can be used for internal calibration. An internal calibrator contains a determined amount of this modified target that can be added directly to a clinical specimen and undergoes the same manipulation as the target of the patient specimen. One caveat for internal controls is that they must have the same or a very similar efficiency of amplification. Moreover, when the internal control fails to be detected, it is not possible to determine whether an inhibitor is present or there is an amplification problem. It is important to use a low amount of the internal control to avoid competition with the target of the patient specimen. When detecting and/or quantifying RNA from tissue or cells, amplification of a housekeeping gene (e.g., GAPDH, β-actin) can be used as an internal control. Most housekeeping genes are highly abundant and might not be the most appropriate internal control. The use of RNA from a gene with the same approximate abundance as the target sequence should be used.
New Test Verification/Validation
As with any other area of the clinical laboratory, the introduction of a new test requires proper validation. There are major differences between the implementation of an FDA-approved test and one that is not. CLIA ’88 provides specific guidance for validation of these assays. Laboratories implementing FDA-approved tests must verify and document the performance characteristics of the test for the indications for use in populations similar to those in which the manufacturer has established performance. Implementation of in-house developed assays requires a more involved process, with extensive documentation on test performance and QC programs that ensure reproducible performance of the test.
Verification of a new test is a complex process that can be divided into two phases: analytical and clinical verification. Analytical verification provides information about the analytical performance of the test. Clinical verification provides information about the clinical utility of the test with regard to the intended use. Determination of the intended use provides information about the appropriate settings, including disease states and populations for which the test can be useful. In this context, the phrase, intended use refers to the DNA or RNA target that a molecular assay detects or quantifies, whereas indications for use refers to the clinical syndrome/condition for which the assay can be used for diagnosis, management, or monitoring of disease [4, 6, 9].
Analytical Verification
Before a new or improved test is introduced, careful evaluation of the performance characteristics of the assay under laboratory conditions needs to be done. The analytical verification process provides information regarding the performance of the assay but also can provide practical information needed for daily operation of the test. Historically, analytical validation programs has been challenging because of the lack of standards and reference materials for a many nucleic acid targets. This shortfall has impacted the laboratory’s ability to determine assay sensitivity and accuracy.
As part of the analytical verification, laboratories must determine the assay’s analytical sensitivity, analytical specificity, accuracy, and precision. For quantitative assays, information regarding the linear dynamic range or reportable range determines when a measurement or change in the quantity of the analyte is clinically relevant or due to inherent test error. A number of national and international organizations are taking steps to develop standard reference materials. The National Institute of Standards and Technology developed one of the first nucleic acid standard reference materials for human identity testing and is actively working in the certification of a human genome to be used for Next Generation Sequencing protocols. When standardized reference materials are not available, laboratories must rely on alternatives to validate tests. Laboratories can develop their own reference materials for analytical validation and monitoring daily performance of the assay. These reference materials may be available in-house or from an outside source such as a collaborating laboratory, government agency (CDC, FDA, NIH), or commercial supplier. Examples include cell lines that contain a specific genetic change, plasmids, and intracellular RNA or DNA. When it is difficult to obtain a natural reference material, laboratories develop synthetic reference materials. These synthetic reference materials may be in the form of single- or double-stranded DNA or RNA that is manufactured in vitro and that can be accurately quantified by several physical and/or biochemical methods, misture of different cell lines that contain specific genetic changes of interest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree