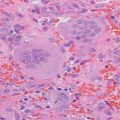
Fig. 4.1
Changes in lumbar spine BMD from baseline diagnosis of PHPT to before surgery 6 years later
A discussion of treatment options included parathyroidectomy versus observation, and the patient preferred medical observation.
Assessment and Diagnosis
PHPT has been associated with bone loss most notable in the cortical bone compared to cancellous bone [1, 2]. The prevalence of osteoporosis assessed by DXA in patients with PHPT has been found by Cipriani et al. to be close to 60 % with a prevalence of vertebral fracture of 35 % (study population with 91 % women and a mean age of 63 years) [3]. Conversely, the prevalence of PHPT in patients with osteoporosis has been reported between 0.5 and 6.1 % [4].
The identification of concomitant osteoporosis and PHPT is important since it may alter clinical management, as surgical correction of PHPT has been associated with improvement of BMD [5, 6].
Current clinical practice guidelines recommend DXA BMD evaluation in all patients with PHPT, as BMD results may change PHPT management toward surgery for potential skeletal benefits [5]. In a prospective study of patients with PHPT, only 14 % had a history of clinical fractures at baseline assessment but 60 % had osteoporosis based on DXA findings [3].
This DXA evaluation should include BMD measurement at the radius in addition to the spine and hips, as cortical (compact) bone is more susceptible than trabecular (cancellous) bone to the effects of PTH [2, 5].
The presence of osteoporosis (as defined by fragility fractures or a DXA T score ≤ −2.5) is a strong indication for surgical intervention in patients with PHPT. This recommendation is based on BMD improvement in patients that undergo surgical intervention [5, 7, 8].
In patients with PHPT who have a contraindication for surgery or who refuse surgical intervention, medical management is an alternative treatment [5, 9]. Most commonly, bisphosphonates are the treatment of choice based upon clinical studies showing improvement of BMD, although data regarding fracture outcomes are lacking [9]. A meta-analysis of patients with PHPT and calcium levels <12 mg/dL reported improved BMD at the lumbar spine and femoral neck in patients treated with surgery or bisphosphonates, without significant change in forearm BMD [7, 9]. In the studies that assessed BMD without PHPT intervention, decreased BMD was noted at the lumbar spine, femoral neck, and forearm at 2-year follow-up [7]. It is important to note that BMD change is only a surrogate marker for fracture outcome, for which clinical evidence is not available in patients with PHPT [7, 9].
There is no high-quality evidence available to be able to recommend when DXA BMD should be repeated after surgical intervention for PHPT. Studies have shown improvement in BMD between 12 and 36 months after surgical cure [10, 11]. A repeat BMD at 12–24-month follow-up is advised for patients who prefer observation or are receiving medical therapy [5].
Multiple localization techniques which help plan the surgical procedure are currently available. These studies should only be performed when surgery is a consideration, since the diagnosis of PHPT is based on biochemical evidence alone [5, 8].
Available localization techniques include neck ultrasound, sestamibi scintigraphy, computerized tomography (CT) scanning, magnetic resonance imaging (MRI), and catheter-based localization. Each of these modalities is associated with different advantages, disadvantages, costs and radiation dose. Overall, the sestamibi scan and neck ultrasound have sensitivities above 75 % and the four-dimensional CT (4D-CT) scan has a sensitivity of 89 %. The positive predictive value for each of these three techniques is above 90 % [12]. This highlights the point that the diagnosis of PHPT is a biochemical diagnosis. In addition, even when localization studies are used to help guide surgery, they might be negative in some cases.
There is a known relationship between dietary calcium intake and serum PTH levels that can have different effects on bone metabolism. There are concerns that reducing the calcium intake in patients with PHPT might lead to more pronounced stimulation of PTH secretion and a deleterious effect on bone; on the other hand, a reduced calcium intake might translate into decreased urinary calcium load and a lower risk of kidney stones [5]. A calcium food questionnaire study in 31 patients with asymptomatic PHPT found that calcium supplementation in subjects with a low dietary calcium intake (below 450 mg/day) resulted in a decrease in serum PTH (after 4 weeks) and improvement in BMD (at the end of 1-year follow-up) [13]. The present recommendation for calcium intake in patients with PHPT is the same as for patients without PHPT, due to lack of clinical evidence to the contrary [9, 13, 14].
Management
She received annual follow-up for 6 years by her primary care provider without any interim history for kidney stones, fractures, or worsening hypercalcemia. BMD during this time decreased at the lumbar spine by 13 % (T score −2.7) (Fig. 4.1), at the left hip by 5.6 % (T score −1.5), and at the right hip by 6.0 % (T score −1.4) (Fig. 4.2) with a significant decline in combined total hip BMD (Table 4.1). At her 6-year follow-up at age 51, she was referred for an endocrinology consultation. A right wrist BMD was also measured at this time and corresponded to a T score of −3.0 (Fig. 4.3). The potential benefits of surgical intervention to BMD and fracture risk were revisited, and a parathyroid scan (Fig. 4.4