Fig. 21.1
Ports placement. Three 12-mm trocars are used for ports
Detailed Procedure: Intracorporeal Delta-Shaped Anastomosis (Video 21.1)
Due to advances in technology and surgical techniques, the use of extracorporeal anastomosis is gradually shifting toward intracorporeal anastomosis. Several techniques for intracorporeal Billroth I anastomosis using a linear stapler, circular stapler, or hand-sewing technique have been reported in the literature. Among them, a linear stapler has several advantages over the other methods. It requires only a 12-mm trocar, which is easy to handle, and has three staple lines, which is thought to be more secure than the two staple lines created by a circular stapler.
There are several linear stapler techniques: the delta-shaped anastomosis [6], the triangulating-stapling technique [7], the bookbinding technique [8], and the linear gastroduodenostomy [9]. The delta-shaped anastomosis is a representative of intracorporeal Billroth I anastomosis, which is a functional end-to-end gastroduodenostomy technique using linear staplers [6, 7, 9, 10]. Here, we describe the delta-shaped Billroth I anastomosis because it is the most popular and is easier technically (Table 21.1):
Get Clinical Tree app for offline access

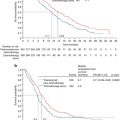
Table 21.1
Brief summary of published reports on intracorporeal Billroth I anastomosis
Author | Year | Staplers | The details of Billroth I anastomosis | Number of cases | Complications | Conclusions |
|---|---|---|---|---|---|---|
Kanaya et al. [6] | 2002 | Linear | Delta shaped | 9 | No complications as a result of the anastomosis | Safe and feasible |
Kim et al. [11] | 2008 | Linear | Delta shaped | 25 | 12 % (n = 3) | Safe and feasible |
1 anastomotic leakage, 1 anastomotic stenosis, and 1 delayed gastric emptying | ||||||
Tanimura et al. [12] | 2008 | Linear | Triangulating stapling | 81 | 1 anastomotic leakage | Safe and feasible |
Song et al. [13] | 2008 | Linear | Delta shaped | 20 | 1 intra-abdominal bleeding | Shorter bowel recovery than extracorporeal anastomosis |
Kinoshita et al. [14] | 2011 | Linear | Delta shaped | 42 | 14.3 % (n = 6) | Faster recovery than extracorporeal |
No leakage | ||||||
2011 | Linear | Delta shaped | 339/239 | 3.9 % (n = 9) | Better early surgical outcomes than extracorporeal anastomosis, especially in obese patients | |
2 anastomotic leakage, 1 anastomotic bleeding | ||||||
3.5 % (n = 12) | ||||||
1 anastomotic leakage, 1 anastomotic bleeding | ||||||
Kanaya et al. [17] | 2011 | Linear | Delta shaped | 100 | 1 minor anastomotic leakage | Mean follow-up 54.9 months, satisfactory outcomes |
Lee et al. [18] | 2011 | Linear | Delta shaped | 26 | 3.9 % (n = 1) | Feasible and safe |
1 anastomotic bleeding | ||||||
Omori et al. [19] | 2012 | Circular | Delta shaped (single-incision laparoscopic distal gastrectomy) | 20 | No postoperative complications | Safe and feasible |
Ikeda et al. [8] | 2013 | Linear | Bookbinding technique | 10 | No complications | Feasible and safe |
Omori et al. [10] | 2013 | Linear | Triangulating stapling (single-incision laparoscopic distal gastrectomy) | 45 | No anastomotic complications | Safe and feasible |
1.
Liver retraction
A.
Because the left lobe of the liver overlies most of the lesser curvature of the stomach and the lesser omentum, liver retraction is absolutely necessary for a TLDG and intracorporeal anastomosis.
B.
Begin by penetrating a 2-0 straight Prolene needle into the abdomen just below the xiphoid in the midline (on the left side of the falciform ligament). Then, insert the needle from the peritoneal cavity to the outside of the body at the right upper epigastrium (on the right side of the falciform ligament). Clip the middle portion of the suture twice with a mid pars condensa. A gauze is placed between the liver and the suture to protect the liver. Both ends of the suture are pulled and are grasped snugly over the skin of the anterior abdominal wall with a mosquito clamp. This results in a V-shaped sling that retracts the liver cranially and anteriorly (Fig. 21.2) [20].
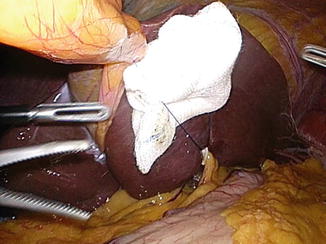
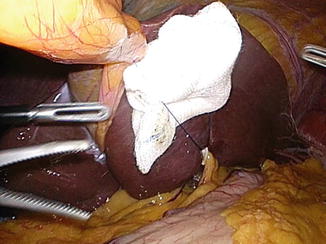
Fig. 21.2
Combined retraction of the falciform ligament and the left lateral lobe of the liver
2.
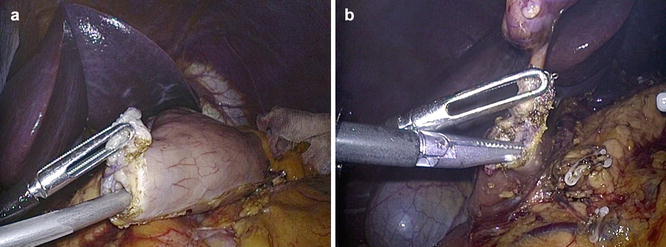
Duodenum transection (Fig. 21.3)


Fig. 21.3
Duodenum transection in a vertical direction through the 12 mm port of assistant
A.
After mobilization of the gastroduodenum, the duodenum is transected just below the pylorus using a linear stapler (blue or purple cartridge). A sufficient length of duodenum is required. To make the duodenal stump, a Kocher maneuver is sometimes required prior to the anastomosis to minimize tension on the anastomosis. Clearing adhesions on the transverse colon, hepatoduodenal ligament, gallbladder, and pancreas head is recommended
B.
The stapler is introduced through the left lower 12-mm port with the stapler directed posteroanteriorly instead of the usual craniocaudal direction. (Its direction is rotated 90° compared to the usual position. This can facilitate a favorable blood supply to the anastomosis and provides a wider space for the manipulation of the anvil side of a 45-mm linear stapler.
C.
Check the color of the duodenal stump. If the blood supply to the duodenal stump is poor, immediately convert to a Billroth II or Roux-en-Y gastrojejunostomy after using an additional linear stapler to transect the duodenal portion receiving the poor blood supply.
3.
Tumor localization and stomach transection
A.
After complete D1+ or D2 lymphadenectomy is performed, the stomach is transected. If the tumor is located below the angle, the proximal stomach is transected immediately above the angle without checking the location of tumor.
B.
If the tumor is located above the angle of the stomach, it is difficult to make an accurate proximal resection line because the lesion cannot be palpated or visualized. In this case, the location of lesion can be confirmed by intraoperative endoscopy or comparing the location between the endoscopic clips and the laparoscopic clips using intraoperative X-ray [21, 22].
C.
The proximal stomach is transected from the greater curvature by linear stapler (blue or gold or purple cartridge). Two linear staplers are enough to transect the stomach in most cases.
4.
Specimen delivery and check of the resection margins
A.
The specimen is removed through the extension of the umbilical port after placing it in a plastic bag. The plastic bag allows the prevention of wound infection and potential implantation of tumor cells. In most cases, a 3–4-cm-long skin incision with a wound protector is sufficient to deliver the specimen.
5.
Stomach opening (Fig. 21.4)