A safe supply of blood and the knowledge, skill, and resources for the appropriate use of blood are essential for medical services. Many problems are faced in the development of transfusion services in low- or medium-income countries (LMICs). Unfortunately, in many countries, providing safe blood is made more difficult by a lack of blood donors and the high frequency of transfusion-transmissible infections. The problems are compounded by the frequent need for urgent life-saving transfusions. This article examines the problems in supply, safety, and use of blood and how they are being addressed in LMICs, predominantly focusing on sub-Saharan Africa.
Key points
- •
In the last 5 years, nearly all African states had a national blood policy; but just more than half have been able to implement their policies.
- •
The main obstacles to implementation are a lack of trained staff, the high cost of blood in relation to the health care budgets and recruitment of donors. In the absence of centralized services, facilities rely on blood collected by hospitals from family or replacement donors.
- •
The high rate of chronic viral infections in the populations implies that the residual risk of infection of human immunodeficiency virus and hepatitis B infection remains substantial with enzyme immunoassay testing, but there is evidence that the residual risks for these infections are decreasing.
- •
Several initiatives are being trialed to improve the supply, safety and use of blood by encouraging repeat voluntary donors, developing systems that rely more on local resources, establishing international networks across Africa for research and education and improving clinical practice through guidelines and audits of the use of blood.
Introduction
Blood transfusion is life saving and life enhancing, not only directly in emergency situations and acute or chronic illness, but also in facilitating surgery and chemotherapy that would not be possible without blood components. In high-income countries, the safety and availability of blood transfusion and the human and material resources to use blood are largely taken for granted. However, in many parts of the world the reliable supply of safe blood is far from secure.
For many reasons, blood has to be collected and used locally. It is far from being a simple medicinal product that can be ordered from a catalog. A blood transfusion for a child with malarial anemia or a woman with severe postpartum hemorrhage requires a complex social, technical, and medical infrastructure, including a pool of donors, organization of collection, testing processing of blood, and the clinical and laboratory skills to use blood. Given the complexity of this process, it is not perhaps so surprising that strengthening this chain is not a trivial exercise and by its very nature cannot be completely solved by addressing only one aspect of this process. Here, the authors examine the elements required for the most effective use of blood and how they are being developed across the world.
Introduction
Blood transfusion is life saving and life enhancing, not only directly in emergency situations and acute or chronic illness, but also in facilitating surgery and chemotherapy that would not be possible without blood components. In high-income countries, the safety and availability of blood transfusion and the human and material resources to use blood are largely taken for granted. However, in many parts of the world the reliable supply of safe blood is far from secure.
For many reasons, blood has to be collected and used locally. It is far from being a simple medicinal product that can be ordered from a catalog. A blood transfusion for a child with malarial anemia or a woman with severe postpartum hemorrhage requires a complex social, technical, and medical infrastructure, including a pool of donors, organization of collection, testing processing of blood, and the clinical and laboratory skills to use blood. Given the complexity of this process, it is not perhaps so surprising that strengthening this chain is not a trivial exercise and by its very nature cannot be completely solved by addressing only one aspect of this process. Here, the authors examine the elements required for the most effective use of blood and how they are being developed across the world.
Safety and supply
A safe supply of blood is an essential part of medical services. An unsafe blood supply is costly in both human and economic terms. Transfusion of infected blood not only causes direct morbidity and mortality, but also undermines confidence in modern health care. Those who become infected through blood transfusion may also contribute to a secondary wave of infections. Investment in safe supplies of blood is cost-effective for every country, even those with few resources. At the same time, an insufficient supply costs lives because severely anemic patients do not survive unless transfused. Where should the priority be?
The shockwave of the human immunodeficiency virus (HIV) epidemics put overwhelming emphasis on blood safety, but now the supply of blood should take back its legitimate place as a priority. An adequate and sustainable blood supply would go a long way to reducing mortality in developing countries, especially among women and children.
The World Health Organization (WHO) has identified 4 key objectives for blood services to ensure that blood is safe for transfusion:
- •
Establish a coordinated national blood transfusion service that can provide adequate and timely supplies of safe blood for all patients in need.
- •
Collect blood only from voluntary nonremunerated blood donors from low-risk populations, and use stringent donor selection procedures.
- •
Screen all blood for transfusion-transmissible infections, and have standardized procedures in place for grouping and compatibility testing.
- •
Reduce unnecessary transfusions through the appropriate clinical use of blood, including the use of intravenous replacement fluids and other simple alternatives to transfusion, wherever possible.
The WHO also emphasizes that effective quality assurance should be in place for all aspects of the transfusion process, from donor recruitment and selection through to infection screening, blood grouping and blood storage to administration to patients and clinical monitoring for adverse events.
Blood-borne infections
Local blood transfusion services encounter many problems, including lack of funding, insufficient training, poor management, frequent failure in supply of reagents and consumables, and breakdown of the cold chain (mostly related to frequent power cuts). Since 2000, a lot of investment has gone into providing HIV, hepatitis B surface antigen (HBsAg), and to some extent, hepatitis C virus (HCV) tests in Africa. In particular, there have been enormous efforts to ensure that blood collected in Africa is tested for HIV.
Blood-Borne Viral Infections
The overall prevalence of HIV antibody in sub-Saharan Africa ranges between 0.5% and 16.0%. In donors, it tends to remain less than 5% in West Africa, less than 10% in East and Central Africa and more than 10% in southern Africa.
Chronic hepatitis B prevalence, as indicated by the presence of circulating HBsAg, ranges between 5% and 25% of the population, including blood donors. This high prevalence is due to (vertical) transmission at birth or (horizontal) infection in infancy and limited national vaccination programs, indeed infection after 10 years of age is uncommon. HBsAg is more prevalent in West Africa (10%–25%) than in East or Central Africa (5%–10%), whereas the lowest prevalence is found in southern Africa (5% or less).
Antibody to HCV is not routinely screened for in many parts of Africa, but the prevalence of this infection ranges between 0.5% and 3.0% and reaches 10% to 15% in Egypt. There is evidence of geographically limited pockets of high prevalence, suggesting the importance of specific factors, such as various types of injections and past diagnostic or vaccination campaigns, contributing to the spread of infection.
Other Infections
Most countries in sub-Saharan Africa do not screen for human T-lymphotropic virus 1 (HTLV-1) because the prevalence is low (<2%). However, in other areas of the world, more than 10% of chronically transfused patients have evidence of exposure to HTLV-1. Although the risk of acquiring syphilis from infected blood is low, most blood banks in sub-Saharan Africa do screen for Treponema pallidum . Fresh blood is potentially infectious for syphilis, but storage at 4°C can inactivate the bacterium.
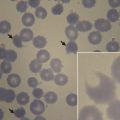
Malaria is not only the leading cause of anemia requiring transfusion across Africa but can also be transmitted by transfusion. In North America and Europe, transmission of malaria from donors who have visited malaria-endemic areas and have a subclinical patent blood stage infection can transmit the parasite, often with fatal results.
In areas of low or no malaria transmission, screening for the parasite is important, as recipients are likely to have no immunity. In countries where malaria is highly endemic, the prevalence of Plasmodium spp in donor blood is often very high (16%–55%). Excluding donors with low-grade parasitemia would reduce the supply of blood; in any event, the current methods of screening donors by blood film or rapid diagnostic tests may be insufficiently sensitive to prevent transmission of malaria. Preemptive treatment of recipients of red cells with antimalarial drugs may be a viable alternative.
Bacterial contamination of blood components is poorly recognized, although some surveys suggest bacterial infection may be present in 10% of products at the time of issue. The most common bacterial infections were due to gram-negative organisms, and the most likely source of contamination was the blood bank and not donors. More widely, the testing of components is limited by the expense of facilities for rapid detection of bacterial contamination. Assessing the scale of the problems and factors behind bacterial contamination of blood would be a priority for future hemovigilance and quality-assurance programs.
Testing blood products
Test sensitivity and coverage is critical in the face of high prevalence rates for HIV, hepatitis B virus (HBV) and HCV. Some 15 years ago, a survey of blood collection services across India showed that 87% of the donor units were screened for HBV, 95% for HIV, 94% for syphilis, 67% for malaria, and 6% for HCV. Only 13% of blood banks used enzyme-linked immunosorbent assay (ELISA) kits for HBsAg. Notification of the occurrence of transfusion-associated hepatitis was provided less than 40% of the time. There have been substantial efforts to improve the coverage and quality of testing for these viruses over the last decade.
Even with good coverage, the residual risk of all viral infections is high because of the window period of patent infection before detectable antibody, antigen or viral nucleic acid. The residual risk of HBV has always been substantial because of donations containing undetected low levels of HBsAg or occult HBV DNA. Estimates of the residual risk of HIV transmission in the preseroconversion window period were 1:2600 to 6000, hepatitis C 1:400 to 1500, and hepatitis B 1:300 to 500, when using enzyme immunoassay (EIA) screening.
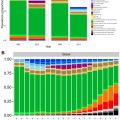
In spite of these substantial problems, the considerable international effort to improve the blood safety led by PEPFAR and the Global Fund seems now to be showing significant improvements in the number of units donated and the number of countries screening at least 95% of donations for HBV and HCV, whereas the median of national prevalence for HBV and HCV markers reactive blood donations has declined between 2004 and 2011.
The fruits of this work can be seen in the reduction in HCV prevalence over time in cohorts of chronically transfused patients across Africa. Some more recent estimates for the residual risk for HIV for Zimbabwe are 1:7500 units for first-time donors and 1:5500 for repeat donors. In Gabon, the current residual risks are HIV 1:16,000, HCV 1: 4800 and HBV 1:2000, again showing a broad improvement when compared with previous estimates from Africa.
Across the world there is increasing concern over the transmission of West Nile virus and in Asia and Latin America concern about infection with dengue and chikungunya viruses through blood products. These mosquito-borne infections (or arboviruses) are of wide concern for global transfusion practice as asymptomatic, but viremic donors, may transmit infection through blood products. Furthermore, the diseases may spread to areas with suitable mosquito vectors in tropical and subtropical zones and by travelers to nonendemic countries.
Since 2003, all donations in the United States are tested for West Nile virus by nucleic acid testing. There is less certainty over what measures should be used to prevent arboviral transfusion-transmitted infection in epidemics. During epidemics of dengue, screening for donors at risk, donor tracing, and a 7-day quarantine of blood components at risk were undertaken to reduce the risk of viral transmission. In Reunion during the chikungunya epidemic in 2006, the French Blood Service interrupted blood donations on the island, except donations for platelets, whereby they implemented systematic screening for the virus by nucleic acid testing (NAT).
Supply and usage
Blood Donors
Recruiting voluntary donors from the community is complex and expensive and depends on regular education programs, collection teams, vehicles and cold storage. It is proving problematic to expand the number of volunteer donors. Some difficulties remain in persuading donors to donate in the light of HIV testing. There are also cultural beliefs surrounding blood donation that inhibit donors coming forward. Some of these seem to be misinformation about donating blood (eg, men will become impotent if they donate blood; HIV can be caught from the blood bag needle). There are, however, other cultural beliefs related to understanding the value of blood to the individual and to society, for example, blood is related to kinship or personal health. Understanding local beliefs surrounding blood and blood donation is likely to be important in developing effective services. It is worth noting that similar problems were a barrier to widespread acceptance of blood donation in London more than 70 years ago.
As volunteer donors are in short supply, family members are frequently used to provide blood for their relatives in hospital. In 2002, in Africa as a whole, WHO estimated that more than 60% of blood originated from replacement/family donors. In sub-Saharan Africa, the proportion of blood derived from replacement donors is certainly higher. Most viral infections, such as HIV, HBV, and HCV, have similar prevalence in age-matched replacement and volunteer donors. Nevertheless, in Brazil, one-third of donors who were seropositive for syphilis came to the blood bank to help a friend or a relative who needed blood. Although they reported and recognized some high-risk behavior, most were motivated by direct appeal to donate blood. The ultimate aim should be to maximize conversion of voluntary and replacement donors into regular donors because those who are successful repeat donors have the best safety profile.
Notwithstanding the problems in recruiting donors from the community, there is still an argument that a centralized community-based blood service is a necessity to ensure that there is an adequate blood supply to meet clinical demand. Reliance on family replacement donors does not yield sufficient blood units; therefore, there needs to be a dedicated effort to collect from voluntary nonremunerated donors in the community.
Use of Blood Products
In contrast to higher-income countries, most transfusions in sub-Saharan Africa are given for life-threatening emergencies. Transfusions are administered to children predominantly for malaria-related anemia. Many clinical guidelines suggest that transfusions for children are indicated if hemoglobin (Hb) less than 40 or 50 g/L with symptoms of decompensation ( Table 1 ). The evidence is that children with severe anemia (Hb <50 g/L) who are not transfused have a high chance of dying, often soon after admission. In a recent study in East Africa, 52% (54 of 103) of severely anemic children who were not transfused died within 8 hours, and 90% of these deaths occurred within 2.5 hours of admission. Anemia is an independent risk factor for death during admission; by 24 hours, 128 of 1002 (13%) severely anemic children had died, compared with 36 of 501 (7%) and 71 of 843 (8%) of those with moderate and mild anemia, respectively.
| Indications for Transfusion | Volume and Speed of Transfusion | ||
|---|---|---|---|
| Hb Level (g/L) | Clinical Symptoms | ||
| WHO Pocket Book of Hospital Care for Children (2005) | 40 or less OR 60 or less PLUS 1 or more | Not required Deep and labored breathing Cardiac failure Clinical dehydration or shock Impaired concentration Malaria parasitaemia >10% | 20 mL/kg whole blood or 10 mL/kg packed cells over 3–4 h |
| Kenya Guidelines for Appropriate Use of Blood and Blood Products (2004) | <40 OR <50 PLUS | Not required Respiratory distress | 20 mL/kg whole blood over 3–4 h |
| Ugandan National Guidelines (2010) | 40 or less OR 60 or less PLUS 1 or more | Not required Hypoxia Cardiac decompensation Acidosis Impaired consciousness or cerebral malaria Septicaemia Meningitis Malaria parasitaemia >20% | 20 mL/kg whole blood or 10 mL/kg packed cells over 3–4 h |
| Tanzania National Malaria Guidelines (2006) | 40 or less OR 60 or less PLUS | Not required Cardiac failure | 20 mL/kg whole blood or 10 mL/kg packed cells over 3–4 h |
Pregnant women are the second most common recipients of blood, particularly for hemorrhagic emergencies. Hemorrhage during pregnancy or at the time of delivery may contribute to a significant proportion of maternal deaths. In Botswana, a review of the causes of maternal deaths suggested that hemorrhage contributed to 40% of deaths, and overall two-thirds of the women who died were HIV positive. Risk factors for transfusion in pregnancy include not only hemorrhage but also prenatal anemia, lack of prenatal care, gestational age of less than 34 weeks at delivery and HIV infection.
Although improved transfusion services would be an important component of strategies to reduce maternal mortality, they are not sufficient on their own. In many countries, a comprehensive emergency obstetric and neonatal care, that provides a continuous service, is still only available in a minority of regional and district hospitals. The picture of current care suggests that there is a real need to integrate hematology and blood transfusion, HIV management and antenatal care if substantial progress is to be made in reducing the terrible burden of maternal mortality in low- and middle-income countries (LMICs).
Significant quantities of blood are also used in trauma, often related to motor vehicle accidents, surgery and general medicine. There are neither systematic reviews nor international guidelines covering the use of blood and blood products in these specific contexts and few audits of blood use. The scope for improving clinical practice and reducing unnecessary transfusion is probably substantial.
The success of chronic blood transfusion in the primary and secondary prevention of stroke in sickle cell disease has significantly improved the outcome for severe sickle cell disease in Europe and North America. However, implementing these life-enhancing regimes in Africa faces substantial challenges, including costs, unreliable and insufficient supply of blood for elective procedures, cultural beliefs, and the high frequency of transfusion reactions. Hydroxyurea may offer a more viable route not only for the management of severe sickle cell disease but also to reduce transfusion requirements in thalassemia intermedia.
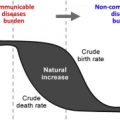
As LMICs improve their public and primary health care, chronic medical illnesses, such as cardiac disease, diabetes and cancer, become more of a priority for health care needs. To be able to provide therapies for these disorders, especially for cancer, transfusions are needed to support patients through bone marrow suppression. Unfortunately, in some instances, the unreliability of the supply of whole blood and blood components to support elective blood transfusion may force treating physicians to choose less rigorous chemotherapeutic regimens, which can affect long-term outcomes. Initiatives to improve cancer care and cardiac surgery in LMICs must also include attention to blood supply and safety to support patients through intensive treatments.
Systems
Taken together, small numbers of volunteer blood donors, a frequently fragile cold chain, and difficulties with pathogen testing, lead to low stocks of blood and blood products that ultimately affect patient care and outcomes. Patients in poorer countries usually present late in the course of their disease, and the need for urgent transfusion coupled with shortages of blood, mean that patients may die before a blood transfusion can be organized. In situations where blood must be donated by relatives before a patient can be transfused, several hours or even days can elapse. The process can be speeded up if relatives are asked to donate after patients have been transfused with blood from the hospital’s stocks. In this way a combination of voluntary donations to maintain some emergency stocks, combined with posttransfusion donations from patients’ relatives, may provide a practical solution to blood shortages.
Even in tertiary centers, many patients with anemia die within a few hours of admission before they can be transfused. Ten years ago, one clinical research center reported the average wait for blood transfusion in children with severe anemia to be 6 hours. Last year, a recent survey of clinical practice during trial of fluid replacement showed that 82% of children with severe anemia were transfused within 8 hours.
Focus on Sub-Saharan Africa
It is axiomatic that transfusion medicine should be incorporated into national health plans. The WHO has provided a recommended structure of national blood transfusion services. They suggest that at the national level the transfusion service should have a medical director, an advisory committee, and clear national transfusion policies and strategies with the appropriate statutory instruments to ensure the national co-ordination and standardization of blood testing, processing and distribution. Notwithstanding these recommendations, transfusion activities must be integrated with other services at local and national levels.
There has been some progress to realize the WHO’s recommendations for a national blood program. In Africa in 2002, the WHO estimated that among the 46 member states in the African continent, only 14 had a national blood policy and just 6 had a policy to specifically encourage and develop a system of voluntary nonremunerated donation. In the most recent survey in 2007, 40 out of 41 of the African states surveyed had a national blood policy; but only 56% (23 out of 41) countries were able to implement their policies.
It is worthwhile reflecting on why the development of national transfusion services has not been achieved. A key reason is that it is expensive and logistically complex. Management skills to run such services are insufficient and the cost of blood transfusion is high in relation to disposable income and health care budgets.
When a transfusion service is provided by individual hospitals, it places an enormous burden on laboratory resources. One survey showed that in a typical district hospital in southern Africa, the overall cost of the transfusion service, including consumables, proportional amounts for capital equipment, staff time, and overheads, was 36% of total laboratory costs. In hospital-based systems that depend on replacement donations, it is the patients’ family that bears the cost of donor recruitment.
The cost of a national service is even greater because of the additional costs of quality assurance, local education programs, dedicated collection teams, vehicles, and cold storage. In addition, a national service has to solve the very real practical problems of maintaining regular distributions of blood to remote facilities. A unit of blood in a centralized service costs around 4 times as much as one from a hospital-based system that uses family replacement donors (this cost does not include capital costs). Blood is, therefore, an expensive commodity in relation to the annual per capita budget for health care in these countries; it remains to be seen if blood costing more than $50 per unit when produced in centralized, externally funded units is sustainable. Precise cost-benefit analyses for the use of blood have not been done.
A perennial problem in health care systems is the availability of skilled technical staff; this may be compounded by internal migration of technical staff from hospitals to national or regional centers. There is a severe lack of training and career advancement opportunities for technical and clinical blood service staff. Training programs to increase capacity for the processing, testing, and issue of blood are, therefore, an integral part of service development.
Improvements
Putting the World Health Organization Objectives into Practice
In middle-income countries in Asia, many countries have established national blood services. For example, the Iranian Blood Transfusion Organization was established in 1974 as a national centralized organization to supply blood products free of charge to both public and private hospitals. With external assistance from Germany, Pakistan has moved to establish national and provincial blood transfusion programs.
In sub-Saharan Africa some countries have used external funds to establish an integrated national service; but few have been able to make the transition to a sustainable, national transfusion service in the absence of external funding, and even fewer have been able to reach an adequate blood supply. However, some recent success has been achieved in developing a transfusion service in several centers in Nigeria (see later discussion). The alternative is that transfusion services have to be optimized within the existing general hospital budget. Whatever sums are available, the problems surrounding the supply, safety, cost, and use of blood must be addressed. There has to be a balance between providing an ideal, integrated national service and the more pragmatic solutions afforded by local services.
Development of a National Transfusion Service in Nigeria
In 2004, Nigeria, a country of more than 140 million people, had a highly fragmented hospital-based transfusion system, with little co-ordination from the central government. Most donated blood collected was from replacement and paid donors. Testing for transmissible disease markers was inconsistent and poorly controlled. The practice of family replacement donors in a hospital-based blood service was, at that time, the most economical option; but in the face of high child and maternal mortality rates, the blood supply was insufficient. There was, therefore, the need to change practice.
The Safe Blood for Africa Foundation with a grant from US Agency for International Development and later the President’s Emergency Plan for AIDS Relief (PEPFAR) established a demonstration blood service in the capital, Abuja. This service collected blood from voluntary unremunerated donors in the local community. The blood was tested for HIV, hepatitis B and C, and syphilis and distributed to the local hospitals. A simple, but effective, quality management system was established with standard operating procedures written and followed. The objective of this project was to be the model for other centers throughout the country.
Subsequently, the Federal Ministry of Health established 6 zonal transfusion centers under the umbrella of the National Blood Transfusion Service. In addition, 10 states opened transfusion centers; there is one that serves the needs of the military forces. The Federal Ministry of Health also established an expert committee, which drafted a national blood policy and national guidelines for the standards for the practice of transfusion in Nigeria. The Safe Blood for Africa Foundation has, to date, provided technical assistance for the establishment of these centers and provided training to the staff in all elements of transfusion.
The major problem was to recruit blood donors. The youth were encouraged to donate with the establishment of a Club 25 program for donors less than 25 years of age. There was active promotion through the media, and it was highlighted by a televised donation by the president on the occasion of the official opening of the Abuja center. A problem encountered was the high number of donors presenting with Hb levels less than the required standard of 125 g/L. This problem is probably a reflection of the poor health status within the community.
Improving the Blood Supply
Careful donor selection is crucial not only to improve the supply of blood but also to reduce transfusion-transmitted infection risk. The selection of volunteer donors from lower-risk populations is considered the most effective approach, and considerable effort has been devoted to promoting voluntary, repeat donations. In practice, these are often secondary school students with median age ranging between 16 and 20 years. They are younger and have a greater proportion of females than replacement donors; but there are some concerns that, although these younger donors have a lower prevalence of transfusion-transmitted infections than older donors, they may have a higher incidence of new infections. Experience has shown that, although recruiting volunteer donors in schools can be relatively straightforward, making them into repeat donors is difficult and expensive. Encouraging both volunteer nonremunerated and family replacement donors to donate blood repeatedly is the challenge for sub-Saharan African blood services in order to provide safer blood.
Several strategies have been devised to encourage repeat donors and, thus, reduce the risk of virus carriage. In Zimbabwe, the Pledge 25 Club, a program using education and incentives to attract school students to give blood 25 times, has been successful. Similar, less ambitious schemes, for example, a Club 5, could also be effective. The WHO slogan of “Safe Blood Starts with Me” has also resulted in educational programs around the world. These schemes can be complemented by strategies to recruit donors from faith-based organizations or collaborating with radio stations to organize and promote blood donations. Specific strategies intending to encourage family replacement donors to become repeat donors are being developed.
The best use of fluid replacement, pressure devices, and pharmaceuticals, such as tranexamic acid for severe hemorrhage, are under study. The landmark CRASH-2 study (Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage-2) showed that after major trauma the antifibrinolytic tranexamic acid, given within 3 hours of the initial trauma as a loading dose 1 g over 10 minutes then infusion of 1 g over 8 hours, reduced all-cause mortality by 10%.
Several studies have shown the use of placental blood to prevent neonatal anemia, particularly in malarious areas. The high hematocrit from the placental blood and easy availability may make it suitable for small-volume emergency transfusions. However, the logistics and infrastructure needed to collect placental blood free of bacterial contamination, to obtain consent from women in labor and test and distribute these small volumes of blood, should not be underestimated.
Improving Screening for Blood-Transmitted Infections
New approaches to blood donor testing for transfusion-transmitted diseases have been adapted to local situations. Rapid immunochemical tests are being developed for blood-borne pathogens and may cut the cost of predonation and postdonation testing to a tenth of present costs. Many rapid diagnostic tests (RDTs) for anti-HIV and HBsAg are available, although fewer for anti-HCV; but sensitivity and specificity, ease of use, and cost vary greatly. The WHO has established systematic evaluations of both EIA and rapid tests to guide developing countries in their choice of tests. The current reviews of rapid diagnostic tests using immunochromatography have shown the limitations of these tests for screening for HIV, HBV, and HCV. Operator errors may be improved through training; but many rapid diagnostics tests (RDTs), especially hepatitis B rapid assays, are less sensitive than the respective EIAs; this must question the suitability of rapid diagnostic test as the sole test, particularly where the prevalence of these viral infections is high.
Nucleic acid testing (NAT) is highly effective and has been introduced in South East Asia, South Africa, Brazil, and a few centers elsewhere. The efficiency of individual-donation and mini-pool NAT is driven by the size of pool of samples treated. Widespread use of NAT is out of reach for most countries; cheaper, simpler methods to perform NAT testing would be useful. However, a recent rapid amplification method for quantization of HIV load has produced equivalent results to the current gold standard methods. Large-scale evaluation of these and similar tests is now planned.
Another approach to improve the sensitivity of HIV ELISA testing in the absence of NAT screening has been to use 2 HIV ELISA tests in parallel. This approach has prevented a substantial number of HIV-infected donations from entering the Chinese blood supply, at the cost of discarding many false-positive donations. Test performances of all tests may be improved by the development of an external quality-assurance scheme.
Blood safety has often focused on the risk of viral infection in donors, but bacterial contamination of units is also a substantial problem. Two studies have highlighted the considerable risk of bacterial infection in nearly 10% of whole blood units. Contamination seems to be of environmental, rather than of donor, origin and reducing these hazards will be an important challenge in the future.
Meeting the Financial Requirements of Transfusion Services
The challenge for poorer countries is that enough safe blood should be available for health services and individuals even when resources are extremely limited. The high cost of providing blood makes it impossible to recoup the cost of blood by user fees alone, and blood services will require internal or external public funding for the foreseeable future. Developing systems that rely more on local resources means that in the long term they may be more flexible, productive and sustainable.
Improving the Clinical Use of Blood
Monitoring and improving the appropriate use of blood is crucial to preserve the supply of blood and to improve patient care. The scope for improvement in clinical practice is great. For example, strict enforcement of a transfusion protocol in a Malawian hospital reduced the number of transfusions by 75% without any adverse effect on mortality. Even in a trial setting, the WHO’s or local guidelines for the transfusion of acute anemia in children (see Table 1 ) are frequently breached. As the scope of transfusion in LMICs expands into nonemergency settings, there is perhaps not surprisingly emerging evidence of inappropriate use of platelets or of neonatal transfusions.
Reduction in blood use has been achieved in Africa by improved or modified surgical techniques or cell salvage. In other circumstances, transfusion procedures can be adapted to local circumstance, for example, the use of exchange transfusion when leukapheresis or plasmapheresis is not available.
The use of guidelines can reduce unnecessary transfusions, and many institutions in sub-Saharan Africa and Asia have developed guidelines to promote rational use of blood transfusions and blood components. The principles underlying most transfusion guidelines are similar and combine a clinical assessment of whether patients are developing complications of inadequate oxygenation, with measurement of their Hb (as a marker of intracellular oxygen concentration). In the United States, anesthetists suggest that transfusions are almost always indicated when the Hb concentration is less than 60 g/L, whereas in many sub-Saharan African countries transfusions are recommended for children at Hb concentrations less than 40 g/L, provided there are no other clinical complications. Moreover, the lack of fractionated blood products and the reliance on whole blood should be considered in context. Using whole blood for many of the common emergent indications for transfusion in Africa may be advantageous, as it supplies critical coagulation factors for patients facing hemostatic challenge, such as in the setting of postpartum hemorrhage and following a significant trauma.
Ensuring that the transfusion guidelines are implemented is extremely difficult without formal monitoring and auditing systems. This issue is particularly problematic if the quality of Hb measurements is not assured as clinicians may rely entirely on clinical judgment to guide transfusion practice with an inevitably high proportion of inappropriate transfusions. As the cost of providing a unit of blood is approximately 40 times the cost of a quality-assured Hb test, investment in improving the Hb testing is likely to not only improve practice but also reduce transfusion costs.
Hospital transfusion committees have been an important part of improving transfusion practice in higher-income countries; now such committees have begun to spread in LMICs and started to develop policy and guidelines in tertiary centers in Kumasi, Ghana and elsewhere. One important function of these committees is to review and prevent adverse events, although they are grossly underreported in passive hemovigilance schemes. However, prospective studies suggest that adverse events are more common in resource-poor settings. National hemovigilance schemes are exceptional, but have been established in Namibia and Burkina Faso.
Within the hospital blood bank, the ability to supply blood rapidly is a priority given the high proportion of blood required for medical and obstetric emergencies. There are encouraging reports of the rapid provision of blood for emergency use in district hospitals with a time of 1 hour from requisition to supply, which would be a worthwhile and achievable target for supply of blood.
There are many developments in improving the supply and safety of blood, and the serologic side of transfusion has often been benignly neglected. Alloimmunization rates have been reported to be between 5% and 30% in multi-transfused patients. In some settings, the clinical significance of regional differences in the frequency of minor alleles of the major blood group systems is now being explored.
The complex blood group antigen genotypes and phenotypes in Africa, particularly of the Rh system, suggest that more detailed typing of variants of the RHCE gene in patients (5.5% prevalence of variants across Africa) and in donors, RH54 (DAK) (frequency of 8.1%) may be valuable when more detailed, large-scale blood group phenotyping is possible.
In China, a careful study of 140 women with the partial DEL has shown that they are at risk of alloimmunization to the D antigen and that they require RhD immunoglobulin prophylaxis. Women expressing the partial DEL should receive only RhD-negative red blood cells (RBCs), whereas patients with DEL with complete expression of antigen can safely receive RhD-positive RBCs.
The technical infrastructure and skills needed to screen patients for alloantibodies and to provide antigen-negative blood is frequently absent in many countries and regional centers in sub-Saharan Africa. Developing reliable panels of screening cells and reagents locally and providing the requisite training and establishing quality-assurance schemes may be feasible developments with external support.
The Ebola Pandemic in West Africa
The outbreak of the Ebola virus in 3 West African countries caused loss of life to many thousands of people. At the time of the outbreak, there was no proven therapy for the disease; however, 40% to 65% of patients made a full recovery. Those who survived have a developed immunity, and it has been hypothesized that antibody-containing plasma recovered from these individuals could be used as a passive therapy for Ebola-infected patents. The epidemic has highlighted the needed for well-organized hospital services. It may be that blood centers could play a significant role in providing treatment if it is proven that plasma, harvested from convalescent patients, is efficacious in the treatment of acutely ill patients; trials to test this were set up during the recent epidemic.
Research Directions in Transfusion Medicine
International policies and guidelines for blood transfusion, including blood donation, screening, clinical practice, and service organization, are based on experience from, and evidence generated in, high-income countries. Consequently, they are not necessarily appropriate for poorer countries. To improve the effectiveness of their internal operations, blood services need to be constantly conducting their own research, for example, to validate new kits or equipment or to change donor recruitment strategies. However, blood services invest very little in developing research skills among their staff and even less in conducting research that is of international quality and that could be shared across different services.
Most published transfusion-related research has been heavily biased toward transfusion-transmitted infections, particularly HIV. However, the major problem facing many blood services in poorer countries is blood shortages; but good-quality research exploring strategies for innovative donor recruitment and improving the effectiveness of clinical use of blood and economic aspects of transfusion is extremely limited.
There is increasing interest in research, audit, and collaboration in Africa and Latin America in addition to well-established postgraduate teaching in South Africa, Nigeria and Tanzania, to name but a few examples. Both the Anglophone and Francophone Transfusion Research Groups have multinational research programs.
Some key research needs of transfusion services identified at a workshop in Africa in 2015, which are likely to be relevant for other resource-limited settings, were an in-depth understanding of pragmatic and culturally sensitive approaches to blood donor recruitment; good evidence of the costs and effectiveness of different blood service models; and the critical need for appropriate information technology systems to manage and optimize blood stocks and blood donor recruitment and tracking. Transfusion research into the complex issues of systems, costs and models of sustainable funding is virtually nonexistent but is essential to guide the design and operation of cost-effective and feasible blood services in poorer countries.
For all of these, research needs to be addressed; not only does research capacity within blood services need to be improved but also the national and international societies for blood transfusion and the blood transfusion leadership in the WHO need to be strengthened to facilitate coordination, knowledge exchange, and evidence-based policy making.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree