Fig. 7.1
(a) Endoscopic view of a squamous cell carcinoma (SCC) of the left vocal fold. (b) Preoperative CT scan of the same lesion showing the invasion of the left anterior paraglottic space. (c) Endoscopic view 3 years after TLM
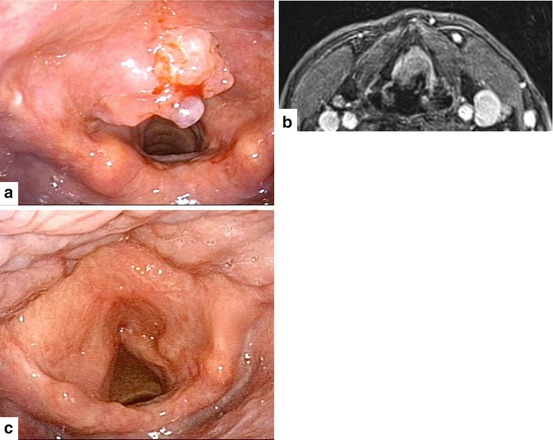
Fig. 7.2
(a) Endoscopic view of an SCC invading the infrahyoid portion of the epiglottis. (b) Preoperative MRI showing partial involvement of the preepiglottic space without infiltration of the thyroid cartilage. (c) Endoscopic view 2 years after TLM
For some authors [39], radical control of disease by a transoral approach cannot be achieved when the lesion involves the laryngeal framework and/or tends to grow outside the laryngeal box. The efficiency of CT or MRI to preoperatively diagnose minimal cartilaginous involvement is around 60–80 %; [44, 51] therefore, cartilage infiltration is often an intraoperative finding, accompanied by the impossibility to obtain frozen sections on cartilaginous tissue. The removal of a cartilage window or extensive vaporization of the involved thyroid laminae recommended by some authors [32–34] is not a guarantee of good oncologic results [38, 39, 52, 53].
Vocal cord mobility is another crucial issue: vocal fold fixation (associated or not with arytenoid fixation, [33, 38]) represents an independent risk factor for local recurrence in patients treated by TLM, with 5-year local control ranging between 50 and 70 % [54]. As proposed by Holsinger et al., tumors with complete fixation of the arytenoid and vocal cord should be classified as T3b, while tumors with scarce mobility or cord fixation, but with a functional cricoarytenoid joint, should be categorized as T3a. Only the latter are amenable to partial or subtotal removal of the arytenoid [55]. Although it is technically possible to perform total arytenoidectomy, this extreme endoscopic procedure has functional limitations, with frequent secondary aspirations.
Moderate infiltration of the paraglottic and preepiglottic space can be managed by TLM: however, the narrow space of work in the posterior crico-thyro-arytenoid corner, in comparison with the relatively wider view allowed at the supraglottic level, may be crucial in determining a higher failure rate [39].
Another matter of debate is the decision of skipping neck dissection in cases of a clinically and radiologically negative neck (cN0). During conventional open surgery, neck dissection is generally performed at the same time as the primary resection. Many authors recommend to perform neck dissection 2 weeks after TLM as a second-stage procedure, thus decreasing the risk of laryngeal edema (and, consequently, tracheotomy) and fistula, and allowing reevaluation of the surgical field in view of the definitive histopathology [29, 37, 56]. In case of a wait-and-see policy, strict clinical examination every 2–3 months in the first 2 years, with periodic ultrasound examinations of the neck, is mandatory to identify positive nodes at an early stage in order to perform delayed neck dissection without compromising survival. Oncologic outcomes of TLM in locally-advanced glottic and supraglottic tumors are summarized in Tables 7.1 and 7.2, respectively.
Table 7.1
Review of published data on oncologic results of TLM for advanced glottic cancer
Author(s) | Number of patients | pT | Treatment | LC with TLM (follow-up) | Final LC (follow-up) | DSS (follow-up) | OS (follow-up) |
|---|---|---|---|---|---|---|---|
Ambrosch et al. (2001) [57] | 167 | T3 | TLM | 68 % (5 y) | 87 % (5 y) | 62 % (5 y) | – |
Motta et al. (2005) [58] | 51 | T3 | TLM | 65 % (5 y) | – | 72 % (5 y) | 64 % (5 y) |
Grant et al. (2007) [30] | 10 | T3–4 | TLM ± RT | 45 % (4 y) | – | – | 62 % (4 y) |
Peretti et al. (2010) [24] | 11 | T3 | TLM | 71.6 % (5 y) | – | 100 % (5 y) | – |
Vilaseca et al. (2010) [54] | 51 | T3 | TLM | 47.1 % (5 y) | 88.2 % (5 y) | 86.3 % (5 y) | 73.1 % (5 y) |
Blanch et al. (2011) [44] | 26 | T3 (AC+) | TLM | – | 80.4 % (5 y) | – | – |
Peretti et al. (2013) [59] | 30 | T3 | TLM ± RT/CRT | 55 % (5 y) | – | – | – |
Canis et al. (2014) [60] | 122 | T3 | TLM ± adjuvant RT/CRT | 71.5 % (5 y) | 83 % OP (5 y) | 84.1 % (5 y) | 58.6 % (5 y) |
Pantazis et al. (2015) [13] | 19 | T3 | TLM ± adjuvant RT/CRT | 52.6 % (5 y) | 73.7 % (5 y) | 63.2 % (5 y) | 63.2 % (5 y) |
Table 7.2
Review of published data on oncologic results of TLM for advanced supraglottic cancer
Author(s) | Number of patients | pT | Treatment (follow-up) | LC with TLM (follow-up) | Final LC (follow-up) | DSS (follow-up) | OS (follow-up) |
|---|---|---|---|---|---|---|---|
Iro et al. (1998) [27] | 48 | 3–4a | TLM ± ND ± RT | 83.3 % (5 y) | – | – | – |
Rudert et al. (1999) [29] | 17 | 3–4a | TLM ± ND ± RT | – | – | – | 47 % (5 y) |
Ambrosch et al. (2001) [57] | 50 | 3–4a | TLM ± ND ± RT | 86 % (5 y) | 91 % (5 y) | 71 % (5 y) | – |
Motta et al. (2004) [61] | 18 | 3 | TLM | 77 % (5 y) | – | 81 % (5 y) | 81 % (5 y) |
Grant et al. (2007) [62] | 10 | 3–4a | TLM ± ND ± RT | T3 100 % (3 y) T4 80 % (4 y) | – | – | T3 67 % (3 y) T4 75 % (4 y) |
Cabanillas et al. (2008) [63] | 15 | 3 | TLM ± ND ± RT | 70 % (5 y) | – | 80 % (5 y) | – |
Peretti et al. (2010) [24] | 20 | 3 | TLM ± ND ± RT/CRT | 83 % (5 y) | – | – | – |
Vilaseca et al. (2010) [54] | 96 | 3 | TLM ± ND ± RT | 69.8 % (5 y) | 91.7 % (5 y) | 61.8 % (5 y) | 45.8 % (5 y) |
Canis et al. (2013) [35] | 104 | 3 | TLM ± ND ± RT/CRT | 77.3 % (5 y) | 92 % OP (5 y) | 84.2 % (5 y) | 66.5 % (5 y) |
Pantazis et al. 2015 [13] | 24 | 3 | TLM ± ND ± RT/CRT | 87.5 % (5 y) | 91.7 % OP (5 y) | 91.7 % (5 y) | 87.5 % (5 y) |
From a functional point of view, the possibility to tailor the TLM resection allows various structures to be maintained. Preservation of the laryngeal framework, infrahyoid musculature, superior laryngeal nerves, pharyngeal constrictor muscles, and hyoid bone limits the consequences on postoperative swallowing mechanisms [59, 64–69]. This leads to a reduced need for tracheotomy or feeding tube, faster rehabilitation, and reduction of more than 50 % in hospital stay compared with open-neck procedures [59, 60, 68–70].
In studies including advanced cancers, complications have been significantly correlated with tumor size, surgeon experience, and tumor location [71]. The most significant complications reported are postoperative bleeding, aspiration pneumonia, cervical emphysema, dyspnea, local infection, and cervical fistula. Postoperative hemorrhage is the most common and feared complication due to the vital risk for patients generally without tracheotomies [33], with a similar incidence to open approaches (3–14 %) [71]. The second most frequent complication, especially in case of supraglottic laryngectomy, is aspiration pneumonia: temporary aspiration rate favorably compares with data reported after open partial approaches (32–89 %) and CRT organ preservation protocols (up to 84 %) [72–74]. In the study by Vilaseca et al., the reported rate of aspiration pneumonia in a cohort of patients with T3–4a supraglottic carcinomas treated by TLM was 6.5 % (only 1.3 % of patients had repeated pneumonia) [34].
Peretti et al., in a cohort of glottic pT2 and selected pT3, reported that postoperative subjective satisfactory swallowing was significantly better (95.7 %) compared to data reported in the literature after supracricoid partial laryngectomy (59.8 %) and CRT (61.9 %). The same trend was confirmed by objective evaluation of swallowing, with the majority of patients presenting normal function after TLM. Hospitalization time was significantly shorter compared to RT protocols (8.3 vs. 20–24 days). Moreover, reduction in perioperative morbidity following TLM seems to fit better with the overall general frail conditions of elderly patients and those with poor pulmonary function (both at higher risk of aspiration pneumonia) [59, 71].
Oropharyngeal Cancer
The majority of studies investigating the role of TLM in the treatment of oropharyngeal cancer have recruited a limited number of patients with a short follow-up [75–77]. However, a multicenter study by Haughey et al. [78] analyzed a series of 204 patients undergoing TLM for high-stage oropharyngeal cancer, 34 % with T3–T4 tumors. After resection, 117 (58 %) patients received adjuvant RT alone, whereas 33 (16 %) received adjuvant CRT. The authors documented a statistically significant difference in survival in T1–T2 vs. T3–T4 tumors (p = 0.025), with a risk of death that was twofold greater (HR 2.0–2.3) in higher T categories. Furthermore, the group with negative margins had fewer T3–T4 cases than the positive margins group (34 vs. 50 %), but the difference did not reach statistical significance. In this series, the 3-year overall survival was 86 %, locoregional control 93 %, and the long-term GT rate approximately 4 %. Similar results have been reported for a cohort of 71 patients, including 32 % of T3–T4 lesions, who underwent CRT [79]. Three-year overall survival was 83 %, locoregional control rate 90 % (including salvage surgery), but a GT rate of 35 % was observed. A similar study by Canis et al. [80] confirmed the efficacy of TLM, demonstrating 75 % 5-year locoregional control and 56 % 5-year overall survival for tonsillar pT3 and pT4a. Only 3 % of patients needed a permanent GT after surgery and adjuvant treatment. In this view, while maintaining comparable oncologic results (Table 7.3), TLM offered better functional outcomes than CRT.
Table 7.3
Summary of survival outcomes in recent series on TLM and TORS for advanced oropharyngeal cancer
Author(s) | Number of patients | Stage | Survival (follow-up) | Local control (follow-up) |
|---|---|---|---|---|
TLM | ||||
Haughey et al. (2011) [78] | 204 | III–IV | Stage III + IV (3 y) OS: 86 % RFS: 88 % | LC 97 % |
Canis et al. (2013) [80] | 102 | I–IV | Stage III + IV (5 y) OS: 56 % RFS: 60 % | T3–T4a (5 y) LC 75 % |
TORS | ||||
Weinstein et al. (2010) [81] | 47 | III–IV | Stage III–IV (2 y) DSS: 90 % | Stage III–IV (2 y) LC 98 % |
Hypopharyngeal Cancer
Approximately 70–85 % of patients affected by hypopharyngeal SCC reported in large series have stage III–IV disease at presentation, and the 5-year overall survival rate is reported to range from 15 to 45 %. In such a scenario, nonsurgical organ preservation protocols have been largely incorporated [6], but minimally invasive organ and function preserving surgery such as TLM has been investigated in the attempt to reduce CRT-related morbidities [82, 83]. However, in locally advanced tumors (T3–T4), experience with TLM is still limited and only a few institutions have treated a reasonably large cohort of patients [82, 84, 85]. Generally, TLM in hypopharyngeal SCC is the least established transoral laser procedure, even though in selected cases it has progressively replaced open partial pharyngectomies, especially in view of the better results achieved in chronic aspiration and pneumonia (Fig. 7.3) [86]. Furthermore, TLM has no age limit and tracheotomy is usually not required [87]. Tumors of the lateral pharyngeal wall are generally accessed with ease, while in tumors involving the retrocricoid area, an endoscopic approach is only suitable for lesions without cartilage or arytenoid joint involvement. In tumors of the medial wall and the apex of the piriform sinus, the absence of anatomical barriers to the supraglottic larynx and paraglottic space allows rapid invasion of these areas. In addition, the ipsilateral supraglottis and paraglottic space lateral to the vestibular fold should be included in the resection. A contraindication to TLM for hypopharyngeal cancer is invasion of the paraglottic space lateral to the true vocal cord [86].
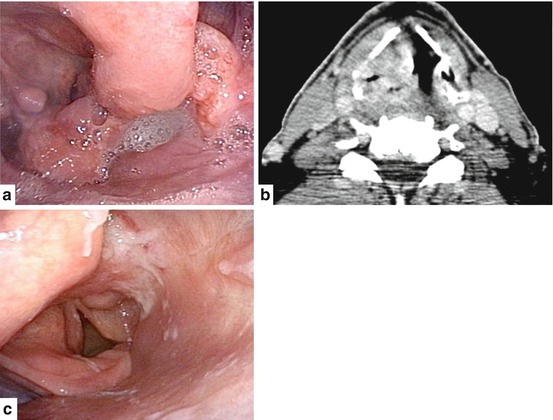
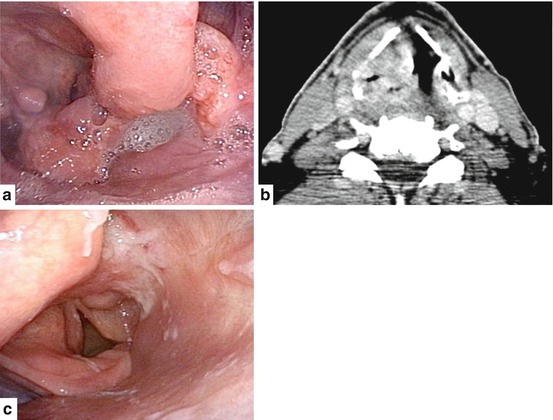
Fig. 7.3
(a) Endoscopic view of a T4a hypopharyngeal SCC of the right pyriform sinus and supraglottis. (b) Preoperative CT scan showing infiltration of the thyroid cartilage and adjacent tissues. (c) Endoscopic view 4 years after TLM and adjuvant CRT
Most patients affected by stage III-IV disease receive adjuvant RT/CRT and local control rates are better than those obtained with nonsurgical treatment alone [88]. In such a scenario, the question is whether the intensity of adjuvant treatment should be reduced after TLM, thus making the surgery worthwhile or, on the contrary, will only increase side-effects. On one hand, surgery gives the possibility to have objective pathologic data about the true tumor extension and neck involvement. On the other, the risk of distant disease supports the use of CRT regimens as adjuvant treatment. In any case, these treatments are expensive, may increase toxicity, and reduce the possibility of its use in the not uncommon event of a second primary which may then not be treated by TLM [87]. In summary, the oncologic results of TLM in hypopharyngeal cancer appear comparable with open approaches, with a 5-year overall survival (OS) of about 40–50 % in stage III and IV, and 5-year disease specific survival (DSS) around 60 %. Higher rates of laryngeal preservation in these selected cases are also reported (Table 7.4).
Table 7.4
Oncologic results of TLM for advanced hypopharyngeal cancer
Author(s) | Number of patients | Stage | Survival (follow-up) | Local control |
|---|---|---|---|---|
Steiner et al. (2001) [84] | 129 | III–IV | Stage III + IV (5 y) OS: 47 % RFS: 69 % | – |
Vilaseca et al. (2004) [85] | 28 | II–IV | Stage II + IV (4 y) OS: 43 % | LC T3 56.2 % (n = 49) LC T4 100 % (n = 1) OP 79 % |
Martin et al. (2008) [82] | 172 | III–IV | Stage III (5 y) OS: 64 % DSS: 86 % Stage IV (5 y) OS: 41 % DSS: 57 % | LC T3 75 % (n = 75) (82 % plus adjuvant RT vs. 66 % without) LC T4 57 % (n = 28) |
Transoral Robotic Surgery
Laryngeal Cancer
The current size and rigidity of instruments commonly used in TORS can render a transoral robotic approach to the larynx and hypopharynx cumbersome; [89–91] furthermore, tracheotomy is often required [92]. New instruments and surgical systems that are not limited by “a straight line approach” (the Flex System, the Robo-ELF, and the MicroRALP system) [93, 94], can potentially overcome these challenges, but applicability in surgical procedures of the larynx has not yet been shown in a clinical setting [95–97].
TORS has mainly found three applications in cancer of the larynx: supraglottic laryngectomy [98, 99], total laryngectomy [100], and cordectomy [101]. When glottic cancer is considered, there are no reports on treatment of locally advanced tumors by TORS. Even for early lesions there is a lack of data on long term oncologic outcomes, while functional results (in terms of tracheotomy rate and nasogastric feeding tube) tend to be suboptimal compared to TLM [102–105].
Similarly, series on TORS supraglottic laryngectomy predominantly include early tumors (T1–T2), even though T3 lesions, based on preepiglottic space extension, are also amenable to this technique. Up to now, the overall small number of patients reported does not allow realistic comparison with other types of treatment, also considering the wide range of tracheotomy and GT rates in the different series [106–110]. Furthermore, Mendelsohn et al. described tumor stage as an important predictor of functional recovery, with low-T categories (pT1–pT2) having significant earlier return to swallowing, than more advanced ones (pT3) [111].
The rationale behind robotic total laryngectomy, although technically demanding and more costly, is to decrease postoperative morbidity and reduce recovery times [112], with a smaller pharyngotomy and maximally mucosa-sparing incisions, which minimize lateral dissection and preserve fascial barriers between the neopharynx and carotid sheaths. The indications for the procedure are yet to be well-defined and its main advantage seems to be experienced in salvage laryngectomy for functional reasons after CRT. However, to date, there are no data showing better results than open total laryngectomy [113–115].
Oropharyngeal Cancer
Before considering the potential applications of TORS for the treatment of advanced oropharyngeal squamous cell carcinomas (OPSCCs), it is essential to mention that the current staging system has relevant limitations in regard to stage grouping. For example, stage IV groups together patients with totally different disease, such as T1N2a and T4N2c. Therefore, it appears more reasonable to stratify indications for treatment based on T and N categories.
Especially in advanced tumors, the first-line approach has typically been CRT, in view of the good response and nonnegligible morbidity, even in the best hands, of conventional surgery. However, data published in the last decade have emphasized the remarkable late effects of CRT. At the same time, the striking increase of human papillomavirus (HPV)-related OPSCCs, which typically affect young patients not exposed to traditional risk factors such as smoking and alcohol, and associated with a better prognosis, have fostered the search for treatments that minimize functional sequelae without jeopardizing the disease control.
TORS have emerged in this context, showing promising potential especially for treatment of early OPSCC, but with less evidence in advanced tumors (Fig. 7.4). In this view, optimal treatment should find a balance between oncologic outcomes and functional results: on one hand, undertreatment can increase the risk of recurrence; while on the other, overtreatment can lead to worse functional results without improving survival. In high-stage OPSCC, the right balance is generally a dual-modality treatment (i.e., CRT or surgery + RT) or, in selected cases, a single-modality treatment (i.e., RT alone, or surgery alone). In some situations, TORS exposes the patient to a risk of overtreatment (i.e., triple-modality treatment: surgery + CRT) in case of positive margins or extracapsular extension at final histopathology. For this reason, in patients in whom preoperative staging reveals in advance the postoperative need for adjuvant CRT, TORS may not be the ideal choice of treatment. On the other hand, TORS provides both a therapeutic and diagnostic step that allows for assessment of pathologic findings and de-intensification of adjuvant treatment, thus avoiding chemotherapy in approximately 40 % of patients, with 10 % requiring no RT/CRT or allowing for utilization of standard postoperative RT dosages.
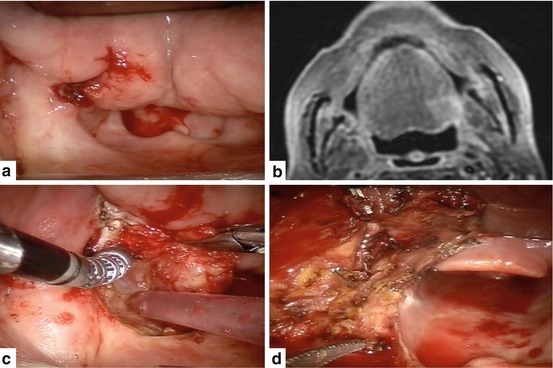
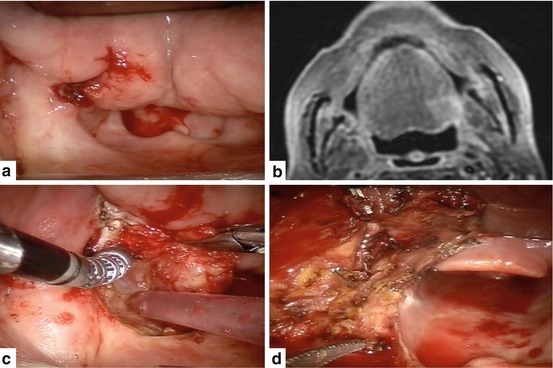
Fig. 7.4
(a, b) Intraoperative view and preoperative MRI of a T4a SCC of the left base of tongue and glossotonsillar sulcus. Deep infiltration of the tongue into the extrinsic muscles is depicted by MRI. (c, d) Intraoperative view during TORS and after tumor resection
Taking into consideration recent data concerning the treatment of OPSCC, Lorincz et al. [116] developed a decisional algorithm including TORS, conventional surgery, RT, and CRT. In their evaluation, TORS + neck dissection is considered as a valuable choice in tumors with low T categories (T1 or T2) and without radiologic signs of lymph-node extracapsular extension, reserving surgery + postoperative RT (60 Gy) in N2 and N3 patients. In fact, while different authors have reported optimal outcomes even in tumors with high T classification, there is no evidence of the reproducibility of such results outside these very selected series.
To date, there is limited data on oncologic outcomes of locally advanced tumors treated by TORS, since most series prevalently include T1–T2 neoplasms, with T3–T4 approximately accounting for only 20 % of cases [101, 117–119]. In a single series, compared directly to open approaches, TORS for T1–T3 tonsillar cancer was seen to have a higher rate of negative margins and more rapid functional recovery [120], showing its potential even in moderately advanced tumors. In a study by Weinstein et al. [81], excellent disease-free survival at 1 (96 %) and 2 years (79 %) was reported in 47 patients with stage III or IV OPSCC treated by TORS (Table 7.3). Regarding the need for adjuvant therapy, 39 % each required RT or CRT. However, comparison with CRT is difficult because of the heterogeneity of the different series, with TORS patients being generally characterized by lower stage and higher prevalence of HPV positive tumors. Furthermore, morbidity is often overestimated in the nonsurgical group used for comparison. In fact, in an “all stages” MSKCC cohort treated mainly (88 %) with concurrent CRT, the authors reported GT dependency in 7 % of patients at 1 year, which compares favorably with the significantly higher rates of functional complications after CRT reported in other studies [121–123]. Moreover, in this light, data from MSKCC are similar to those on chronic GT dependence after TORS, which in a systematic review by Hutcheson et al. [124] ranged from 0 to 7 % (mean follow-up, 11–26 months).
Transnasal Endoscopic Surgery
TES was introduced in the 1980s for treatment of inflammatory diseases of the nose and paranasal sinuses. The indications rapidly expanded to include first the management of benign tumors and subsequently the resection of malignant lesions of the sinonasal tract and nasopharynx.
The first experiences in the treatment of naso-ethmoidal malignancies were limited to lesions of different histology not encroaching the anterior skull base [125, 126]. However, with the refinement of duraplasty techniques, endoscopic surgeons started to approach even tumors eroding the skull base, invading the dura, or with limited extension to the brain (T3–T4a-b) [127–130]. The indications for TES in nasopharyngeal carcinoma vary in relation to histology. Based on the WHO classification [131], TES can be considered an alternative to re-irradiation in residual/recurrent T1, T2, and very selected T3 nasopharyngeal carcinomas or a reasonable primary treatment option in the more rarely observed salivary gland-type carcinomas or papillary adenocarcinoma.
Malignant Lesions of the Sinonasal Tract
Malignancies of the sinonasal tract are rare, accounting for 3 % of all cancers of the head and neck. Their major peculiarity is the extreme histological variability, which is frequently associated with variable natural history and response to different treatments. For a long time, surgery followed by RT or CRT has been invariably considered the standard of care for management of advanced lesions. The major advancement in surgery was the introduction in the 1960s of anterior craniofacial resection (ACR), a technique providing a reasonably good local control even to lesions encroaching on the anterior skull base. A multicenter collaborative study analyzing 1307 patients (with a reasonable number of patients in each histology group), who underwent ACR followed in most cases by radiotherapy, provided an excellent dataset on survival and morbidity outcomes to be used as a benchmark for future comparisons with alternative treatments [132, 133].
When TES was proposed for treatment of selected malignancies of the naso-ethmoidal complex, it was considered heresy, mainly for the impossibility in most cases to perform the resection according to an “en bloc” principle. However, from the beginning the philosophy guiding endoscopic surgery was to obtain radical resection of the tumor in free margins similar to external procedures. In view of the narrow access through the nostril(s), a new principle of resection (“tumor disassembling”), starting from the endonasal portion of the tumor and progressively removing in a centrifugal fashion different layers of tissue (mucoperiosteum of the naso-ethmoidal cavity on the most involved side; septum, if required; mucoperiosteum of the contralateral side; periorbit and/or dura, in relation to tumor extent), was introduced [127]. When dura of the anterior cranial fossa is resected, duraplasty is performed preferably with autologous material, with a multilayer technique [134] (Figs. 7.5, 7.6 and 7.7).
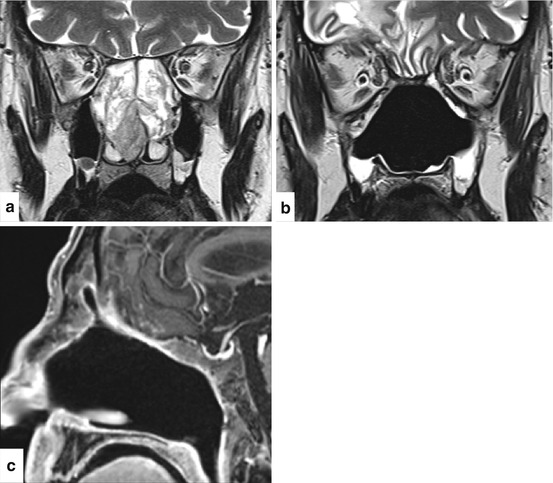
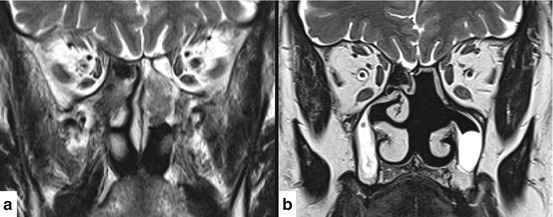
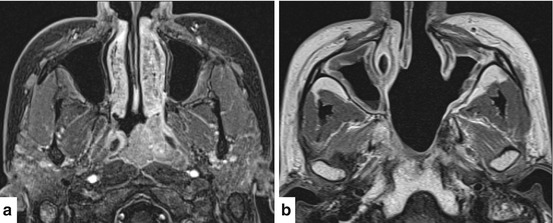
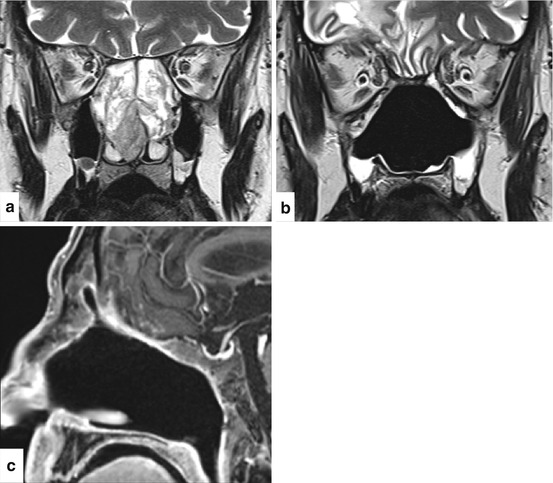
Fig. 7.5
Sinonasal adenoid cystic carcinoma in a 55-year-old man. (a) Coronal T2 weighted MRI sequence showing the lesion, which involves both nasal cavities with no evidence of orbital or transdural spread. Endoscopic resection with transnasal craniectomy and three-layer skull base reconstruction with iliotibial tract was performed. Histologic examination of the surgical specimen demonstrated microscopic infiltration of periobit and dura (pT4bN0M0G2). The patient underwent adjuvant RT. (b) Coronal T2 weighted and (c) contrast-enhanced sagittal T1 weighted MRI sequences show no evidence of disease and perfect healing of skull base reconstruction at 4 years after treatment
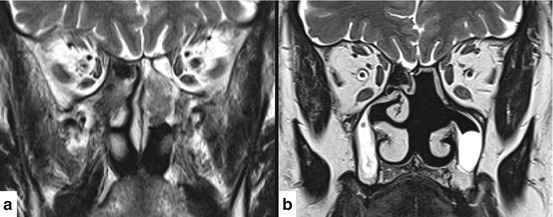
Fig. 7.6
Sinonasal intestinal-type adenocarcinoma in a 64-year-old male woodworker. (a) Coronal T2 weighted MRI sequence shows the lesion localized in the posterior ethmoid and confined to the left nasal cavity. Endoscopic resection with unilateral transnasal craniectomy and two-layer skull base reconstruction was performed. Histologic examination of the surgical specimen was consistent with intestinal-type adenocarcinoma pT2N0M0G2. No adjuvant radiotherapy was added. (b) Coronal T2 weighted MRI sequence shows no evidence of disease and regular healing of the surgical cavity 2 years after treatment
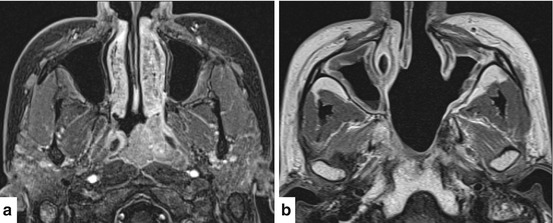
Fig. 7.7
Nasopharyngeal adenoid cystic carcinoma in a 32-year-old woman. (a) Contrast-enhanced axial T1 weighted MRI sequence shows the lesion centered in the left nasopharynx with contralateral extension along the posterior wall. Bilateral type III nasopharyngeal endoscopic resection was performed as primary treatment. Histologic examination of the surgical specimen confirmed the histologic diagnosis and showed the presence of perineural spread. The patient underwent adjuvant RT. (b) Axial T2 weighted MRI sequence shows no evidence of disease at 7 years after treatment
There are still “anatomic” contraindications for the use of TES in malignant tumors of the sinonasal complex. Basically, this technique is not suitable for lesions of the maxillary sinus, apart the very rare cases limited to its medial wall, and finds its main playground in naso-ethmoidal tumors. Contraindications within this group include infiltration of nasal bones and palate, massive involvement of the frontal sinus, gross invasion of the lacrimal pathway, extension into the infratemporal fossa, involvement of the orbital content, extension of dura involvement beyond the meridian of the orbit, and massive invasion of brain parenchyma. These situations require a combination of endoscopic and external approaches.
Other than the extent of tumor to critical areas, which limits the indications for TES, there are biologic features of the tumor itself, which in general suggest adopting a nonsurgical treatment strategy, such as concomitant CRT, or use of neoadjuvant chemotherapy to select the next step (CRT or surgery followed by CRT). This approach seems applicable in high-grade tumors (i.e., poorly differentiated SCC, sinonasal undifferentiated carcinoma, neuroendocrine carcinoma, NUT midline carcinoma) [135, 136], which are associated with a high risk of distant metastasis and are frequently diagnosed at an advanced local stage requiring extensive and mutilating surgery.
Twenty-five years after TES was proposed as an alternative to ACR, it is time to try to compare the two techniques with regards to survival and morbidity outcomes. However, there are factors which include the rarity of the disease, histologic heterogeneity, and the length of follow-up in relation to the propensity of some tumors to recur many years later, which made it difficult to accrue large series with sufficient follow-up to make statistically robust comparisons [130]. The three major series (Table 7.5), collected at two Italian Tertiary referral centers, at the M.D. Anderson Cancer Center in Houston, and at the Royal National Throat Nose & Ear Hospital in London, respectively, include a number of patients ranging from 120 [128] to 184 [127]. In spite of the different distribution by histology, with a prevalence of olfactory neuroblastoma in the series from the USA [128] and UK [130], and adenocarcinoma in the Italian study, the results in terms of oncologic outcomes are similar, with 5-year OS varying from 76 to 84 %, and DSS from 82 to 87 %. When morbidity is considered, it is noteworthy that complications occurred in 9–11 % of patients, and no death in the postoperative period was observed. Although the comparison with the results of the collaborative study on ACR is hindered by the different distribution of patients by stage, with a higher rate of advanced tumors in the ACR group, the reported 5-year OS and DSS of 54 % and 60 %, respectively [132], a 36.3 % complication rate, and 4.7 % mortality rate [133] suggest that ETS may favorably compete with ACR in specific indications.
Table 7.5
Characteristics of the three largest sinonasal malignant tumors endoscopic resection series to date
Nicolai et al. (2008) [127] | Hanna et al. (2009) [128] | Lund et al. (2015) [130] | |
|---|---|---|---|
Number of cases, n | 184 | 120 | 140 |
Reporting period | 1996–2006 | 1992–2007 | 1996–2014 |
Mean age, years | 59 | 53 | 63 |
Male sex, n (%) | 117 (64) | 65 (54) | 68 (49) |
Surgical approach, n (%) | |||
Endoscopic | 134 (73) | 93 (77) | 140 (100) |
Cranioendoscopic | 50 (27) | 27 (23) | – |
Prior treatment, n (%) | 52 (28) | 70 (58) | 25 (22) |
T stage, n (%) | |||
1 | 52 (28) | 30 (25) | 57 (41) |
2 | 26 (14) | 30 (25) | 27 (19) |
3 | 32 (17) | 25 (21)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |