Soft tissue sarcomas are rare cancers. They should be managed by a multidisciplinary team with experience caring for these diverse malignancies. Local control is frequently achieved with a combination of radiation therapy and surgery. This article reviews the data supporting the role of adjuvant radiotherapy in the care of patients with soft tissue sarcoma and describes the side effects of surgery and radiation therapy. Preoperative radiation therapy increases the risk of wound complication from surgery, but has fewer long-term side effects than postoperative radiation therapy. The timing of radiation therapy can be tailored to each patient.
Key points
- •
Sarcomas should be managed by a multidisciplinary team with experience in caring for patients with sarcoma.
- •
Surgery is the cornerstone for management, but many patients with sarcoma are treated with adjuvant radiation therapy to improve local control.
- •
Preoperative and postoperative radiation therapy have similar rates of local control, but different side effect profiles. Therefore, combining radiation therapy with surgery should be tailored to each patient.
Introduction
Sarcomas encompass a diverse array of malignancies that originate in the musculoskeletal system. The cell of origin is most often muscle, fat, or bone. Overall, there are approximately 10,000 of these malignancies diagnosed in the United States annually. Most occur in an extremity (50%). Other major sites are the retroperitoneum, trunk, and head and neck regions.
This article focuses on the use of radiation therapy for adult-type soft tissue sarcomas. Special mention is made of other sarcomas (eg, the management of retroperitoneal sarcoma) where appropriate. Although this article focuses on the use of radiotherapy, emphasis is placed on the multidisciplinary management of these malignancies.
Introduction
Sarcomas encompass a diverse array of malignancies that originate in the musculoskeletal system. The cell of origin is most often muscle, fat, or bone. Overall, there are approximately 10,000 of these malignancies diagnosed in the United States annually. Most occur in an extremity (50%). Other major sites are the retroperitoneum, trunk, and head and neck regions.
This article focuses on the use of radiation therapy for adult-type soft tissue sarcomas. Special mention is made of other sarcomas (eg, the management of retroperitoneal sarcoma) where appropriate. Although this article focuses on the use of radiotherapy, emphasis is placed on the multidisciplinary management of these malignancies.
Importance of multidisciplinary evaluation
Because of the rarity and marked heterogeneity of soft tissue sarcomas, it is crucial that patients be evaluated in centers with clinical expertise. The heterogeneity of histologic subtypes and varied clinical presentations observed require treatment plans that are ideally discussed and formulated in the context of a multidisciplinary setting. Pathologic expertise is essential in making an initial diagnosis. Radiologic evaluation is appropriate for adequate and complete staging. Discussion between the radiologist and surgeon additionally provides for a carefully planned surgical approach, allowing a determination of the proximity of disease to vital neurovascular and visceral structures. In addition, an open dialogue among the treating surgeons and medical and radiation oncologists allows timely consensus regarding the need, timing, and sequence of respective therapies in an effort to limit treatment-related morbidity while maintaining functional outcomes and performance status. Plastic and reconstructive and vascular surgical specialties may be used in specific scenarios. In addition, the evaluation and management of patients in a center with expertise may provide a sense of patient comfort and reduced anxiety in knowing that providers have experience and a working knowledge of an otherwise rare disease.
Staging work-up
The American Joint Committee on Cancer (AJCC) 7th Edition (2010) staging for sarcoma is now used. For soft tissue sarcoma, not only are tumor size, lymph node status, and distant metastatic status integral to staging but tumor grade is also incorporated in the system. All grade 1 tumors are considered stage I given their low risk of malignancy-related death. All metastatic tumors are stage IV. Stage III tumors are considered to be those greater than 5 cm and grade 3, or those with involved lymph nodes. The remainder are considered stage II.
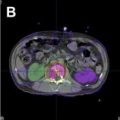
The staging of individuals diagnosed with sarcoma requires adequate imaging not only of the primary site but also as an assessment for disseminated disease. A determination of tumor size, relationship to fascial planes, proximity to vital structures, and presence or absence of metastasis all aid in determining an optimal treatment plan for patients. Magnetic resonance imaging (MRI) is the preferred imaging for sarcomas of the extremity, whereas computed tomography (CT) may be appropriate for retroperitoneal and truncal sarcomas. Adequate imaging of the chest is essential because the lungs are the most common site for distant spread. Staging should be individualized based on histologic subtype because some histologic subtypes show varying patterns of metastasis. Cross-axial imaging of the abdomen and pelvis should additionally be considered for histologies prone to abdominal spread, including leiomyosarcoma, epithelioid sarcoma, angiosarcoma, and myxoid round cell liposarcoma. Myxoid round cell liposarcoma has additionally been associated with spinal metastasis, whereas alveolar soft part sarcoma has been associated with the development of brain metastasis. Positron emission tomography/CT may additionally be considered and has both prognostic and predictive abilities.
Individuals with localized or locally advanced disease (stage I–III) are often treated with multimodality therapies, primarily surgery with additional consideration for radiation and/or chemotherapy as part of a neoadjuvant or adjuvant approach. Individuals with disseminated disease (stage IV) are traditionally treated with palliative systemic therapies, although the degree of disease burden, particularly in the setting of oligometastatic disease, may warrant aggressive treatment approaches, including metastasectomy.
Surgical considerations
Role of Biopsy
The primary focus of the orthopedic oncologist is the execution of an operative plan that resects the tumor and a surrounding margin of normal tissue while preserving or reconstructing as much functional tissue as possible. Before the widespread use of adjuvant radiation therapy, radical resections and amputations were common. The recognition that a limb-sparing resection plus adjuvant radiation therapy offered an equivalent outcome to amputation represented a landmark shift in the management of patients with soft tissue sarcoma of the extremity. Therefore, the importance of a multidisciplinary team approach to treating patients with soft tissue sarcoma cannot be overstated. The critical first step in planning this treatment is the biopsy. Because normal tissue encountered during biopsy potentially becomes contaminated by neoplastic cells, definitive resections are performed so that all tissue contacted by biopsy instruments is included in the resection and the radiation field, which means that a biopsy tract or incision that passes outside the planned surgical field requires a more extensive resection and a wider radiation field, and incurs additional morbidity to the patient. Although many types of biopsy are possible (typically either a core needle biopsy or an incisional biopsy), all biopsies should be planned with the definitive resection in mind. To that end, an important consideration for the diagnostician is whether or not an unknown soft tissue tumor may be a sarcoma. Referral to an orthopedic oncologist for a planned biopsy should be considered for any soft tissue tumor that has one or more of the following: (1) size greater than 5 cm, (2) location deep to fascia, and (3) heterogeneous signal intensity on MRI. By planning the radiation therapy, the biopsy, and the definitive resection together, radiation oncologists and orthopedic oncologists are able to optimize the treatment plan for the greatest chance of successful limb preservation.
Surgical Margins
Because sarcomas often grow along fascial planes, the battle for local control seems to begin and end with a wide resection. However, such resections, where a surrounding margin of normal tissue is removed along with the tumor, are not definitive without adjuvant therapy. Patients treated with a negative-margin excision and no adjuvant radiation therapy might be expected to have local control of their disease. In reality, they experience rates of local recurrence of up to 40%. It is now accepted that cancer cells are commonly found beyond the boundaries of the sarcoma pseudocapsule, but no one has been able to show a correct amount of normal tissue that should be resected to remove all cancer present, in part because of the difficulty of determining where these satellite cells are found relative to the tumor. One author has shown cancer cells in the supposedly normal tissue peripheral to the tumor in two-thirds of cases. In this study, cells were found up to 4 cm beyond the pseudocapsule of the tumor. There was no correlation between the presence of cancer beyond the pseudocapsule and signal changes on the MR imaging. It is this uncertainty about when and where cancer is located beyond the pseudocapsule and even beyond the surgical margins that may explain the benefit of adjuvant radiation therapy in obtaining local control. The presence of residual sarcoma cells in the tumor bed is associated not only with local recurrence but also with decreased disease-specific survival. With adjuvant radiation therapy, whether administered preoperatively or postoperatively, rates of local recurrence decrease from nearly 40% to approximately 10%. Even when adjuvant radiation therapy is not part of the initial treatment plan, it should be elected to treat patients with unplanned positive margins identified on histopathology after resection.
The concept of the planned positive margin has been made possible by the use of adjuvant radiation therapy. A planned positive margin describes a situation in which the surgeon anticipates and executes a margin-positive resection to spare a critical structure (typically a nerve, vessel, or bone) adjacent to a tumor. Provided that the structure is not fixed to the tumor and that adjuvant radiation therapy is used, this carefully planned and anticipated margin-positive situation provides similar outcomes to margin-negative controls.
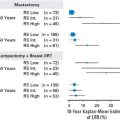
Evidence for the use of radiotherapy in sarcoma management
Classic studies from the 1970s and 1980s established the role of radiotherapy in the management of extremity sarcomas. A randomized trial at the National Cancer Institute comparing amputation versus limb-sparing surgery followed by radiotherapy showed similar overall survival rates with an acceptable local recurrence rate in the surgery and radiotherapy arm (15%). The benefit of radiation therapy in addition to limb-sparing surgery was evaluated in a second National Cancer Institute study that randomized patients with extremity sarcoma to a compartmental resection versus tumor resection followed by radiotherapy. The surgery alone arm had a lower local control rate (80% vs 100%) and again overall survival was not affected. Another prospective, randomized trial at Memorial Sloan Kettering Cancer Center compared limb-sparing surgery alone versus surgery plus brachytherapy. The addition of brachytherapy increased the rate of local control from 69% to 82%.
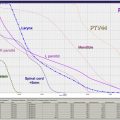
The seminal contemporary contribution to this area is the randomized study of preoperative versus postoperative radiotherapy conducted by the National Cancer Institute of Canada (NCIC). The radiotherapy techniques consisted of 50 Gy in the preoperative setting and 66 Gy given postoperatively. Longitudinal expansions around the tumor were 5 cm and radial expansions were 2 cm. The local control rate (90%) and overall survival were similar. There was a doubling (35% vs 17%) of the wound complications within 120 days after surgery in preoperative versus postoperative radiotherapy arms. However, these wound complications were predominantly in the lower extremity. Moreover, long-term complications such as fibrosis, edema, and joint stiffness seemed to be decreased in the preoperative radiotherapy arm.
Therefore, the body of randomized data suggests that radiotherapy in combination with tumor resection provides excellent local control at the primary site. The optimal timing of radiotherapy (preoperative or postoperative) can be influenced by individual factors such as overall life expectancy of the patient and therefore the concern regarding long-term complications, and the underlying risk and potential complications from a wound infection (eg, vascular disease or uncontrolled diabetes).
Radiation therapy for unresected sarcomas
As described in detail earlier, surgery is the foundation of local therapy for sarcomas. However, there are clinical scenarios in which surgery is not an option. In some cases, patient comorbidities may make certain surgeries too risky. In other cases, en bloc surgical resection may cause such significant morbidity that patients decline surgery. In these cases, the multidisciplinary team needs to consider creative options to try to achieve local control. In these situations, radiation therapy alone can be considered. In contrast with the radiation doses used in preoperative (50 Gy) or postoperative (60 Gy) radiation therapy, to achieve local control with radiation therapy alone, a higher dose of radiation is generally required for most soft tissue sarcomas.
The sarcoma group at the Massachusetts General Hospital reported the outcome of 112 patients whose unresected soft tissue sarcomas were treated with radiation therapy. At the time of the analysis, median follow-up was 139 months. Tumor size at the time of radiation therapy and radiation therapy dose influenced local control. Local control at 5 years for sarcomas less than 5 cm, 5 cm to 10 cm, and greater than 10 cm was 51%, 45%, and 9%, respectively. Five-year local control for tumors treated with less than 63 Gy was 22%, whereas 5-year local control was 60% for tumors treated to doses of 63 Gy or greater. Use of chemotherapy, histologic grade, and tumor location did not influence the results of this retrospective study. Fourteen percent of all patients had a major complication from radiation therapy. The complication rate from radiotherapy increased to 27% for patients treated with at least 68 Gy. Although these results of radiotherapy for the treatment of unresected soft tissue sarcomas are inferior to the combination of surgery and adjuvant radiation therapy, they show that radiation therapy alone with a dose of at least 63 Gy can achieve local control in approximately half of all soft tissue sarcomas up to 10 cm in size. Therefore, for select patients who are unable or unwilling to undergo surgery, radiation therapy alone or with concurrent ifosfamide chemotherapy should be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree