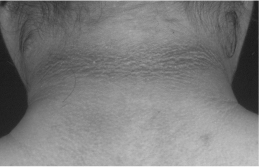
Figure 22.2 Acanthosis nigricans in a patient with polycystic ovary syndrome.
Investigations
- A pregnancy test should be done in all women who have missed an expected menstrual period.
- Luteinizing hormone (LH): high serum LH levels (due to an increased frequency and amplitude of the LH pulse) and a high (>3) ratio of LH to follicle-stimulating hormone (FSH) are seen in many women with PCOS. However, these are not part of the diagnostic criteria for PCOS. Serum LH levels are affected by the timing of the blood sample relative to the last menstrual period.
- FSH: serum FSH levels should be measured to rule out ‘ premature ovarian failure’ (see Chapter 21).
- Androgens: testosterone, androstenedione and dehydroepiandrosterone sulphate (DHEA-S) are usually raised in PCOS. The excess androgens can be derived from the ovary, the adrenal cortex or both. It is important to check androgen levels to screen for androgen-secreting ovarian and adrenal tumours (see below).
- Sex hormone-binding globulin (SHBG): elevated insulin levels and androgen levels both inhibit the hepatic production of SHBG. Lower SHBG levels (seen in about 50% of patients) result in an increase in circulating free androgens.
Exclude other causes of menstrual irregularity or hyperandrogenism by performing the following tests:
- Hyperprolactinaemia: serum prolactin.
- Hypo/hyperthyroidism: free thyroxine and thyroid-stimulating hormone.
- Congenital adrenal hyperplasia: 17-hydroxyprogesterone (9 a.m., follicular phase).
- Cushing’s syndrome (only if there is a high clinical suspicion of Cushing’s syndrome): two or three 24-hour urine collections for free cortisol measurement or an overnight dexamethasone suppression test.
- Androgen-secreting ovarian or adrenal tumours: serum testosterone levels are nearly always higher than 5.2 nmol/L. Those with adrenal tumours usually have serum DHEA-S levels above 21 μ mol/L. Their serum LH levels are low.
About 8% of hyperandrogenic patients have no identified cause despite thorough investigation and are said to have idiopathic hyperandrogenaemia.
Look for impaired glucose tolerance/diabetes mellitus. About 45% of patients with PCOS have impaired glucose tolerance or type 2 diabetes mellitus. Ideally, an oral glucose tolerance test (OGTT) should be performed in all patients. If this is not practical, a fasting glucose and glycated haemoglobin level should be done. If either one is abnormal, an OGTT should be performed to distinguish between impaired glucose tolerance and diabetes mellitus. A fasting lipid profile should also be requested in all women with PCOS.
Figure 22.3 Ovarian ultrasound in a patient with polycystic ovary syndrome.

Ultrasound
The presence of 12 or more follicles in each ovary measuring 2–9 mm, and/or an increased ovarian volume of more than 10 mL (calculated by the formula: 0.5 × length × width × thickness), is part of the Rotterdam criteria for the diagnosis of PCOS (Fig. 22.3). Ovarian ultrasound may show increased ovarian stroma. The transvaginal approach should be used. However, these ultrasonographic criteria may be difficult to document if an experienced ultrasonographer is not available.
Treatment
The management of PCOS depends on the patient’s symptoms (hirsutism, oligomenorrhoea, obesity, glucose intolerance) and goals (e.g. desire to become pregnant).
Hirsutism
Oral contraceptive pills
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








