Herbs and natural agents
Illicit drugs
Prescription medications
Anti-depressants and anti-psychotics
Hormonal agents
Others
Anise
Blessed thistle
Fennel
Fenugreek seeds
Marshmallow
Nettle
Red Clover
Red Raspberry
Cannabis
Cocaine
Amphetamines
Benzodiazepines
Opiates
Selective Serotonin Reuptake inhibitors (SSRI)
Citalopram (±)
Fluoxetine (CR)
Paroxetine (±)
Monoamine Oxidase inhibitors (+++)
Tricyclic
anti-depressants (+++)
Alprazolam (±)
Buspirone (+++)
Anti-psychotics
Resperidone (+++)
Haloperidol (+++)
Clozapine (0)
Olanzapine (+)
Conjugated Oestrogen and Medroxyprogesterone combinations
Medroxyprogesterone contraceptive depot injections (Depo-Provera)
Danazol
Anti-emetics and motility agents
Domperidone (+++)
Metoclopromide (+++)
Chlorpromazine (+++)
Prochlorperazine (+++)
Cisapride (+)
H2 receptor blockers
Methyldopa (+)
Sumatriptan (+)
Sodium Valproate
Opiates
Reserpine
Verapamil
Isoniazid
What additional features in the history would increase the likelihood of a pituitary tumour as the cause of her symptoms?
Symptoms of an intracranial mass lesion including headache and visual disturbances would be suggestive. Clinical features of acromegaly may rarely be associated with pituitary adenomas that co-secrete growth hormone and prolactin. Large tumours producing prolactin may compress the normal pituitary gland leading to pituitary hormone deficiencies and their associated clinical features.
Prolactinomas are usually sporadic tumours but can occasionally occur as part of multiple endocrine neoplasia type 1; a family history of pituitary adenoma, parathyroid dysfunction or other ‘endocrine tumours’ should be sought [2].
What are the physical signs to look for?
Physical examination would include general examination, breast examination, examination of the thyroid and visual assessment. Breast examination should include inspection of chest wall to look for any skin lesions and scarring. Asking the patient to perform gentle, segmental, massage of the breast towards the nipple (in the presence of a chaperone) will often produce milk. When in doubt about the nature of discharge from the nipple, the expressed secretions can be examined under low power with a microscope. True milky secretions will contain easily seen fat globules and scanty cellular material. If microscopy proves inconclusive or contains abundant cellular material then the secretions can be sent for cytological examination. Goitre and signs of hypothyroidism should be looked for. Assessment of vision should include visual acuities, visual fields by confrontation and fundoscopy.
Case Study: Part 2
Further questioning did not reveal any positive drug history. There was no history to suggest nipple stimulation, chest wall irritation, symptoms of an intracranial mass or features of hormonal deficiency. There was no family history of pituitary or other endocrine problems. Apart from expressible galactorrhoea; examination was normal with intact visual fields and no goitre. Differential diagnosis at this stage would include many of the causes of hyperprolactinaemia listed in Tables 7.1 and 7.2.
Physiological | Pharmacological | Pathological | ||
|---|---|---|---|---|
Pituitary | Hypothalamic pituitary stalk compression/damage | Systemic disorders | ||
Coitus | See Table 7.1. | Prolactinoma | Granulomas | Primary hypothyroidism |
Exercise | Non–functioning pituitary macroadenoma | Infiltrations | Neurogenic chest wall trauma | |
Lactation | Acromegaly | Irradiation | Thoracic surgery | |
Pregnancy | Lymphocytic hypophysitis | Rathke’s cyst | Herpes zoster (thoracic) | |
Sleep | Trauma | Trauma | Chronic renal failure | |
Stress | Tumours (e.g., craniopharyngioma, germinoma, hypothalamic metastasis or meningioma) | Cirrhosis | ||
Cranial irradiation | ||||
Epileptic seizure | ||||
Polycystic ovarian syndrome | ||||
What biochemical tests and radiological investigations are needed to reach a diagnosis?
Biochemical Tests
The first step would be ruling out pregnancy with urine or serum estimation of human chorionic gonadotropins. Complete blood count, renal function, liver function test and urinalysis help exclude systemic disease. Endocrine evaluation should include thyroid function tests, prolactin, gonadotrophins and oestradiol. Prolactin estimation should not be performed immediately following breast examination. Borderline prolactin values should be reconfirmed by repeat testing because of the significant variability of prolactin levels across the day and its response to stressful stimuli. All patients with unexplained hyperprolactinaemia require MRI (magnetic resonance imaging). Serum prolactin above 2,000 mU/l is almost always associated with pituitary or sellar tumours and a prolactin >5,000 mU/l is virtually diagnostic of a macroprolactinoma.
When evaluating prolactin results the clinician needs to be aware of assay “interferences” due to the presence of macroprolactin and the “prolactin hook effect.” Macroprolactin is a complex of prolactin with IgG antibody found in about 1 % of normal individuals resulting in artificially elevated measurements of serum prolactin. Macroprolactin is a physiologically inactive complex and therefore not associated with clinical symptoms of hyperprolactinaemia. Re-assay of serum after polyethylene glycol treatment usually confirms the presence of macroprolactin. Large tumours producing exceedingly high concentrations of prolactin and this may saturate both the capture and signal antibodies in immunoassays. This is known as the “hook effect” and results from blockage of the capture antibody-prolactin-signal antibody “sandwich” formation, leading to misleadingly low prolactin values, very rarely within the normal range, in automated immunometric assays. Re-assay of diluted serum will resolve the problem leading to accurate determination of the prolactin level. Patients with galactorrhoea and apparently normal serum prolactin should have prolactin levels verified after sample dilution.
Dynamic Testing with Metoclopramide
Whilst not in routine use, this can provide useful information in patients with mild to moderate elevations in serum prolactin that may be medication related or due to a microprolactinoma too small to be seen on MRI. The intravenous administration of a dopamine antagonist in normal subjects produces a marked rise in prolactin and only a mild increase in thyrotropin stimulating hormone (TSH). Patients with a microprolactinoma exhibit a blunted prolactin response and an exaggerated TSH response.
Imaging
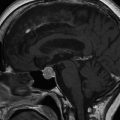
Pituitary imaging provides information about the size of the tumour and its relationship to the optic pathways; it is also useful in the follow up of patients with larger tumours. Imaging is best performed using MRI of the pituitary and hypothalamus with gadolinium contrast enhancement. For patients unable to tolerate or too large to fit in the MRI tunnel, computed tomography scanning of the pituitary can be useful but provides inferior resolution of the pituitary.
Indications for MRI pituitary would include:
Sustained hyperprolactinaemia (at any level) after other causes have been excluded.
Headache and visual field defects.
Visual Assessment
Formal visual field testing using Goldmann perimetry should be performed if the adenoma is touching or in close proximity to optic structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree