C7. Platelet abnormalities in the neonate and childhood
Thrombocytopenia
Most infants with thrombocytopenia come to the attention of the neonatologist because of haemorrhagic symptoms: petechiae, purpura, epistaxis or mucous membrane bleeding.
Mechanisms of thrombocytopenia in neonates and children fall into two basic categories:
• Increased destruction
• Impaired or ineffective thrombopoiesis.
Thrombocytopenia due to increased destruction
Idiopathic thrombocytopenic purpura (ITP)
ITP is one of the most frequently seen examples of increased platelet destruction. A typical history is bruising and petechiae appearing suddenly in a child who is otherwise in excellent health. The peak age for the diagnosis of ITP is 2 to 4 years. In childhood ITP, males and females are affected with equal frequency—in contrast to adult ITP, in which females dominate by a 3:1 ratio. Often there is a history of a viral illness or vaccination 1 to 3 weeks prior to presentation. The platelet count in these children is commonly <10 × 109/L. The blood film should be carefully scanned for the presence of reactive lymphocytes as well as large platelets when a case of ITP is suspected.
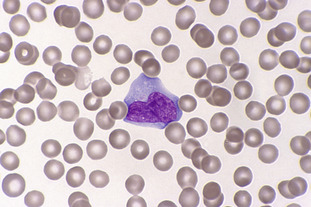
In the majority of cases, ITP in children is an acute self-limiting disease resolving within 6 months whether or not therapy is given. Refer to Fig C7-1.
Thrombocytopenia due to impaired or ineffective thrombopoiesis
Amegakaryocytic thrombocytopenia (AMEGA)
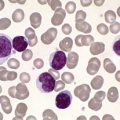
AMEGA occurs in infancy and early childhood. The mode of inheritance is either X-linked or autosomal-recessive. AMEGA is a very rare disorder in which patients present with a petechial rash, bruising or bleeding in the first year of life. Mild to moderate anaemia and leucopenia may be present. Megakaryocytes in the bone marrow are either reduced in number or absent. Granulopoiesis and erythropoiesis are normal. The red cells may be macrocytic and the HbF increased.
Between 20% and 40% of cases may develop aplastic anaemia in the first few years of life.
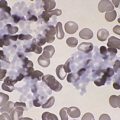
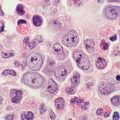
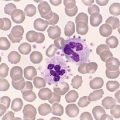
Patients with AMEGA have a predisposition to develop acute leukaemia. Refer to Figure C7-2 and Figure C7-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree