Erythrocytes must regulate hemoglobin synthesis to limit the toxicities of unstable free globin chain subunits. This regulation is particularly relevant in β-thalassemia, in which β-globin deficiency causes accumulation of free α-globin, which forms intracellular precipitates that destroy erythroid precursors. Experimental evidence accumulated over more than 40 years indicates that erythroid cells can neutralize moderate amounts of free α-globin through generalized protein quality control mechanisms, including molecular chaperones, the ubiquitin-proteasome system, and autophagy. In many ways, β-thalassemia resembles protein aggregation disorders of the nervous system, liver, and other tissues, which occur when levels of unstable proteins overwhelm cellular compensatory mechanisms. Information gained from studies of nonerythroid protein aggregation disorders may be exploited to further understand and perhaps treat β-thalassemia.
Hemoglobin synthesis during erythroid maturation is tightly coordinated to maximize the production of functional hemoglobin A (α 2 β 2 ) and to balance the levels of individual globin subunits, which are unstable and cytotoxic in the absence of their partners. The importance of this homeostasis is illustrated in β-thalassemia, a common inherited anemia in which β-globin gene mutations cause a relative excess of free α-globin, which forms intracellular precipitates and reactive oxygen species. Accumulation of free α chains destroys erythroid precursors by ineffective erythropoiesis and also shortens the life span of mature erythrocytes. The phenotype of β-thalassemia is largely determined by the degree of free α-globin excess and is characterized by minimal symptoms in β-thalassemia minor to severe symptoms in β-thalassemia major. Individuals who are heterozygous for a β-globin null allele (β-thalassemia trait) are usually unaffected despite synthesis of 2-fold excess α-globin, indicating that erythroid precursors are able to neutralize significant amounts of free α-globin. Defining the associated protective mechanisms will provide insights into basic erythroid biology and may also have implications for treating β-thalassemia.
Virtually all cell types detoxify and/or degrade potentially damaging unstable proteins through mechanisms termed protein quality control. Numerous diseases ensue when the levels of unstable proteins exceed tissue capacities for quality control. Excessive protein misfolding, aggregation, and consequent toxicities are linked to the pathogenesis of numerous diseases affecting the nervous system, heart, pancreas, liver, and other tissues. In β-thalassemia, abundant excess α-globin is destabilized by several mechanisms, including deficiency of its natural binding partner β globin and autocatalytic oxidative stress. It is likely that this disease affects erythroid protein quality control mechanisms and vice versa. This article reviews experimental evidence indicating that erythroid cells can mitigate the toxicity of excess α-globin to a certain extent using generally conserved protein quality control pathways. The authors propose that β-thalassemia fits within a broader framework of protein aggregation disorders and that by applying the lessons learned from these nonerythroid diseases, the understanding of β-thalassemia pathogenesis can be extended to devise novel therapies for this common genetic disorder that causes significant morbidity in many areas of the world. Moreover, closer examination of protein quality control using β-thalassemia as a model system could provide new insights into rare protein aggregation disorders affecting other tissues.
General principles of protein quality control: how cells handle unstable proteins
Basic principles of protein quality control are discussed briefly in this article and reviewed more extensively elsewhere. Protein misfolding occurs frequently in all cells by “off-pathway” folding of otherwise normal polypeptides and random biosynthetic errors. High protein concentrations and rapid biosynthesis of proteins on polysomes increase nonproductive associations that lead to misfolding and aggregation. These processes are accelerated either during or after protein synthesis by various insults, including destabilizing mutations, deficiency of endogenous binding partners, and environmental stresses such as thermal and oxidant injury ( Table 1 ). Several of these factors apply to β-thalassemia and other hemoglobinopathies.
| Intrinsic Causes | |
| Mutated or incomplete proteins | Coding sequence mutations (missense or nonsense), synthetic errors, premature translation termination, proteolytic cleavage products |
| Lack of binding partner a | Absence of obligate chaperone or multimeric complex partners, excess subunit synthesis |
| Postsynthetic damage a | Oxidative or free radical damage, covalent modifications, denaturation, proteolytic cleavage |
| Misfolded proteins | Off-pathway folding, an inherent part of protein synthesis and existence |
| Intracellular Conditions | |
| Thermal stress | Thermal denaturation |
| Reactive small molecules and free radicals a | Oxidation, nitrosylation, glycation, deamidation, oxidative cross-linking |
| Extremes of ionic strength and pH | Favor multimer dissociation and protein denaturation |
| Macromolecular crowding a | High rates of protein synthesis |
| Presence of other misfolded or unfolded proteins a | Nascent polypeptides (not yet fully folded), misfolded or mutated proteins, depletion of chaperones by other stresses |
Misfolded and aggregated proteins can be deleterious to the cell not only through loss of protein function but also via toxic gain of function. These proteins can interfere with other normal proteins directly by physical interactions or indirectly by sequestering and monopolizing protein quality control system components that regulate critical cellular functions. Numerous interdependent elements contribute to protein quality control in virtually all cells. These elements include molecular chaperones, the ubiquitin-proteasome system (UPS), and lysosome-autophagy pathways.
Molecular Chaperones
Molecular chaperones represent a diverse and multifunctional class of proteins that bind “client” proteins to facilitate their folding and/or assembly into multisubunit complexes. Most chaperones, termed “public,” recognize a broad range of client proteins, frequently through interactions with hydrophobic surfaces. For example, ubiquitously expressed heat shock protein (Hsp) 70 is estimated to bind up to 15% to 20% of newly synthesized proteins in mammalian cells. Other “private” chaperones perform specialized functions by recognizing more limited repertoires of client proteins. Molecular chaperones participate in protein quality control through several mechanisms. These chaperones promote folding of many newly synthesized proteins and also help to repair proteins that become misfolded during cellular stress. In addition, chaperones irreversibly bind damaged proteins to mitigate their potentially toxic effects, direct their subcellular localization to structures termed aggresomes, and/or facilitate their degradation through lysosome-autophagy or ubiquitin-proteasome proteolytic systems.
The UPS
The UPS for protein degradation was initially recognized and characterized in reticulocytes and is now known to regulate numerous essential functions in all cells. For example, the UPS regulates cell growth, division, and differentiation through precisely timed proteolysis of specific substrates. Oxygen-sensitive UPS pathways regulate erythropoietin production to maintain circulating erythrocytes. The UPS also participates in protein quality control by degrading misfolded and otherwise damaged proteins. Proteins are generally marked for degradation by covalent conjugation of polyubiquitin chains, which serve as a recognition signal for the 26S proteasome complex. Ubiquitin is joined to target proteins by the concerted action of E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin-protein ligases, with the E3-ligase complex providing substrate specificity. E3 ubiquitin ligases recognize substrates on their own or through interactions with chaperones and other adapter proteins, allowing for multiple layers of regulation and specificity for both normal and damaged proteins.
Autophagy
Autophagy refers to numerous processes in which cytoplasmic proteins or whole organelles are degraded by lysosomes. Macroautophagy, the most commonly cited and best understood form, is a highly conserved pathway for bulk degradation of cytoplasmic contents, including organelles. During this process, the material to be degraded is enveloped in a double-membrane autophagosome, which fuses with a lysosome to form an autolysosome. Chaperone-mediated autophagy represents direct translocation of chaperone-unfolded proteins into the lysosome for subsequent degradation. Microautophagy is the capture of small amounts of cytoplasmic material through direct invagination of lysosomal membranes. The most well-defined function of autophagy is the maintenance of the amino acid pool during starvation through nonspecific bulk protein degradation. However, recent work illustrates the importance of autophagy in a broad range of cellular functions. For example, during erythropoiesis, mitochondria are removed from reticulocytes through macroautophagy (discussed later). Autophagy-mediated processes also participate in cellular protein quality control by removing misfolded and aggregated proteins, as illustrated in studies of neurodegenerative diseases.
Aggresomes
Until recently, protein aggregation was thought to be a passive process induced by association of sticky misfolded polypeptides. However, new studies suggest that formation of aggregates may be a conserved and regulated process whereby abnormal proteins are sequestered into organized structures termed aggresomes to inhibit harmful interactions with normal proteins and facilitate subsequent degradation.
Aggresomes form when the cell’s capacity to remove or repair abnormal proteins is exceeded. These structures were initially described for abnormal membrane-bound proteins, including the cystic fibrosis transmembrane receptor, but subsequently identified in a variety of diseases associated with abnormal cytoplasmic proteins. In tissue culture models, aggresome formation is induced by the expression of unstable proteins and/or inhibition of proteasomal degradation pathways. Aggresomes surround centrioles (the microtubule organizing center [MTOC]) and may be enclosed in an intermediate filament cage. Aggresome formation is microtubule-dependent, and the current model holds that microtubule-associated motor proteins actively deliver dispersed protein precipitates to MTOC-associated aggresomes. Aggresomes contain ubiquitinated proteins, molecular chaperones, and multiple components of the ubiquitin-proteasome pathway.
Current studies indicate a central role for aggresomes in protein quality control pathways. Proteasomes and chaperones such as Hsp70 and Hsp90 are present at the MTOC under basal conditions, perhaps to form the basis of an organized protein quality control center. Although aggresomes are relatively insoluble, their contents are dynamic. Photobleaching studies demonstrate the capacity for aggresomes to exchange contents with soluble cytoplasmic compartments, perhaps through chaperone-mediated refolding. The presence of proteasomes within aggresomes suggests that they can also serve as a proteolysis center. Aggresomes may also target abnormal proteins for degradation through autophagy. A critical aggresome component, p62/SQSTM, can bind polyubiquitinated proteins and polymerize around them, forming a shell to facilitate fusion with lysosomes. Aggresomes can also sequester precipitated proteins that cannot be degraded, perhaps limiting their toxicity. Overall, it seems that the functions of aggresomes and the ultimate fate of their contents depend on the cell type and the nature of the resident abnormal proteins.
Protein quality control pathways in disease
Disorders of protein aggregation have mainly been characterized in the central nervous system, but they also involve numerous other tissues including liver, heart, and pancreas ( Table 2 ). Despite divergent affected cell types and clinical features, several common themes emerge. First, abnormal disease-associated proteins are generally cleared through autophagy and/or the UPS. Clinical manifestations of cytotoxicity ensue when quality control systems become overloaded as cells age and accumulate excess aggregated protein over time. Second, abnormal proteins are frequently sequestered in aggresome-like structures, named according to the disease. For example, Mallory bodies in alcoholic liver disease and Lewy bodies in Parkinson disease resemble aggresomes morphologically and contain known aggresome components such as p62/SQSTM1. Third, diverse aggregation-prone proteins share similar mechanisms of cytotoxicity. One hypothesis is that these aggregates globally inhibit protein quality control systems through numerous potential mechanisms, including sequestration of proteasomes and chaperones, physical clogging of proteasomes, depletion of the free ubiquitin pool, and increased oxidative stress. The result is misfolding and accumulation of “bystander” proteins and impaired degradation of critical physiologic proteasome substrates such as cell cycle regulators, leading to cellular dysfunction and apoptosis.
| Disease | Abnormal Protein | Cell Type | Intracellular Inclusion |
|---|---|---|---|
| Alzheimer Disease | Tau | Neurons | Neurofibrillar tangles |
| Amyotrophic Lateral Sclerosis (Familial) | Superoxide dismutase 1 | Neurons | Bunina bodies |
| Parkinson’s Disease | α-Synuclein | Neurons | Lewy bodies |
| Huntington’s Disease | Huntingtin (polyglutamine expansion) | Neurons | — |
| X-Linked Spinobulbar Muscular Atrophy (Kennedy Disease) | Androgen receptor (polyglutamine expansion) | Neurons | — |
| Prion Disease | Prion protein | Neurons | — |
| α 1 -Antitrypsin Deficiency | α 1 -Antitrypsin | Hepatocytes | — |
| Alcoholic Liver Disease | Intermediate filaments | Hepatocytes | Mallory bodies |
| Wilson Disease | ATP7B | Hepatocytes | — |
| β-Thalassemia | α Globin | Erythrocytes | — |
One example of a protein aggregation disorder is familial ALS caused by mutations in superoxide dismutase 1 gene, SOD1 . These mutations cause toxicity not through loss of function but rather by generating a misfolded aggregation-prone protein with enhanced ability to generate reactive oxygen species, analogous to the properties of free α globin in β-thalassemia. Mutant SOD1 proteins are associated with aggresome-like structures and cause global dysfunction of the UPS. Overexpression of the chaperone Hsp70 or Dorfin, a ubiquitin ligase that recognizes SOD1 mutants, partially rescues the toxicity of SOD1 mutations by stabilizing the abnormal proteins or facilitating their degradation. In this way, efforts to define how protein quality control systems intersect with disease pathophysiology have elucidated new pathways for potential therapeutic manipulation.
Protein quality control pathways in disease
Disorders of protein aggregation have mainly been characterized in the central nervous system, but they also involve numerous other tissues including liver, heart, and pancreas ( Table 2 ). Despite divergent affected cell types and clinical features, several common themes emerge. First, abnormal disease-associated proteins are generally cleared through autophagy and/or the UPS. Clinical manifestations of cytotoxicity ensue when quality control systems become overloaded as cells age and accumulate excess aggregated protein over time. Second, abnormal proteins are frequently sequestered in aggresome-like structures, named according to the disease. For example, Mallory bodies in alcoholic liver disease and Lewy bodies in Parkinson disease resemble aggresomes morphologically and contain known aggresome components such as p62/SQSTM1. Third, diverse aggregation-prone proteins share similar mechanisms of cytotoxicity. One hypothesis is that these aggregates globally inhibit protein quality control systems through numerous potential mechanisms, including sequestration of proteasomes and chaperones, physical clogging of proteasomes, depletion of the free ubiquitin pool, and increased oxidative stress. The result is misfolding and accumulation of “bystander” proteins and impaired degradation of critical physiologic proteasome substrates such as cell cycle regulators, leading to cellular dysfunction and apoptosis.
| Disease | Abnormal Protein | Cell Type | Intracellular Inclusion |
|---|---|---|---|
| Alzheimer Disease | Tau | Neurons | Neurofibrillar tangles |
| Amyotrophic Lateral Sclerosis (Familial) | Superoxide dismutase 1 | Neurons | Bunina bodies |
| Parkinson’s Disease | α-Synuclein | Neurons | Lewy bodies |
| Huntington’s Disease | Huntingtin (polyglutamine expansion) | Neurons | — |
| X-Linked Spinobulbar Muscular Atrophy (Kennedy Disease) | Androgen receptor (polyglutamine expansion) | Neurons | — |
| Prion Disease | Prion protein | Neurons | — |
| α 1 -Antitrypsin Deficiency | α 1 -Antitrypsin | Hepatocytes | — |
| Alcoholic Liver Disease | Intermediate filaments | Hepatocytes | Mallory bodies |
| Wilson Disease | ATP7B | Hepatocytes | — |
| β-Thalassemia | α Globin | Erythrocytes | — |
One example of a protein aggregation disorder is familial ALS caused by mutations in superoxide dismutase 1 gene, SOD1 . These mutations cause toxicity not through loss of function but rather by generating a misfolded aggregation-prone protein with enhanced ability to generate reactive oxygen species, analogous to the properties of free α globin in β-thalassemia. Mutant SOD1 proteins are associated with aggresome-like structures and cause global dysfunction of the UPS. Overexpression of the chaperone Hsp70 or Dorfin, a ubiquitin ligase that recognizes SOD1 mutants, partially rescues the toxicity of SOD1 mutations by stabilizing the abnormal proteins or facilitating their degradation. In this way, efforts to define how protein quality control systems intersect with disease pathophysiology have elucidated new pathways for potential therapeutic manipulation.
Protein quality control systems in erythropoiesis
Erythroid maturation presents unique protein quality control challenges, including the high concentration of cytotoxic hemoglobin subunit proteins, oxidative stress associated with iron (both free and heme-bound), and the need to clear unnecessary nonglobin proteins and organelles during terminal maturation. Accordingly, many of the principles and systems of protein quality control can be applied to normal erythroid development and associated diseases, particularly hemoglobinopathies such as β-thalassemia.
Molecular Chaperones
The involvement of molecular chaperone systems in erythroid development is reviewed by Weiss and Dos Santos. Reticulocytes can increase the production of chaperones in response to stress by preferential messenger RNA translation, indicating the importance of protein quality control during late-stage erythroid maturation. Public chaperones such as Hsp70 facilitate erythroid maturation through regulation of key erythroid proteins. α-Hemoglobin stabilizing protein (AHSP) is an erythroid-specific private chaperone that specifically stabilizes free α-globin subunits. Loss of AHSP in mice causes hemolytic anemia with globin precipitates (Heinz bodies) and exacerbates β-thalassemia. Other important globin chaperones, both private and public, are likely to play additional important roles in erythropoiesis.
Ubiquitin-Mediated Proteolysis
The UPS was initially described in reticulocytes, a relatively simple anucleate cell that degrades multiple proteins as part of normal maturation. More recent studies have explored the role of proteasome-dependent protein degradation during erythropoiesis. Activated erythropoietin receptors may be cleared in part by proteasomal degradation. Cytoskeletal proteins actin and tubulin are degraded by the UPS in reticulocytes, and pharmacologic proteasome inhibition interferes with numerous aspects of erythroid maturation in vitro, including enucleation. General understanding of the UPS and its components is expanding rapidly, and future studies will likely identify additional roles for targeted proteolysis in globin homeostasis and erythroid maturation.
Autophagy
Maturing erythroid cells eliminate not only soluble proteins but also organelles. Reticulocytes degrade mitochondria and ribosomes by autophagy. Targeted deletions of murine genes encoding macroautophagy pathway components, including Nix , Ulk1 , and Atg7 , interfere to varying degrees with physiologic degradation of mitochondria during reticulocyte maturation. Morphologic studies described later in this review illustrate lysosomal engulfment of α-globin inclusions in β-thalassemic erythroblasts, although the overall importance of autophagic pathways in degrading excess α-globin is not known.
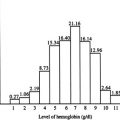
Proteolytic control of globin chain balance
The synthesis and subsequent fate of nascent globin chains have been analyzed extensively through pulse-labeling studies in normal and thalassemic erythroid precursors. Normally, globin chain synthesis is relatively balanced, with some studies revealing a slight excess of α chains in a soluble pool. The per-cell globin chain synthetic rates are highest in the basophilic erythroblast stage and decrease as the cells mature, but globin synthesis and accumulation continues through the late stages, with reticulocytes producing as much as 7% to 20% of the total hemoglobin content. β-Thalassemic erythroid precursors contain a larger pool of excess free α chains that are initially competent to form hemoglobin tetramers but are unstable in the absence of their binding partner. These early studies provided first evidence linking α-globin excess to the pathophysiology of β-thalassemia. Analysis of the erythroid precursors in β-thalassemia trait and intermedia at different stages of maturation provided further insights into globin chain metabolism. In these studies, the α to β chain ratio increased during successive stages of maturation, with the highest amounts of α-globin excess found in circulating reticulocytes. Prolonged labeling experiments showed that in bone marrow erythroblasts, β chains accumulate at a constant rate but nascent α chain levels stabilize over time, so that the α to β chain ratio decreased. This effect was highest in the earlier maturation stages. These data indicate that β-thalassemic erythroid precursors, particularly at early developmental states, degrade excess α-globin to prevent its accumulation. This protective mechanism becomes less effective during the course of maturation as globin chains accumulate and the capacity to remove excess α chains becomes overwhelmed.
Subsequent experiments characterized the proteolytic degradation of α-globin. Hanash and colleagues mixed reticulocyte and normoblast lysates to show that earlier erythroid precursors have a greater capacity to degrade excess α chains. This activity was specific for α-globin and blocked by proteolysis inhibitors. Moreover, α-globin proteolysis was higher in erythroid precursors of patients with β-thalassemia than in those of patients with other anemias or causes of reticulocytosis. Early experiments describing the UPS in reticulocyte lysates used denatured globins or globin chains rendered unstable by incorporation of amino acid analogues. These experiments indicate that erythroid precursors have the capacity to degrade excess or structurally unstable globins.
Studies by Shaeffer focused on the role of the UPS in α-globin degradation. Pulse-chase labeling of intact β-thalassemia reticulocytes showed that they degrade endogenous α-globin but not β-globin, in an ATP-dependent manner. Biochemical studies showed that β-thalassemia reticulocyte lysates can ubiquitinate added α-globin at several sites to facilitate its degradation by proteasomes. Moreover, mono- or polyubiquitination of α-globin was required for its proteasomal degradation. Further work has shown that free α, β, and γ globin chains can be ubiquitinated and degraded using in vitro reconstituted systems and that this process can occur cotranslationally or shortly after the release of the nascent chains from ribosomes.
One implication of this research is that the differences in proteolytic capacity for α-globin may account for some of the phenotypic heterogeneity in β-thalassemia and for the interspecies differences in the manifestations of β-globin gene mutations. In humans, a 50% reduction in β-globin synthesis usually results in the asymptomatic β-thalassemia trait. In mice, a similar reduction in the β-globin gene dosage causes a more severe phenotype that resembles β-thalassemia intermedia. Rouyer-Fessard and colleagues have suggested that this interspecies difference may be due in part to reduced capacity for degrading unstable toxic α-globin in mouse erythroblasts.
Accumulation of free β-globin chains in α-thalassemia also poses protein quality control problems for erythroid precursors. For example, pulse-chase labeling of reticulocytes from a patient with α-thalassemia showed normalization of globin chain accumulation through preferential degradation of β-globin, similar to what is seen with α chains in β-thalassemia. However, free β-like globin chains are more stable and soluble than α-globin, partly due to formation of homotetramers. Compared to β-thalassemia, α-thalassemia is associated with fewer globin precipitates in erythroid precursors and reduced ineffective erythropoiesis. However, severe forms of α-thalassemia are characterized by extensive hemoglobin H (HbH) (β 4 ) inclusions in circulating erythrocytes, causing shortened half-life and anemia. Further comparative studies are required to better define the similarities and differences in how protein quality control pathways handle excess free α and β-globin chains.
Together, numerous studies over many years have indicated that the UPS can degrade unstable globins as a protective mechanism against hemoglobinopathies, particularly β-thalassemia. Additional proteolytic systems may complement this UPS function. For example, oxidant-damaged hemoglobin can be degraded by intact reticulocytes and extracts in ATP- and ubiquitin-independent pathways, possibly through a cytosolic protease. This activity seems to be retained in mature erythrocytes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree