© Mayo Foundation for Medical Education and Research 2016
Ann E. Kearns and Robert A. Wermers (eds.)Hyperparathyroidism10.1007/978-3-319-25880-5_1515. Primary Hyperparathyroidism in Pregnancy
(1)
Division of Endocrinology, Diabetes, Metabolism, and Nutrition, Department of Internal Medicine, Mayo College of Medicine, Mayo Clinic, Rochester, MN, USA
(2)
Department of Surgery, Mayo College of Medicine, Mayo Clinic, Rochester, MN, USA
Keywords
Primary hyperparathyroidismMultiple endocrine neoplasia type 1HypercalcemiaPregnancyParathyroidectomyCase Presentation
A 23-year-old pregnant woman was referred for management of primary hyperparathyroidism (PHPT) in the setting of multiple endocrine neoplasia type 1 (MEN1). Shortly after becoming pregnant, the patient’s calcium was found to be 11.4 mg/dL. At the time of presentation, she was at 23-week gestation with the following laboratories: serum calcium, 10.2 mg/dL (nl, 8.9–10.1); phosphorus, 2.9 mg/dL (nl, 2.5–4.5); normal creatinine; and PTH, 45 pg/mL (nl, 15–65).
Her father and one of her three sisters also had MEN1, manifested by pancreatic neuroendocrine tumors, PHPT, and a pituitary tumor in her sister. She had been diagnosed with MEN1 by genetic testing (exon 10 Arg 527 stop) 6 years prior to pregnancy and was found to have associated PHPT. At that time, her serum total calcium was 10.5 mg/dL (nl, 9.1–10.3), phosphorus was 3.1 mg/dL (nl, 2.5–4.5), parathyroid hormone (PTH) level was 40 pg/mL, and creatinine was 0.7 mg/dL. Nuclear parathyroid scan showed mild focal increased uptake at the lower pole of the left thyroid lobe and posterior to the right thyroid lobe, consistent with small parathyroid adenomas. She had normal bone mineral density and no history of nephrolithiasis and denied symptoms of hypercalcemia such as polydipsia, polyuria, nausea, anorexia, constipation, pain, and neuropsychiatric changes, so the decision was made to forego surgery and monitor her serum calcium every 6 months.
Other studies done at that time of her initial diagnosis of MEN1 included a magnetic resonance imaging (MRI) of the brain with and without contrast with inclusion of a sella protocol, which was normal. A computed tomography (CT) scan of her abdomen with biphasic imaging of the pancreas was also unremarkable. She had normal gastrin, chromogranin A, human pancreatic polypeptide (HPP), glucagon, insulin-like growth factor 1 (IGF1), and prolactin levels.
Assessment and Diagnosis
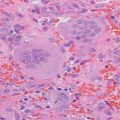
Neck ultrasound showed a 7 × 3 × 5 mm hypoechoic oval nodule posterior to the right thyroid and a 4 × 2 × 3 mm nodule inferior to the left thyroid lobe, suggestive of possible parathyroid adenomas. An obstetrical ultrasound was normal with an estimated gestational age of 20 weeks and 6 days. Maternal fetal medicine recommended fetal heart rate monitoring before and immediately after surgery. They also suggested she be positioned with left lateral tilt during surgery to avoid vena cava compression and possible compromise to uterine blood flow. Finally, they felt her risk of preterm labor was remote and hence, did not recommend delaying surgery for antenatal steroids for fetal lung maturity.
MEN1 is an autosomal dominant condition caused by mutations in the tumor suppressor gene MEN1, which classically predisposes affected patients to tumors involving the parathyroid glands, anterior pituitary, and pancreatic islet cells. Carcinoid, adrenal cortical tumors, facial angiofibromas, collagenomas, and lipomatous tumors can also develop in MEN1. PHPT due to parathyroid adenomas is the most common manifestation of MEN1, occurring in 90 % of patients [1]. Compared to patients with sporadic PHPT, patients with MEN1-associated hyperparathyroidism usually present at an earlier age (second to fourth decade vs. sixth decade), have an equal male-to-female ratio (1:1 vs. 1:3), and have lower bone mineral density [2]. Many of these patients are diagnosed after hypercalcemia is noted incidentally, but they may also present with vague symptoms of hypercalcemia (polydipsia, polyuria, malaise, constipation, neuropsychiatric changes) or with nephrolithiasis [1].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree