Fig. 3.1
Clinical presentation of AC of the lower lip. Actinic cheilitis of lower vermilion characterized by blurring of the vermilion line, atrophy, dryness, red and white areas, crusting, and ulceration
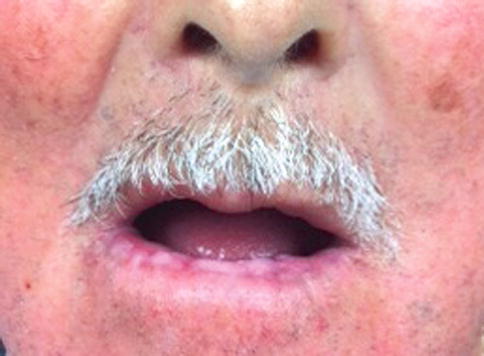
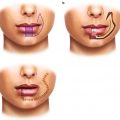
Fig. 3.2
Actinic cheilitis and generalized changes on the face due to chronic sun exposure
3.4 Histopathology
When evaluating clinical lesions, a clinician should not treat AC based on the clinical appearance because the clinical appearance may not indicate the true nature of the process. An incisional biopsy with histopathologic review is warranted to determine the extent of histopathologic changes, which may not be homogenous even in clinically homogenous areas. In larger lesions, multiple biopsies and serial sections might be necessary to ascertain the greatest degree of epithelial change [3].
Cheilitis has been described as having many characteristics. Typically, the epithelium is atrophic (thin and lacking rete ridges), hypertrophic (acanthotic, or thickened, with or without elongation of the rete ridges), ulcerative (partial or complete epithelial loss), or acantholytic (indicating desmosomal junctional disruption and suprabasilar separation of cells). Hyperkeratosis, either ortho- or parakeratosis, is reported to occur in a majority of the cases and give the clinical appearance of a scaly lesion. Solar elastosis, seen as basophilic connective tissue changes, is indicative of UVB damage to the collagen underlying the epithelium, and replacement by an amorphous material has been reported in some studies to occur in 100 % of the cases evaluated. Inflammation is also a predominant feature in the connective tissue, and in a majority of the cases that reported this feature, perivascular inflammation deeper in the tissue has also been noted. Vasodilation of superficial vessels is also a common finding [3, 9–11] (Figs. 3.3 and 3.4).
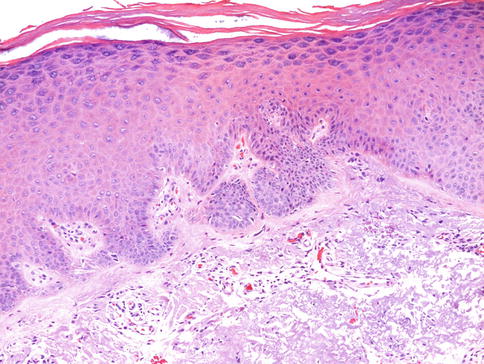
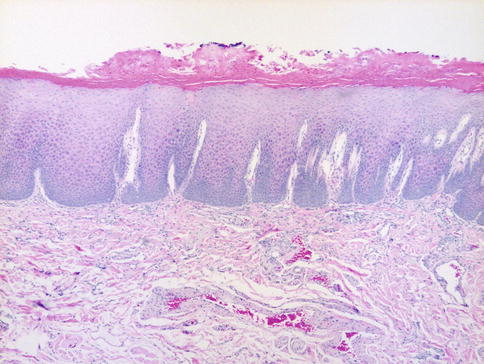
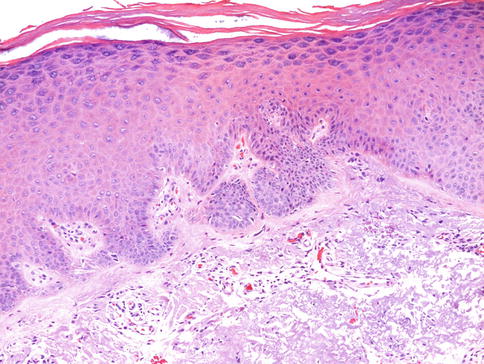
Fig. 3.3
Actinic cheilitis of labial vermilion exhibiting marked parakeratosis of the surface seen as crusting of the lip. The epithelial retia are elongated and exhibit dysplastic changes in the lower half of the epithelial thickness (moderate dysplasia). Dilated vascular channels are seen in the underlying connective tissue, which exhibits focal solar elastosis (H & E, 40×)
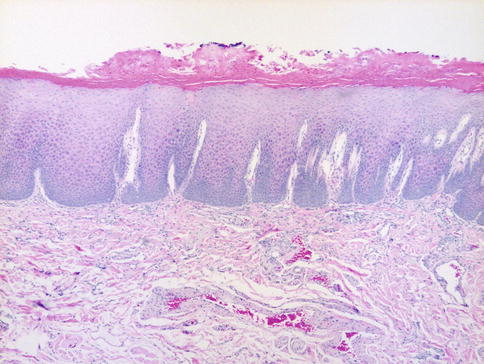
Fig. 3.4
Actinic cheilitis of labial vermilion showing marked orthokeratosis of the surface of the epithelium and dysplastic changes confined to the basal and parabasal cell layers (mild dysplasia). Dilated venules are seen in the underlying connective tissue which exhibits prominent solar elastosis exemplified as basophilic (bluish) change (H & E, 100×)
Dysplasia has been reported in up to 100 % of cases. As dysplasia is a requisite for the diagnosis of AC, this seems reasonable. In a large study that reviewed 152 cases of AC, mild dysplasia was present in 52 %, moderate dysplasia in 24 %, severe dysplasia in 13 %, and carcinoma in situ in 11 %. Similar to dysplasia of the oral mucosa, the degree of epithelial dysplasia can only be a predictor of chance of malignant transformation, rather than a direct indicator of malignant potential. Interestingly, the degree of inflammation seen is directly correlated with the degree of dysplasia, which may indicate an innate immunologic response to the epithelial changes [3, 9–11].
3.5 Treatment
Given the positive relationship of sun exposure and UV radiation to the development of AC, application of lip balm with anti-UVA and anti-UVB ingredients, such as para-aminobenzoic acid (PABA), or sun-blocking agents, such as zinc oxide or titanium dioxide, should be applied for protection when exposure is expected. Once changes do occur, application may aid in the prevention of further damage.
Once biopsy has determined the extent of microscopic change, complete removal is indicated. Many treatment options for AC have been studied and have shown to have varying degrees of efficacy.
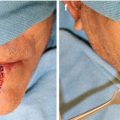
The gold standard of treatment for AC is vermilionectomy. This procedure involves full-thickness surgical resection of the epithelium. Vermilionectomy is very operator dependent owing to the difficulty in scalpel incisions and closure. Simple vermilionectomy involves removal to the level of the orbicularis oris. A modified technique includes removal of minor salivary glands and muscle. Labial mucosa is advanced forward to replace the excised vermilion. Complications of this procedure include hematoma, wound dehiscence, scarring, loss of normal lip contour, and paresthesia. A modified version of vermilionectomy is the W-plasty technique, which allows for better cosmetic healing. Studies show that ~93 % exhibited no or mild retraction upon healing with W-plasty as compared to 70 % of the classic technique exhibiting moderate to severe retraction. Regardless of the technique, vermilionectomy is extremely efficacious in the removal of AC. One further advantage of vermilionectomy to nonsurgical treatment is that it allows posttreatment histopathologic review and is beneficial in determining the extent of the disease process [8, 12].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree