Proximal Tibia Resection with Endoprosthetic Reconstruction
Jacob Bickels
Martin M. Malawer
BACKGROUND
Resection of the proximal tibia includes the removal of one-half to two-thirds of the tibia along with a portion of all muscles that insert on it as well as the entire popliteus muscle, in combination with an extra-articular resection of the proximal tibiofibular joint. The peroneal nerve is preserved.
Of all anatomic locations in which major bone resections and prosthetic reconstructions are done, the proximal tibia is considered to be the site in which surgery is the most complicated, where rates of complications are highest, and whose functional outcome is poorest. The major contributors to these complications include the lack of muscle coverage along the anteromedial aspect of the tibia, the relatively small caliber of the blood vessels around the leg, and the need to include the insertion site of the extensor mechanism with the removed surgical specimen. In the past, these difficulties made it impossible to perform limb-sparing surgery, and above-knee amputations were the only surgical option for malignant tumors at this site.
The limb-sparing technique illustrated in this chapter allows a safe approach to the dissection of popliteal vessels and to the resection and replacement of the proximal one-third to two-thirds of the tibia. Preoperative evaluation of tumor extent requires a detailed understanding of the anatomy and careful evaluation by computed tomography (CT), magnetic resonance (MR) imaging, bone scintigraphy, and biplane angiography.
Types of possible reconstructions include primary arthrodesis, prosthetic replacement, and allograft replacement. We prefer the prosthetic replacements because of the high rates of nonunion and infections associated with allograft reconstruction and the poor function of an arthrodesed knee. The use of a gastrocnemius rotational flap is a key factor in achieving adequate soft tissue coverage of the prosthesis and in restoring function of the extensor mechanism.
ANATOMY
Knee Joint and Cruciate Ligaments
The knee joint is seldom directly invaded by tumors of the proximal tibia. When it does occur, invasion is usually the result of a pathologic fracture, contamination of an improper biopsy technique, or tumor extension along the cruciate ligaments. The presence of hemarthrosis is suggestive of intra-articular disease.
Involvement of the cruciate ligaments is often not determined until the time of surgery, although an MR imaging scan is a reliable means of determining cruciate ligament involvement preoperatively. An extra-articular resection (ie, en bloc resection of the proximal tibia, joint capsule, and femoral condyles) should be considered if nodules are identified on the cruciate ligaments.
Extensor Mechanism
The attachment site of the extensor mechanism at the tibial tuberosity is resected en bloc with the proximal tibia.
Reconstruction of this mechanism is essential for a functioning extremity.
Popliteal Trifurcation
The popliteal artery divides into the anterior tibial artery, the posterior tibial artery, and the peroneal artery at the inferior border of the popliteus muscle. The popliteal trifurcation is actually composed of two bifurcations. The first is found where the anterior tibial artery arises from the popliteal artery, which then continues as the tibioperoneal trunk. The anterior tibial artery is the first branch and arises at the inferior border of the popliteus muscle. The second bifurcation is found where the peroneal artery and the posterior tibial artery arise from the tibioperoneal trunk; thus, this bifurcation is distal to the anterior tibial artery. It is almost always necessary to ligate the anterior tibial artery at the time of resection, whereas the other vessels must be identified before ligation.
A unique and fortuitous anatomic feature is that the popliteus muscle covers the posterior surface of the tibia, which affords an excellent boundary between the posterior soft tissue extension from the tibia and the neurovascular bundle of the lower extremity. This is in contrast to what occurs at the distal femur in which the posterior aspect is covered solely by the popliteal fat.
Tibiofibular Joint
The proximal tibiofibular joint is located close to the posterolateral aspect of the proximal tibia. Histologic studies show that tumors involving the proximal tibia have a high incidence of extension and involvement of the periscapular tissues of the tibiofibular joint.
To obtain a satisfactory surgical margin while performing a resection of the proximal tumor, it is necessary to remove this joint en bloc, that is, perform an extra-articular resection. This is routine procedure for all high-grade sarcomas of the proximal tibia.
Subcutaneous Location of the Tibia
The entire medial aspect of the tibia lies in a subcutaneous location and remains there after resection and reconstruction approaches had been carried out. This had been a major source of primary and secondary infections, which, in turn, frequently necessitated above-knee amputation.
Today, the routine transfer of the medial gastrocnemius muscle anteriorly to cover the prosthesis is considered a reliable method of prosthetic coverage. It also provides a method of extensor mechanism reconstruction. It is a simple and reliable means of decreasing the incidence of infection, flap necrosis, and secondary amputation.4
INDICATIONS AND CONTRAINDICATIONS
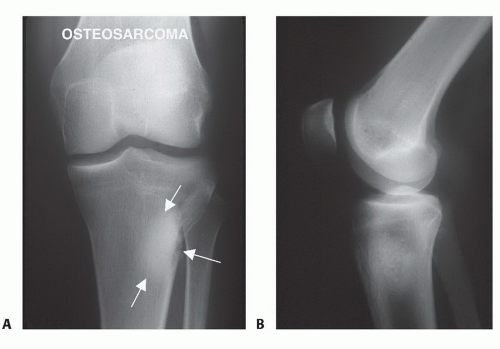
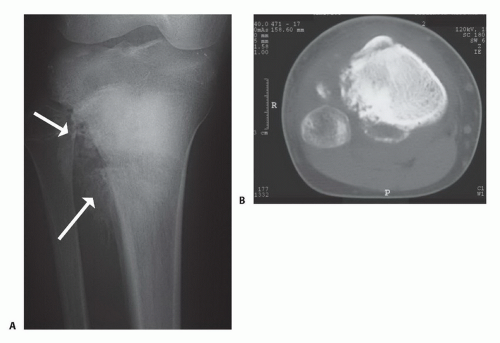
Primary bone sarcomas of the proximal tibia (FIG 1)
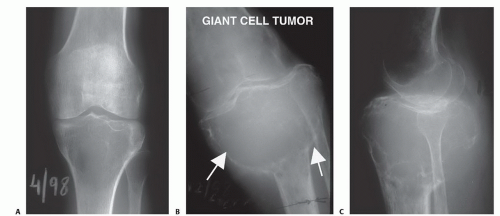
Benign aggressive tumors associated with extensive bone destruction (FIG 2)
Metastatic tumors associated with extensive bone destruction
The major contraindications to limb sparing are neurovascular involvement and compromise as well as extensive soft tissue tumor involvement that precludes adequate prosthetic coverage.
IMAGING AND OTHER STAGING STUDIES
Computed Tomography and Magnetic Resonance Imaging
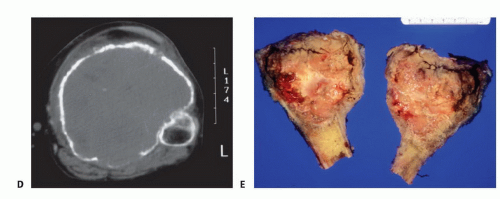
CT and MR imaging are useful to determine the extent of cortical destruction and intramedullary and soft tissue extensions of the primary tumor. These data are essential for determining the level of tibial resection, which is 3 to 5 cm distal to the area of intramedullary tumor involvement. MR imaging can also reveal skip lesions, which may affect the extent of tibial resection (FIGS 3 and 4).
Angiography
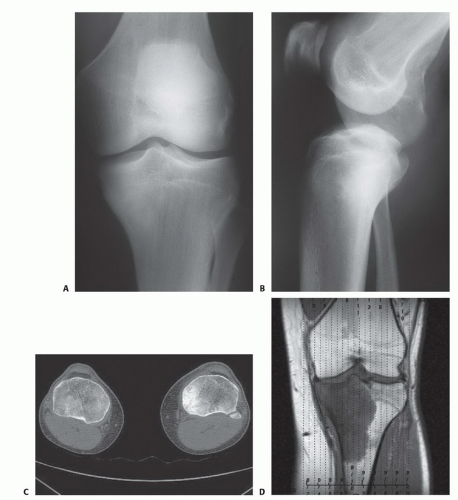
Biplane angiography (FIG 5) is used for local arterial evaluation, especially if CT has revealed posterior soft tissue extension. The anteroposterior view is used to evaluate the popliteal bifurcation; of particular relevance is the integrity of the posterior tibial artery, which may be the sole blood supply to the leg after resection.
The lateral view is essential for evaluating the interval between the tibia and the neurovascular bundle. For example, the popliteus muscle often separates a posterior tumor mass from the vessels. This is reflected as a clear interval on the lateral angiogram and serves as an indication that there is an adequate resection margin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree