With increasing public awareness of the risk for breast cancer and modern techniques of reconstruction, the option of surgical prophylaxis for risk reduction is becoming increasingly popular. Bilateral prophylactic mastectomy for women at increased risk of developing breast cancer and contralateral prophylactic mastectomy for those with unilateral breast cancer seeking symmetry, risk reduction, and ease of follow-up are acceptable options for many women. However, prophylactic surgery is not an inconsequential decision, and careful consideration should be given to the risks and benefits of such procedures.
Key points
- •
With increasing public awareness of risk of breast cancer and modern techniques of reconstruction, the option of surgical prophylaxis for risk reduction is becoming increasingly popular.
- •
Bilateral prophylactic mastectomy for women at increased risk of developing breast cancer and contralateral prophylactic mastectomy for those with unilateral breast cancer seeking symmetry, risk reduction and ease of follow-up are acceptable options for many women.
- •
Prophylactic surgery is not an inconsequential decision, and careful consideration should be given to the risks and benefits of such procedures.
Introduction
As women become increasingly aware of their risk of developing breast cancer, many are choosing to undergo prophylactic mastectomy as a means of risk reduction. Although it is clear that this procedure results in a significantly lower incidence rate of breast cancer, the impact on survival has been less well elucidated. For some, the psychological benefit outweighs the potential complications and for others, the desire for symmetry and reduced need for ongoing mammographic surveillance is critical to their decision making. With significant improvements in reconstructive procedures, the cosmetic outcome is acceptable to many women. Nevertheless, careful evaluation of risks and benefits are warranted when considering prophylactic mastectomy.
Introduction
As women become increasingly aware of their risk of developing breast cancer, many are choosing to undergo prophylactic mastectomy as a means of risk reduction. Although it is clear that this procedure results in a significantly lower incidence rate of breast cancer, the impact on survival has been less well elucidated. For some, the psychological benefit outweighs the potential complications and for others, the desire for symmetry and reduced need for ongoing mammographic surveillance is critical to their decision making. With significant improvements in reconstructive procedures, the cosmetic outcome is acceptable to many women. Nevertheless, careful evaluation of risks and benefits are warranted when considering prophylactic mastectomy.
Risk assessment
At the heart of prophylactic surgery is the desire to reduce risk. In this context, the need for accurate risk assessment is of paramount importance. For women with no current history of breast cancer, there are several risk factors that increase the risk of developing breast cancer. Genetic mutations, particularly in BRCA1 and BRCA2, are well known to increase a woman’s absolute risk of developing breast cancer to approximately 85%. However, there are several other genetic mutations that also increase risk ( Table 1 ). In patients with a significant family history, consultation with a genetic counselor is warranted. Even without a known mutation, patients with a significant family history may opt for prophylactic mastectomy rather than careful surveillance.
| Genetic Risk Factors | Nongenetic Risk Factors | ||
|---|---|---|---|
| Factor | Absolute Lifetime Risk (%) | Factor | Relative Risk |
| BRCA1 | 81 | Classic LIN | 7–11× |
| BRCA2 | 85 | ADH/ALH | 4–5× |
| p53 | 24 | Proliferative change without atypia | 1.9× |
| PTEN | 25 | ||
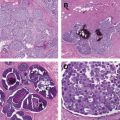
It should also be noted that there are several nongenetic risk factors that also increase a patient’s risk of developing a future breast cancer. Although most of these benign atypias and classic lobular intraepithelial neoplasias (also known as lobular carcinoma in situ) increase risk, the risk elevation is rarely so significant as to prompt women to opt for prophylactic surgery in the absence of other factors (see Table 1 ).
A variety of risk-assessment tools help to quantitate an individual patient’s risk of developing breast cancer, but each has its own limitations. The Gail model is the most often used for patients without a significant genetic risk. Though widely accepted, this model has some limitations in terms of not assessing second-degree family history and lack of widespread validation in non-Caucasian populations. Nonetheless, many risk-reducing trials have defined “high risk” as a Gail 5-year risk of 1.67% or greater. Other risk models, such as the Claus model and the Tyrer-Cuzik model, are designed to incorporate family history to a greater degree than Gail. BRACAPRO is often used to estimate the risk of carrying a BRCA gene mutation, and is used to define patients who may benefit from annual magnetic resonance imaging (MRI) screening (>20%–25% lifetime risk).
Quantitative risk estimation is important for patients who are trying to decide between risk-reducing options. For individuals at high risk, several risk-reducing options are available ( Table 2 ). Patients who present with an ipsilateral breast cancer also have an increased risk of developing contralateral breast cancer, estimated to be 0.5% to 1.0% per year. For patients who opt for an ipsilateral mastectomy, contralateral prophylactic mastectomy can reduce the contralateral risk of developing breast cancer by 96% while providing symmetry.
| Risk-Reducing Measure | Relative Risk (%) |
|---|---|
| Tamoxifen | 37 −49 |
| Raloxifene a | 56 –59 |
| Exemestane a | 65 |
| Bilateral prophylactic salpingo-oopherectomy | 53 |
| Bilateral prophylactic mastectomy | 89.5–100 |
Epidemiology and decision making
Several studies have shown a steady increase in contralateral prophylactic mastectomy rates, but data regarding trends in bilateral prophylactic mastectomy are less common. McLaughlin and colleagues evaluated the 10-year trend for mastectomy procedures in New York and found that whereas contralateral mastectomy rates have been increasing (with a concomitant decline in unilateral mastectomy), the rates of bilateral prophylactic mastectomy remain fairly low ( Fig. 1 ). However, in accord with McLaughlin and colleagues, several other investigators have found a significant upward trend in contralateral prophylactic mastectomy rates ( Fig. 2 ), although interestingly a similar trend has not been seen in Europe.
Several sociodemographic and tumor characteristics have been associated with a higher likelihood of pursuing contralateral prophylactic mastectomy. These factors include younger age, Caucasian race, private insurance, a family history of breast cancer, and lobular tumor histology. However, other factors, such as workup with bilateral breast MRI and the option of immediate reconstruction, are independently associated with the decision to pursue contralateral prophylactic mastectomy.
When surveys have asked women about their motivation to pursue contralateral prophylactic mastectomy, women often cite a desire to reduce risk and live longer. While it is clear that contralateral prophylactic mastectomy will reduce risk of developing contralateral breast cancer, the data regarding survival are more mixed. Whereas some researchers found no impact of contralateral prophylactic mastectomy on disease-specific survival, others, including Bedrosian and colleagues who looked at Surveillance, Epidemiology and End Results data, found that contralateral prophylactic mastectomy was associated with a significantly improved disease-free survival.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree