© Springer International Publishing AG 2018
Philip T. Cagle, Timothy Craig Allen, Mary Beth Beasley, Lucian R. Chirieac, Sanja Dacic, Alain C. Borczuk, Keith M. Kerr, Lynette M. Sholl, Bryce Portier and Eric H. Bernicker (eds.)Precision Molecular Pathology of Lung CancerMolecular Pathology Libraryhttps://doi.org/10.1007/978-3-319-62941-4_11. Precision Medicine in Lung Cancer
(1)
Department of Pathology, Aberdeen University Medical School, Aberdeen Royal Infirmary, Foresterhill, Aberdeen, UK
(2)
Department of Pathology, Aberdeen Royal Infirmary, Foresterhill, Aberdeen, UK
Keywords
Lung cancerNSCLCPrecision medicinePersonalized medicineMolecular testingBiomarker testingImmunohistochemistryMutation testingExternal quality assuranceThis textbook discusses in considerable detail the molecular landscape of lung cancer and how the molecular biology of the tumour is involved in the evolution, growth and development of the disease. Huge advances in our knowledge have been made in recent years, thanks in part to technology allowing whole exome and even whole genome sequencing. Apart from elucidating the molecular basis of this most fatal of malignant diseases, the molecular features of lung cancer can also be exploited therapeutically. Pathologists have known for a very long time about how different individual tumours can be from each other; to a large extent, we now understand that this morphological variation is a reflection of molecular heterogeneity. The development of so-called molecularly targeted drugs, and a realization that these drugs do not work for every patient, rapidly led to the need to select patients, often based on their molecular characteristics, to ensure a higher chance of therapy response. This idea of precision or personalized medicine is of course, not new. The concept of selective toxicity was pioneered decades ago [1] and has been a familiar practice in medicine, treating infections with antibiotics based upon sensitivity testing. In oncology, one of the first tumour types to have a precision medicine approach, selecting patients for therapy based upon pathological characteristics, was breast cancer. Oestrogen and progestogen receptor testing for tamoxifen therapy and, later, HER2 testing for trastuzumab therapy are well established in clinical practice. Precision medicine and personalized therapy in lung cancer is a more recent development, but this has developed into an extremely diverse and complex branch of oncology, bringing considerable benefits for groups of patients, multiple choices for oncologists and considerable demands on pathologists.
Precision Medicine: Impact on Lung Cancer Therapy
In the 1980s cytotoxic agents were used in some patients with small cell lung cancer (SCLC). Systemic chemotherapy , different from that used in small cell carcinoma, was introduced into routine practice as a palliative measure in advanced non-small cell lung cancer (NSCLC ) in the early 1990s. Thus, one could argue that the earliest selection of patients with lung cancer was based upon this paradigm of treating advanced small cell lung cancer in one way, and all other lung cancer by other means. Prior to the introduction of such systemic therapy, lung cancer treatment was based upon surgery and radiotherapy for localized disease and best supportive case (basically no active, cancer-directed treatment) for advanced disease. This rather crude discrimination actually spawned the concept of ‘non-small cell carcinoma’ as a so-called entity , a therapeutic grouping of convenience, which lumped together a group of pathologically and biologically very different diseases because they were all treated in the same way. Multiple cytotoxic chemotherapeutic regimens were developed which improved overall survival in advanced NSCLC to perhaps 6–8 months from diagnosis, but by around 2005, it was felt that a plateau had been reached; various cytotoxic therapy approaches all delivered more or less the same, limited efficacy [2].
Progress in treatment of SCLC has been very limited. Platinum-etoposide-based regimens have been the mainstay of treating this disease for many years. There have been very few signs of success in targeted therapy, and there are none in routine clinical use. The genetics of SCLC are described elsewhere in this book. Genomic studies of SCLC have failed to identify any promising drug targets [3]. One interesting recent development, however, is the exploitation of DLL3 expression on the surface of SCLC cells. An antibody against DLL3 is used as a means to selectively target SCLC cells expressing this marker and deliver an antibody-conjugated cytotoxic agent in patients who express high levels of DLL3 on their tumour, as assessed by a specific anti-DLL3 immunohistochemistry (IHC) assa y [4].
Between 2004 and 2008, two therapeutic developments began a significant change towards precision medicine in advanced NSCLC. The anti-angiogenic agent bevacizumab demonstrated an increased risk of fatal haemorrhage in patients with squamous cell carcinoma, but not in adenocarcinoma where survival benefits were demonstrated in combination with platinum-doublet chemotherapy [5, 6]. The drug was approved only for patients with ‘non-squamous’ NSCLC. A pemetrexed-platinum doublet showed superior outcomes when compared to gemcitabine-platinum in adenocarcinoma and undifferentiated tumours; the drug label for pemetrexed required a diagnosis of adenocarcinoma or large cell carcinoma [7]. These events were the catalyst for the drive towards specific NSCLC subtyping in advanced disease small diagnostic samples and an attempt to eradicate the term NSCLC-NOS (not otherwise specified). This is discussed below and in Chap. 5.
Trials of inhibitors of the epidermal growth factor receptor (EGFR) tyrosine kinase (TKI) began to be reported around 2000, with mixed results, but with the observation that certain patients did spectacularly well on these therapies. These patients tended to be younger, never-smoking females of East Asian ethnicity with advanced adenocarcinoma. It was discovered that these patients who responded particularly well to EGFR TKIs had tumours which bore mutations in the tyrosine kinase domain of the EGFR gene [8, 9] and there followed a series of successful trials demonstrating clear clinical benefit for EGFR TKIs in patients with a range of EGFR mutations in exons 18–21 [10–13]. This underpinned the need for EGFR mutation testing to select patients for EGFR TKI therapy, now a routine practice and standard of care.
The EGFR story highlighted the importance of identifying cancers driven by so-called addictive oncogenic changes [14]. Addictive oncogenes make excellent drug targets and provide biomarkers which are highly predictive of therapy response. The next to be discovered in NSCLC was a group of rearrangements involving the anaplastic lymphoma kinase (ALK) gene and a number of gene partners, leading to activation of the ALK gene tyrosine kinase [15]. The ALK TKI crizotinib rapidly proved its worth in treating patients with adenocarcinomas bearing ALK rearrangements [16–18]. There are now several other ALK TKIs at various stages in the trial regulatory process. Several other apparently addictive oncogenic changes have been discovered in lung adenocarcinomas which are variably associated with, but not exclusive to, the same patient demographic as for EGFR-mutated tumours. Essentially, this reflects an adenocarcinoma phenotype whose genesis is unknown; other than that tobacco carcinogens are not involved. ROS proto-oncogene 1 (ROS1) gene rearrangements are also associated with this adenocarcinoma phenotype, and crizotinib is now approved in many countries for the treatment of patients with such rearrangements [19–22]. RET proto-oncogene (RET) and neurotrophic receptor tyrosine kinase 1 (NTRK1) gene rearrangements and B-raf proto-oncogene (BRAF V600E) and erb-b2 receptor tyrosine kinase 2 (HER2) mutations account for small groups of adenocarcinoma patients with drugs undergoing trials [19–22]. BRAF inhibitors will probably be the first in this latter group to gain regulatory approval. MET proto-oncogene (MET) exon 14 skipping mutations are a promising target found in a number of NSCLC tumour types [23, 24].
The benefits to patients, of discovering therapeutically targetable molecular drivers in their tumours, and delivering the appropriate therapy, have been demonstrated [25]. The benefit is a real, treatment-related effect, rather than a prognostic effect related to the molecular alteration. The use of EGFR and ALK TKIs is now regarded as standard of care in those molecularly defined groups of patients, treatment for ROS1 rearrangements is similarly regarded in many countries and as more drugs gain regulatory approval, so practice will change as newly introduced therapies are incorporated into treatment guidelines for advance stage NSCLC [26, 27]. Immunotherapy, specifically through the use of anti-PD1 and anti-PD-L1 immune checkpoint inhibitors , is rapidly becoming established in the treatment of advanced NSCLC, and with some of these drugs comes the need for biomarker-based patient selection. This matter is discussed in some detail in Chap. 20. All of these developments reflect the remarkable success or personalized, precision medicine for patients with lung cancer. Almost all of the recently approved treatments, which are largely responsible for overall survival for advanced NSCLC extending out to beyond 12 months, are prescribed on the basis of a biomarker test. These advances have also transformed the diagnostic pathways for lung cancer, presenting exciting new opportunities and challenges in equal measure, for pathologists dealing with these cases.
Precision Medicine: Impact on Lung Cancer Pathology
Diagnostic Complexity
The development of lung cancer therapies specifically targeting pathologically and/or molecularly defined subsets of patients, as described above, has had an enormous impact on the diagnostic process required for cases of lung cancer, especially in the setting of advanced disease [28–31].
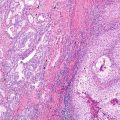
The diagnostic journey begins with the identification of carcinoma in the submitted sample. As discussed below, and in Chap. 5, most diagnostic samples from lung cancer patients provide only very limited amounts of tumour. Through dialogue with colleagues, discussion at the tumour board or multidisciplinary team (MDT) meeting and what should be regarded as mandatory clinical information provided with the samples sent for diagnosis, the pathologist should be aware of the likelihood of a diagnosis of primary lung cancer or any possibility of metastases to the lung. Separation of SCLC from other tumour types is followed by the subtyping of NSCLC cases as accurately as possible. IHC now plays a pivotal role in this process, as discussed in Chap. 5. It is imperative that IHC is carried out only when required. If the diagnosis of adenocarcinoma or squamous cell carcinoma can be made by morphology alone, usually so in 60–75% of cases in small sample diagnosis, IHC should not be carried out to confirm tumour subtype. IHC should only be used in those cases which the pathologist would morphologically classify as NSCLC-NOS. In a case of adenocarcinoma, clinical details should drive any IHC-based investigation of possible primary sites other than lung. There is evidence that pathologists overuse IHC in the small sample diagnosis of lung cancer and thus waste precious tissue, compromising the subsequent molecular testing in appropriate cases [32].
Current guidelines recommend that cases of possible, probable or definite adenocarcinoma should be submitted for molecular testing [33, 34], as these are the samples most likely to bear a targetable molecular alteration. Rare cases of squamous cell or small cell carcinoma in never or long-time ex-smokers should also be tested. As more molecular targets are defined, with approved drugs being made available, it may be justifiable to test all patients with NSCLC, using multiplex testing approaches such as next-generation sequencing (NGS) [35–37]. Currently, however, this broad approach is not financially justifiable, based on the limited number of drugs available in most health systems, and the very strong bias of current targets to an adenocarcinoma phenotype. In an academic setting, a more broad approach, such as testing for multiple targets to select patients for clinical trials, is rapidly becoming common practice [36]; drug availability is the most important driver of testing practice, and this is highly variable from a global perspective.
Tissue Handling
Lung cancer patients mostly present with advanced, metastatic disease and are suitable for only palliative systemic therapy, if any treatment at all. A significant proportion of lung cancer patients are too unwell, either for investigation and tissue confirmation of their disease or systemic therapy. Practice varies, but 15–25% of patients with a clinical diagnosis of lung cancer are unfit for, or refuse, further investigation. If patients do have a tissue diagnosis of their tumour, this will usually be based upon a small tissue biopsy or a cytology sample taken from a site or sites deemed most easily accessible. As a consequence of limited accessibility due to disease location and patient comorbidities, lung cancer samples are almost universally small and contain relatively little tumour [38]. It is therefore essential that these samples are handled with great care, without waste and in ways that facilitate the possible extensive biomarker investigation that may be required once the complete histological diagnosis is achieved.
Tissue samples have to be fixed and processed before sections can be made for staining and examination. Although certain types of biomarker testing may be favoured by different fixation and processing methods, a sample can only be fixed and processed once, and that has to be suitable for all of the possible testing approaches that may be required. Thus, standard fixation using 10% neutral buffered formalin is recommended, and tissue should be fixed for between 6 and 72 h. Outside this window, DNA damage and protein epitope alterations may occur [39]. We have also learned that some IHC epitopes are not well preserved by alcohol fixation, and very short fixation times, which may help preserve DNA, can lead to poor IHC performance.
A conservative approach to the use of IHC in the initial diagnostic phase has already been emphasised. Biomarker testing in lung cancer is now pursued along two separate methodological lines. Some tissue from the formalin-fixed, paraffin-embedded tissue block is used for DNA and, perhaps, RNA extraction. Tissue sections are also required for morphology-based tests such as predictive IHC-based biomarker testing or biomarkers based upon in situ hybridization. For the latter, fluorescence methods (FISH) are more often used than bright field approaches such as chromogenic or silver-precipitant (CISH or SISH) methodology.
For samples where a possible lung cancer diagnosis is likely (various thoracic samples in a relevant clinical context), block cutting strategies can be employed to limit the number of times a block is (re)cut, as this wastes tissue on each occasion. Extra tissue sections taken up front, in anticipation of need, can be used as required for deeper sections, IHC, FISH, etc. It would be rare for laboratories to be able to take sections for molecular analysis in this way, as those sections are normally made separately on a molecularly sterile instrument. These strategies certainly help maximize the use of very limited tissue resources [40].
Genes Versus Proteins
A central tenant in molecular biology is the transcription of DNA to produce mRNA message that is translated into protein. In cells, proteins are the active, effector molecules, encoded by genes. Proteins drive oncogenic events and are also the targets of drugs. Depending on the molecular abnormality being targeted by a drug, it may make more sense to use DNA, for example, for mutation testing, whilst some biomarker tests, for example, PD-L1, directly target the protein itself. Testing lung cancer samples for ALK gene rearrangements has been approached in many different ways [40]. The change in the DNA sequence signalling the rearrangement can be sought at the DNA level by FISH or next-generation sequencing approaches; unique mRNA transcripts can be looked for or elevated levels of ALK protein demonstrated by IHC. Each approach appears to predict for therapeutic response. It is likely that ROS1 rearrangement testing will also develop in a similar way. Diagnostic practice is driven partly by evidence for the most efficacious approach, but also by perceptions about which is the easiest, quickest and cheapest method. Simple, low-cost, rapid testing is always attractive, but it may not necessarily provide the best answers, and pathologists need to be careful not to move their testing approaches too far away from what was validated in clinical drug trials; otherwise, patient selection may become inaccurate and inefficient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree