11
QUALITY
11.1 THERAPY EQUIPMENT QUALITY ASSURANCE
11.1 THERAPY EQUIPMENT QUALITY ASSURANCE
How frequently is quality assurance (QA) on a linear accelerator (linac) performed?
Question 2
What is the protocol used to perform the absolute output calibration of a linear accelerator (linac)?
Question 3
What are the accepted tolerances for linear accelerator (linac) output deviation measured during daily, monthly, and annual quality assurance (QA)?
Question 4
How strictly are photon and electron beam profile flatness and symmetry required to be maintained?
Linac QA requires daily, monthly, and annual QA procedures, and whenever a repair or change is made that affects the function of the linac.
Answer 2
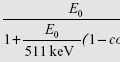
The absolute output calibration of a linac defines the relationship of the radiation dose deposited in the tissue with the output of the machine (measured in arbitrary monitor units [MUs]). The procedure of this calibration in water is performed using the American Association of Physicists in Medicine (AAPM) task group (TG)-51 protocol. The TG-51 protocol prescribes the use of ion chambers and electrometers, which have been calibrated at an accredited dosimetry laboratory in a cobalt-60 beam. The user then uses a conversion factor, kQ, to convert from cobalt-60 to the quality of the beam being calibrated.
Almond PR, et al. AAPM’s TG-51 protocol for clinical reference dosimetry of high-energy photon and electron beams. Med Phys. 1999; 26:1847–1870.
Answer 3
The annual linear accelerator (linac) calibration procedure for photon and electron beams must be performed by a qualified medical physicist and the absolute dose measured in water according to the American Association of Physicists in Medicine (AAPM) task group (TG)-51 protocol must be within 1% of the nominally defined output (typically 1.0 cGy/MU).
The monthly output verification must be within 2% of the nominal defined output for each beam energy. The daily output verification must be within 3% of the nominally defined output for each beam energy.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Answer 4
The constancy checks of photon and electron beam flatness and symmetry in monthly quality assurance (QA) procedure are to be within 1% of the baseline value. The same 1% tolerance is required for annual QA, but a range of field sizes should be checked.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Question 6
How accurate are the treatment couch position indicators required to be?
Question 7
What are the daily quality assurance (QA) procedures performed on a CT simulator?
Question 8
What additional quality assurance (QA) tests are performed monthly and annually on a CT simulator?
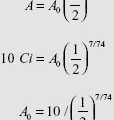
The activity of high-dose-rate brachytherapy sources must be verified by a qualified medical physicist prior to clinical use. Source activity must be measured by using a calibrated well-type ionization chamber and electrometer. Activity of the source must be within 5% of the manufacturer’s specified activity.
Kutcher GJ, et al. Comprehensive QA for radiation oncology: report of AAPM Radiation Therapy Committee Task Group 40. Med Phys. 1994;21:581–618.
Answer 6
Treatment couch position accuracy is very important due to automated positioning controlled by image-guided radiation therapy (IGRT) systems. Couch positioning accuracy is required to be within 2 mm/1° for machines used for conventional treatments, and 1 mm/0.5° for machines used for stereotactic body radiation therapy (SBRT) and stereotactic radiosurgery (SRS) treatments.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Answer 7
According to task group (TG)-66, consistency of the CT number in water, image noise, spatial integrity, and orthogonality of lasers with the imaging plane must be checked daily. Additional checks of the accuracy of laser isocenter marking are common.
Mutic S, et al. Quality assurance for computed-tomography simulators and computed-tomography-simulation process: report of the AAPM Radiation Therapy Committee Task Group No. 66. Med Phys. 2003;30:2762–2792.
According to the American Association of Physicists in Medicine (AAPM) task group (TG)-66, monthly QA includes tests for image quality (such as uniformity, noise, CT number accuracy, contrast, and spatial resolution), mechanical components including table orientation and motion, and safety issues. For annual QA, extra tests include radiation profile, imaging dose, and electron density to Hounsfield unit (HU) calibration.
What are the acceptable criteria for agreement between the light field and radiation field?
Question 10
How often is the electron beam energy required to be verified, and what is its tolerance?
Question 11
What are the daily quality assurance (QA) procedures performed on a high dose rate (HDR) machine?
Question 12
How is a linear accelerator (linac) quality assurance (QA) for a stereotactic body radiation therapy (SBRT)/stereotactic radiosurgery (SRS) machine different from that of a machine used primarily for conventional therapy?
Answer 9
According to the American Association of Physicists in Medicine (AAPM) task group (TG)-142 guidelines, the field sizes defined by the light and radiation should be in agreement within 1 mm or 1% per field side for modern asymmetric jaws.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Answer 10
Each electron beam energy is verified monthly and annually. Electron beam energy is checked monthly by measuring doses at two different depths to spot check the percent depth dose (PDD) of the beam, and must agree within 2% or 2 mm. Annually, electron R50 values are required to be measured to within 1 mm. The electron beam quality specifier, R50, is defined as the depth at which the electron beam percent depth dose is 50% of its maximum.
Almond PR, et al. AAPM’s TG-51 protocol for clinical reference dosimetry of high-energy photon and electron beams. Med Phys. 1999;26:1847–1870.
Answer 11
The daily QA includes checks for timer accuracy, source position accuracy, door interlocks, source exposure indicators, video and intercom system, radiation monitoring system and devices, and control console function.
Wilkinson DA. High dose rate (HDR) brachytherapy quality assurance: a practical guide. Biomed Imaging Interv J. 2006;2:e34.
Answer 12
According to the American Association of Physicists in Medicine (AAPM) task group (TG)-142 guidelines, the tolerance of QA for a linear accelerator (linac) used for SBRT/SRS is more stringent than for a machine used primarily for conventional therapy.
| Procedure | Conventional Tolerance | SBRT/SRS Tolerance |
|---|---|---|
| X-ray monitor units (MU) linearity | ±2% ≥ 5 MU | ±2% ≥ 5 MU, ±5% (2–4 MU) |
| Radiation and mechanical Isocenter coincidence | ±2 mm | ±1 mm |
| Lasers | 1.5–2 mm | 1 mm |
| Collimator size indicator | 2 mm | 1 mm |
| Couch position | 2 mm/1° | 1 mm/0.5° |
| Imaging accuracy | ≤2 mm | ≤1 mm |
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009; 36:4197–4212.
Question 14
How frequent is the quality assurance (QA) performed for cone-beam CT (CBCT) imaging-guidance systems?
Question 15
One qualified radiation therapist did daily output measurement. If the result exceeds the baseline by 5%, what actions should be triggered?
Question 16
How frequently is multileaf collimator (MLC) quality assurance (QA) performed?
Monthly quality assurance (QA) for CBCT system comprises imaging and treatment coordinate coincidence, imaging safety interlocks and imaging quality tests such as geometric distortion, spatial resolution, contrast, Hounsfield unit (HU) constancy, and uniformity and noise.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Answer 14
For linear accelerators (linacs) equipped with CBCT systems, the QA for CBCT imaging verification should be performed daily, monthly, and annually. The daily QA tests the typical image-guided radiation therapy (IGRT) process of imaging and shifting the patient.
Klein EE, et al. Task Group 142 report: quality assurance of medical accelerators. Med Phys. 2009;36:4197–4212.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree