Because of the particularly high frequency of different severe forms of both α and β thalassemia in Asia, the development of approaches for their prevention and management is particularly challenging. However, because of earlier partnerships with richer countries, so-called North/South partnerships, and help from their governments, considerable progress toward the better control of the thalassemias has been achieved in some countries. It is vital that the global health importance of the thalassemias and related disorders, by far the commonest genetic diseases, is emphasized to the appropriate international health agencies.
Key points
- •
The prevention and management of the thalassemias is reasonably advanced in several countries in Asia.
- •
Partnerships are being developed between these countries and those in which facilities for the control and development of thalassemia are not yet established.
- •
There is urgent need for support on behalf of international health agencies for the further development of these programs.
Progress of thalassemia control in Thailand
Thalassemia in Thailand
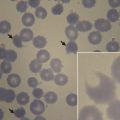
Both α-thalassemia and β-thalassemia and some abnormal hemoglobins (Hb), such as Hb E and Hb Constant Spring (CS), are prevalent in Thailand. The frequencies are 20% to 30% for α-thalassemia, 3% to 9% for β-thalassemia, 10% to 50% for Hb E, and 1% to 8% for Hb CS ( Table 1 ). Different combinations of these abnormal genes lead to more than 60 thalassemia syndromes. The 2 major alpha thalassemic diseases are Hb Bart’s hydrops fetalis or homozygous α 0 -thalassemia and Hb H disease that results from the interaction between α 0 -thalassemia and α + -thalassemia or between α 0 -thalassemia and Hb CS. Almost all fetuses with Hb Bart’s hydrops die intrautero or a few minutes after birth and their mothers often suffer from obstetric complications, such as toxemia of pregnancy (preeclampsia and eclampsia), postpartum hemorrhage due to an enlarged placenta, and the psychological burden of carrying a nonviable fetus to term. Interaction between β-thalassemia genes or β-thalassemia and Hb E genes leads to homozygous β-thalassemia or β-thalassemia/Hb E disease, which are major beta thalassemic syndromes in this region. In β-thalassemia/Hb E disease, although the patients have identical genotypes, the degree of anemia varies greatly, with hemoglobin levels ranging from 3 to 13 g/dL. The birth rates of major thalassemic diseases are shown in Table 2 .
| Major Types of Thalassemia | Frequencies, % |
|---|---|
| α-Thalassemia (α 0 -thalassemia and α + -thalassemia) | 20–30 |
| Hemoglobin Constant Spring (α + -thalassemialike effect) | 1–8 |
| β-thalassemia | 3–9 |
| Hemoglobin E | 10–53 |
| Diseases | Couples at Risk (per year) | Births (per year) | Living Patients |
|---|---|---|---|
| Homozygous β-thalassemia | 828 | 207 | 2070 |
| β-Thalassemia/Hb E | 12,852 | 3213 | 96,390 |
| Hb Bart hydrops fetalis | 3332 | 833 | 0 |
| Hb H disease | 22,400 | 5600 | 336,000 |
| Total | 39,412 | 9853 | 434,460 |
Since 2002, Thailand has implemented the Universal Health Care policy that resulted in a 99% universal coverage among Thai nationals using a mix of health protection schemes. Under this policy, all Thais will receive free treatment, either at the nearby district hospital or by referral for treatment in a medical center for cases that need special care. Almost all patients with thalassemia can have access to free blood transfusion and iron chelation, such as desferrioxamine and deferiprone. To reduce the cost of the iron chelators, the Government Pharmaceutical Organization has synthesized deferiprone for local use. The product is effective in the treatment of iron overload in all thalassemia syndromes, except major thalassemia cases that need regular blood transfusion that still need desferrioxamine treatment as a combination therapy. The estimated direct cost for the management of a patient with major thalassemia who receives regular blood transfusion and desferrioxamine treatment who lives to be 10 to 30 years old is approximately 1.3 to 6.6 million Baht (US$ 39,393–200,000). Even though thalassemia may be cured by stem cell transplantation, it is still expensive and it is difficult to find appropriate HLA-matched donors. Thus, the best approach to cope with thalassemia in developing countries, including Thailand, is to prevent the birth of new cases with major thalassemic diseases.
Progress of thalassemia control in Thailand
Thalassemia in Thailand
Both α-thalassemia and β-thalassemia and some abnormal hemoglobins (Hb), such as Hb E and Hb Constant Spring (CS), are prevalent in Thailand. The frequencies are 20% to 30% for α-thalassemia, 3% to 9% for β-thalassemia, 10% to 50% for Hb E, and 1% to 8% for Hb CS ( Table 1 ). Different combinations of these abnormal genes lead to more than 60 thalassemia syndromes. The 2 major alpha thalassemic diseases are Hb Bart’s hydrops fetalis or homozygous α 0 -thalassemia and Hb H disease that results from the interaction between α 0 -thalassemia and α + -thalassemia or between α 0 -thalassemia and Hb CS. Almost all fetuses with Hb Bart’s hydrops die intrautero or a few minutes after birth and their mothers often suffer from obstetric complications, such as toxemia of pregnancy (preeclampsia and eclampsia), postpartum hemorrhage due to an enlarged placenta, and the psychological burden of carrying a nonviable fetus to term. Interaction between β-thalassemia genes or β-thalassemia and Hb E genes leads to homozygous β-thalassemia or β-thalassemia/Hb E disease, which are major beta thalassemic syndromes in this region. In β-thalassemia/Hb E disease, although the patients have identical genotypes, the degree of anemia varies greatly, with hemoglobin levels ranging from 3 to 13 g/dL. The birth rates of major thalassemic diseases are shown in Table 2 .
| Major Types of Thalassemia | Frequencies, % |
|---|---|
| α-Thalassemia (α 0 -thalassemia and α + -thalassemia) | 20–30 |
| Hemoglobin Constant Spring (α + -thalassemialike effect) | 1–8 |
| β-thalassemia | 3–9 |
| Hemoglobin E | 10–53 |
| Diseases | Couples at Risk (per year) | Births (per year) | Living Patients |
|---|---|---|---|
| Homozygous β-thalassemia | 828 | 207 | 2070 |
| β-Thalassemia/Hb E | 12,852 | 3213 | 96,390 |
| Hb Bart hydrops fetalis | 3332 | 833 | 0 |
| Hb H disease | 22,400 | 5600 | 336,000 |
| Total | 39,412 | 9853 | 434,460 |
Since 2002, Thailand has implemented the Universal Health Care policy that resulted in a 99% universal coverage among Thai nationals using a mix of health protection schemes. Under this policy, all Thais will receive free treatment, either at the nearby district hospital or by referral for treatment in a medical center for cases that need special care. Almost all patients with thalassemia can have access to free blood transfusion and iron chelation, such as desferrioxamine and deferiprone. To reduce the cost of the iron chelators, the Government Pharmaceutical Organization has synthesized deferiprone for local use. The product is effective in the treatment of iron overload in all thalassemia syndromes, except major thalassemia cases that need regular blood transfusion that still need desferrioxamine treatment as a combination therapy. The estimated direct cost for the management of a patient with major thalassemia who receives regular blood transfusion and desferrioxamine treatment who lives to be 10 to 30 years old is approximately 1.3 to 6.6 million Baht (US$ 39,393–200,000). Even though thalassemia may be cured by stem cell transplantation, it is still expensive and it is difficult to find appropriate HLA-matched donors. Thus, the best approach to cope with thalassemia in developing countries, including Thailand, is to prevent the birth of new cases with major thalassemic diseases.
Prevention and control program for thalassemia in Thailand
A nationwide program has commenced to prevent and control homozygous β-thalassemia, compound heterozygote β-thalassemia/Hb E, and Hb Bart’s hydrops fetalis. The program started in 1997, after some preparation in technology transfer to the Minister of Public Health. Three major departments are involved in this program, namely Department of Medical Services, Department of Health, and Department of Medical Sciences. The 3 departments are involved in the prevention and control of thalassemia as follows:
- 1.
The Department of Medical Services is involved in the improvement of treatment to improve the quality of life of patients with thalassemia. The department has worked in collaboration with the Thalassemia Foundation of Thailand and Thai Hematology Society to develop a clinical practice guideline as a reference for how to manage thalassemia in Thailand.
- 2.
The Department of Health is involved more in the screening, counseling, and prenatal diagnosis under the policy “Select partner, Select pregnancy, Select birth,” which will lead to thalassemia-free infants born in the kingdom.
- 3.
The Department of Medical Science is involved in the training of laboratory technicians at various levels to learn how to screen for thalassemia carriers and high-risk couples by using both simple screening tests and standard procedures for the accurate diagnosis of thalassemia.
During 1997 through 2010 we had conducted many workshops and trained medical staff, including pediatricians, physicians, nurses, medical technologists, and technicians, in basic knowledge about thalassemia, laboratory diagnosis, and management. Declaration of the nationwide policy by the Permanent Secretary of the Ministry of Public Health for thalassemia control was announced on February 9, 2005 ( Box 1 ). We are still conducting refresher courses and have held a National Annual Meeting on Thalassemia for the past 20 years.
- 1.
Every pregnant woman should receive genetic counseling for thalassemia.
- 2.
Every pregnant woman should receive thalassemia screening by consent. If the result is found to be positive for thalassemia/hemoglobinopathies trait, the husband should be screened as well.
- 3.
Every pregnant woman and husband with thalassemia/hemoglobinopathies trait should receive a confirmation test to be a COUPLE AT RISK of having severe thalassemia offspring.
- 4.
Pregnant women who are diagnosed to be a COUPLE AT RISK should receive prenatal diagnosis.
- 5.
Every health care unit should organize a thalassemia promote/prevent/control service system that is high standard. If any service exceeds the unit capability, the case should be transferred to the service network.
- 6.
Students, reproductive women, and married couples will extensively receive the information about thalassemia.
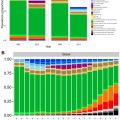
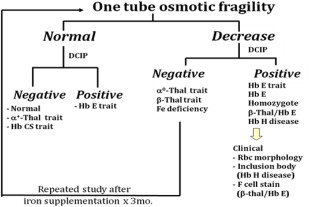
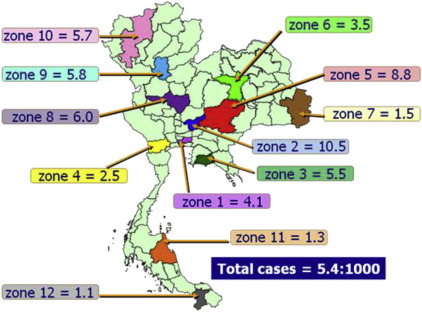
The target group for thalassemia screening is pregnant women. This is done by a simple 1-tube osmotic fragility test for β and α 0 -thalassemia carriers and Hb E by dichlorophenol-indolphenol dye test (DCIP dye test). The husband of those pregnant women who have a positive screening test will be called up for further screening. The couples that have positive screening of both husband and wife will be further referred for a confirmation test by standard methods of blood counts and hemoglobin analysis by automatic high-performance liquid chromatography (HPLC) (Variant System, Bio-Rad Laboratories, Hercules, CA) or by capillary zone electrophoresis in some centers. Fig. 1 demonstrates the schematic outline of thalassemia screening in Thailand. The result of nationwide screening for high-risk couples shows that it varies from the north to south related to the abnormal gene frequencies in each region ( Fig. 2 ). Wanapirak, Chiangmai University, has shown that the total cost of screening for high-risk couples plus the cost of prenatal diagnosis in 21,975 pregnant women and prevention of the birth of 80 severe thalassemic diseases (both α-thalassemia and β-thalassemia) is much less than the costs of treatment of these patients if they were born ( Box 2 ).
- •
Period of screening test: 8 years
- •
21,975 pregnant women have been screened
- •
The program prevented birth of 80 severe thalassemia cases
- •
Total cost of screening (husband and wife) and PND = 3091,000 Thai Baht (US$ 93,667)
- •
The cost of treatment of thalassemia patients = 222,961,250 Thai Baht (US$ 6,756,401)
The overall result of thalassemia control program at Chiangmai Medical School is summarized in Table 3 and the result of national screening cases is summarized in Table 4 . After 20 years of launching a nationwide control program for severe thalassemia, we still achieve only approximately 50% screening of pregnant women because many of them attend the antenatal care clinic late. Moreover, we still have the problem of investigating the husband because some of them work in other places, and even abroad. At the moment, we are planning to move further to perform premarital screening and screening of nonpregnant women as well.
| Year | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total screened | 2152 | 1765 | 1737 | 1504 | 1563 | 1580 | 1400 | 1269 | 1202 | 1100 | 1215 | 16,487 |
| Positive cases | 634 | 697 | 697 | 487 | 598 | 633 | 403 | 383 | 312 | 322 | 373 | 5539 |
| Couple at risk | 41 | 43 | 47 | 31 | 31 | 32 | 25 | 23 | 25 | 23 | 27 | 348 |
| Hb Bart hydrops | 13 | 12 | 12 | 10 | 12 | 12 a | 10 | 8 | 5 | 5 | 8 | 107 a |
| Homo. β thal | 7 | 8 | 6 | 3 | 5 | 4 | 2 | 3 | 3 | 2 | 4 | 47 |
| β thal/Hb E | 21 | 23 | 29 | 18 | 14 | 17 a | 13 | 12 | 17 | 16 | 15 | 195 a |
| Affected | 5 | 7 | 10 | 10 | 7 | 8 | 5 | 6 | 5 | 5 | 7 | 75 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree