Popliteal Resections
Amir Sternheim
Yair Gortzak
Jacob Bickels
BACKGROUND
Soft tissue sarcomas of the popliteal fossa are rare, accounting for less than 5% of all soft tissue sarcomas of the extremities. Surgery in this anatomic area is challenging: Performing a wide resection with negative surgical margins is often difficult because of the periarticular location and the proximity to neurovascular structures.3,7,10
Such tumors formerly were treated with amputations4; however, better understanding of tumor biology and advances in chemotherapy and radiation therapy now allow limb-sparing procedures to be performed in most of these cases.
ANATOMY
The popliteal space is diamond-shaped; on its superior aspect, it is bounded by the semimembranosus and semitendinosus muscles medially and by the biceps femoris muscle laterally. Its inferior boundaries are the two heads of the gastrocnemius muscle. The roof of the fossa is the thin popliteal fascia; the floor is the posterior aspect of the distal end of the femur, the posterior capsule of the joint, and the popliteus muscle, which overlies the proximal tibia.
The popliteal artery and vein enter the popliteal space from its medial aspect through the adductor hiatus and lie directly behind the posterior capsule of the knee joint.
They run obliquely through the fossa and branch into two superior, a single middle, and two inferior genicular branches. After exiting the popliteal fossa, the popliteal artery divides into its terminal branches: the anterior tibial, posterior tibial, and peroneal arteries. The popliteal vein lies between the tibial nerve and the popliteal artery. The short saphenous vein pierces the popliteal fascia to join the popliteal vein within the fossa.
The tibial nerve enters the popliteal fossa lateral to the popliteal artery and approximately in the middle of the fossa. It crosses the artery to its medial aspect and remains at that location. The common peroneal nerve slopes down the superolateral border of the popliteal fossa toward the medial aspect and along the biceps femoris tendon, where it enters a tunnel within the substance of the peroneus longus muscle.
IMAGING AND OTHER STAGING STUDIES
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is the imaging modality of choice for the diagnosis of popliteal soft tissue sarcomas. The typical finding is a soft tissue mass with a solid component, no communication to the knee, and central or irregular nodular gadolinium enhancement. Conversely, the classic presentation on MRI of popliteal cysts, which are the most frequently encountered masses in the popliteal fossa, is a well-defined, unilocular, fluid-filled cyst in direct communication with the knee joint; its peripheral walls are normally enhanced with gadolinium.
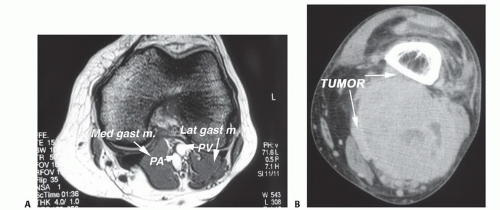
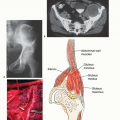
MRI is also used to evaluate the size of the tumor and its relation to the neurovascular structures, the posterior knee joint capsule, and surrounding musculature and to assess local lymph node involvement (FIG 1A-C).
Plain Radiography and Computed Tomography
Plain radiography and computed tomography (CT) scans are performed to rule out invasion of the tumor into the adjacent bones.
Angiography
Angiography (FIG 1D-E) is routinely used to assess the relation of the tumor to the popliteal artery, patterns of possible vascular displacement, the presence of vascular anomalies, and arterial and venous patency.
SURGICAL MANAGEMENT
Positioning
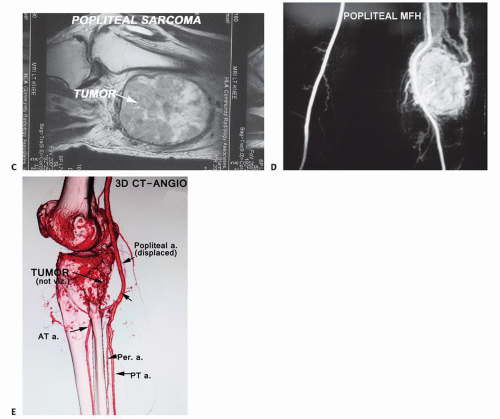
The patient is placed in the prone position (FIG 2) and both lower limbs are draped.
The contralateral leg is prepared for saphenous vein harvesting, which will be necessary for arterial reconstruction if the popliteal artery must be resected.
TECHNIQUES
▪ Exposure
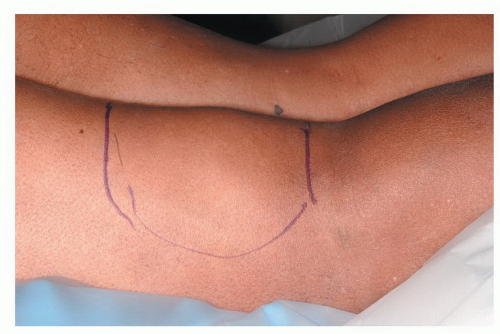
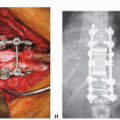
An S-shaped incision is made, crossing from proximal-medial to distal-lateral at the level of the knee joint (TECH FIG 1A). The medial-proximal arm of the incision allows the popliteal vessels to be identified as they exit the adductor hiatus, and the lateral distal arm enables easy exposure of the peroneal nerve, posterior to the fibular head. In addition, making the distal arm of the incision lateral avoids damaging the greater saphenous vein, which runs on the medial aspect of the leg (TECH FIG 1B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree